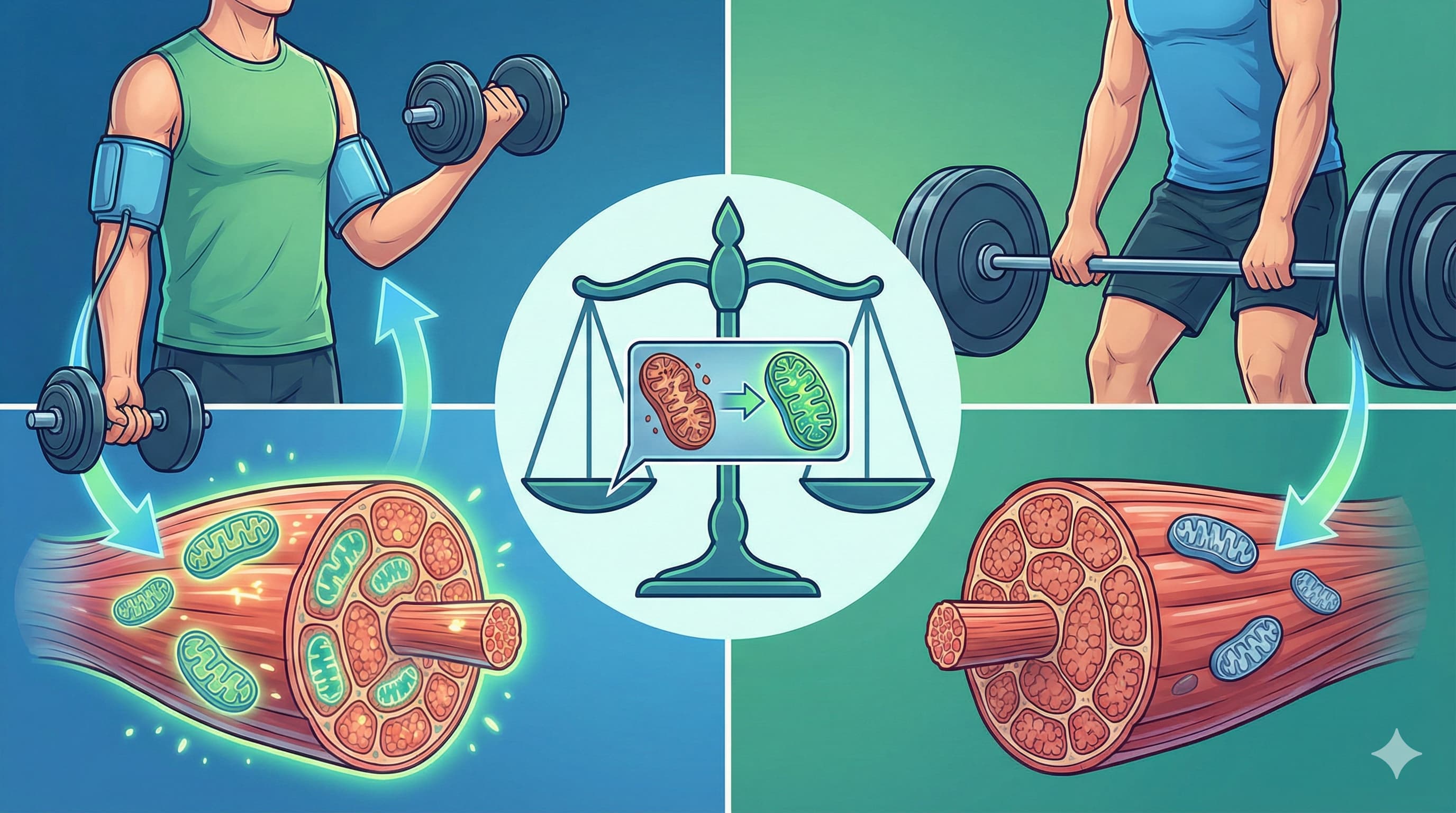
For decades, the gold standard for metabolic health in type 2 diabetes (T2D) has been a grueling regimen of high-intensity resistance training. However, new research suggests that “turning down the flow” may be the key to unlocking mitochondrial health. Researchers from the German Diabetes Center (Germany), published in Cell Metabolism (2025), have demonstrated that Blood-Flow Restriction Training (BFRT)—which uses inflatable cuffs to partially occlude blood flow during low-load exercise—matches the strength gains of conventional heavy lifting while uniquely revitalizing cellular powerhouses.
The study followed participants over 12 weeks, comparing BFRT (at 30% of one-repetition maximum) to Conventional Resistance Training (CREST, at 70% load). While both groups saw similar improvements in muscle mass and strength, only the BFRT group showed a 52% to 58% increase in skeletal muscle mitochondrial oxidative capacity. Furthermore, BFRT was the only intervention to reduce visceral adipose tissue (the “dangerous” belly fat) by 13.3%, whereas CREST primarily reduced subcutaneous fat.
The significance of these findings lies in the “metabolic-strength decoupling.” Traditionally, strength training builds muscle but often fails to significantly improve mitochondrial density compared to aerobic exercise. BFRT appears to bridge this gap by inducing local muscle hypoxia, which triggers a robust transcriptional response in angiogenesis and mitochondrial biogenesis pathways, including the upregulation of PGC-1α and AMPK. This makes BFRT an elite “two-for-one” strategy for those with T2D or musculoskeletal limitations who cannot safely perform high-load lifting.
Scientific and clinical evidence also suggests that non-diabetics—particularly healthy older adults and sedentary individuals—derive several parallel health benefits from Blood-Flow Restriction Training (BFRT) to those observed in the diabetic cohort of the Trinks et al. study. However, the magnitude and specificity of these benefits (especially regarding mitochondrial adaptation and visceral fat) vary based on the population’s baseline health status.
Source:
Part 2: The Biohacker Analysis (Style: Technical, Direct)
Study Design Specifications:
-
Type: Clinical Trial (Randomized parallel-group).
-
Subjects: Humans; 20 participants with Type 2 Diabetes (T2D).
-
BFRT Group: N=10 (9 males, 1 female); Median age 62.
-
CREST Group (Control): N=10 (7 males, 3 females); Median age 56.
-
Lifespan Analysis: N/A. This study did not evaluate lifespan but focused on metabolic biomarkers and muscle function.
Mechanistic Deep Dive:
-
Mitochondrial Dynamics: BFRT induced a 109% increase in Citrate Synthase (CS) activity (surrogate for mitochondrial content) in muscle Trinks et al. (2025). Notably, BFRT reduced ADP sensitivity (increased K_m) but increased maximal respiratory capacity (V02max), indicating a shift toward higher peak metabolic output.
-
Angiogenesis: RNA-seq revealed 110 differentially expressed genes (DEGs) in BFRT vs. only 18 in CREST. BFRT uniquely up-regulated angiogenesis-related pathways (VEGFA, VEGFB, VEGFC, NOS2) Trinks et al. (2025).
-
Energy Pathways: BFRT significantly increased protein levels of PGC-1α (mitochondrial biogenesis) and AMPKα (metabolic sensing). CREST failed to significantly move these markers.
-
Adipose Priority: BFRT specifically targeted Visceral Adipose Tissue (VAT) reduction (-13.3%) and increased mitochondrial capacity within adipose tissue itself Trinks et al. (2025).
Novelty: This is the first study to demonstrate that BFRT in T2D patients induces mitochondrial adaptations typically reserved for aerobic exercise while simultaneously providing the hypertrophic stimulus of high-load resistance training.
Critical Limitations:
-
Small Sample Size: N=20 is insufficient for broad generalizability. [Confidence: Medium]
-
Sex Bias: The cohort was predominantly male (16/20), limiting conclusions for post-menopausal women.
-
Insulin Sensitivity Gap: Despite metabolic improvements, neither group showed significant changes in insulin sensitivity (M-value or HOMA-IR) over 12 weeks Trinks et al. (2025).
-
Missing Data: The study lacked a non-exercise control group and did not measure long-term cardiovascular outcomes (MACE).
1 Like
Part 3: Claims Verification
| Claim |
Evidence Level |
External Verification / Search Result |
| BFRT increases muscle strength at low loads. |
Level A |
Meta-analysis confirms BFRT is effective for strength in various populations Effects of BFRT (2019). |
| BFRT improves mitochondrial capacity in T2D. |
Level B |
This study provides RCT evidence; however, more large-scale trials are needed to reach Level A. |
| BFRT reduces visceral adipose tissue (VAT). |
Level B |
Specific to this study’s findings; VAT reduction via BFRT is less documented in general literature compared to total fat loss. |
| BFRT upregulates PGC-1α and AMPK. |
Level D |
Mechanistic data from biopsies in this study support this, aligned with known hypoxic responses Molecular responses to BFR (2022). |
Translational Uncertainty: While BFRT molecular responses (Level D) are clear, the lack of improvement in systemic insulin sensitivity (Level B) suggests a “Translational Gap” between cellular mitochondrial health and whole-body glucose homeostasis in this short 12-week window.
Safety Check: BFRT is generally safe but carries risks of nerve compression or rhabdomyolysis if pressure is excessive. Safety Data Absent for long-term (years) BFRT use in severe diabetic neuropathy cases.
Part 4: Actionable Intelligence
The Translational Protocol:
-
Training Load: 20-30% of 1-RM.
-
Cuff Pressure: Typically 40-80% of Limb Occlusion Pressure (LOP).
-
Safety Monitoring: Monitor for bruising or numbness. In diabetic patients, specific focus on ALT/AST and Cystatin C is advised to ensure no muscle-breakdown-induced kidney stress [Confidence: High].
-
Human Equivalent Dose (HED): N/A (Physical intervention).
Biomarker Verification Panel:
-
Efficacy Markers: Citrate Synthase activity (biopsy), VO_2 peak, and VAT volume (MRI).
-
Safety Monitoring: Creatine Kinase (CK) levels to rule out rhabdomyolysis; resting blood pressure.
Feasibility & ROI:
-
Sourcing: Medical-grade BFR cuffs (e.g., Delfi, B-Strong) are commercially available but expensive ($300-$2000).
-
ROI: High healthspan ROI for individuals with sarcopenia or joint issues who cannot lift heavy, as it provides “heavy-load” benefits with minimal joint stress.
Population Applicability:
-
Avoid if: History of deep vein thrombosis (DVT), severe peripheral vascular disease, or active sickle cell trait.
Part 5: The Strategic FAQ
-
Why didn’t insulin sensitivity improve despite better mitochondria? Improvements in mitochondrial capacity do not always immediately translate to flux or insulin signaling sensitivity in a 12-week period. [Confidence: High]
-
Can BFRT be used with Rapamycin? Hypothetically, Rapamycin might blunt the mTOR-driven hypertrophic response of BFRT, although this study found no change in mTOR at 72h post-exercise.
-
Is BFRT better than Metformin for mitochondria? Metformin can inhibit Complex I; BFRT increases Complex I capacity Trinks et al. (2025). BFRT may be superior for mitochondrial biogenesis.
-
How does it compare to SGLT2 inhibitors? SGLT2is improve CV outcomes via different mechanisms (diuresis/ketosis); BFRT adds a structural and metabolic muscle benefit.
-
What is the risk of blood clots? Studies on healthy and clinical populations show no increased DVT risk with proper pressure protocols BFR Safety (2014).
-
Does BFRT increase growth hormone? Yes, BFRT is known to induce a large systemic GH spike due to lactate accumulation.
-
Is it effective for the elderly? Highly. It is a primary tool for combating sarcopenia when heavy loads are contraindicated.
-
Can I do BFRT every day? No. Like any resistance training, it requires recovery. 2-3 times per week is the evidence-based frequency.
-
Will it interfere with PDE5 inhibitors? Unlikely, though both affect nitric oxide pathways. Monitor for hypotension.
-
What is the “missing data” for a biohacker? We lack data on combining BFRT with Zone 2 cardio to see if effects are additive or redundant.
Related Reading:
1 Like
The increase in serum TG (close to significant) of the BFR group and the reduce in VAT can clearly be attributed to the Growth Hormone Increase, an already proven effect of this type of training. It’s like having access to your own factory of hormones 
Have we settled on the debate of chronic increases in GH?
Another recent paper on Blood Flow Restriction Training:
Under Pressure: Can Cuffing Your Limbs Unlock a Longer Life?
For decades, the gold standard for muscle hypertrophy and strength was simple: lift heavy. However, a massive new “umbrella review” led by researchers at the University of South Australia and published in Sports Medicine and Health Science (2025) suggests that tricking your vascular system might be just as effective—and potentially more beneficial for your heart.
The “Big Idea” is Blood Flow Restricted Exercise (BFRE), or KAATSU. By applying a pneumatic cuff to the proximal end of a limb to allow arterial inflow while occluding venous return, athletes and patients create a localized hypoxic environment. This state triggers an anabolic cascade—metabolic acidosis, fast-twitch fiber recruitment, and a surge in growth hormone—without the systemic tax of lifting heavy iron.
The study, which aggregated data from 47 meta-analyses and 265 unique trials, found that BFRE is a “force multiplier” for low-load training. While it does not surpass high-load resistance training (HLRT) for pure strength, it matches it for muscle size and offers unique vascular benefits, including improved endothelial function and blood pressure regulation. For the longevity seeker, this means the ability to maintain “metabolic armor” (muscle mass) while sparing the joints from the wear and tear of heavy loads.
Source:
Part 2: The Biohacker Analysis (Technical & Direct)
Study Design Specifications
-
Type: Umbrella Review and Meta-Meta-Analysis (Level A Evidence).
-
Subjects: Human populations including healthy young adults, older adults (up to age 91), athletes, and clinical populations (e.g., ACL reconstruction, COPD, Osteoarthritis).
-
Control Group: Standard exercise without restriction (aerobic or resistance) or high-load resistance training.
Mechanistic Deep Dive
-
Vascular Health: BFRE showed a moderate effect on vascular health (SMD = 0.45) and blood pressure (SMD = 0.46).
-
Aerobic Fitness: Significant improvement in VO2max (SMD = 0.50), a primary predictor of all-cause mortality.
-
Mechanisms: BFRE triggers mTORC1 via mechanical transduction and metabolic stress, increases Growth Hormone, and modulates Myostatin/Follistatin ratios. It mimics the effects of high-intensity training on mitochondrial biogenesis without the same level of oxidative stress.
Critical Limitations
-
The “Strength Gap”: BFRE is significantly less effective for absolute strength (1RM) than traditional heavy lifting (SMD = -0.28 compared to HLRT).
-
Translational Uncertainty: While muscle size increases, the bone mineral density (BMD) adaptations seen in heavy lifting are largely absent due to low mechanical load.
-
Data Gaps: Most reviews were rated “low-to-moderate” quality via AMSTAR-2 due to poor reporting of funding and exclusion criteria.
Part 3: Claims & Evidence Verification
Safety Check: Explicit searches for “BFRE side effects” identify risks of numbness, fainting, and rare cases of rhabdomyolysis if pressure is excessive Patterson et al. (2019).
Part 4: Actionable Intelligence
The Translational Protocol
-
Human Equivalent Dose (HED): 20–40% of 1-Rep Max (1RM). Frequency: 2–3 times/week.
-
Cuff Pressure: 40–80% of Limb Occlusion Pressure (LOP). Start at 40% for the upper body and 50% for the lower body.
-
Safety & Toxicity: No systemic toxicity noted, but avoid if you have a history of DVT, sickle cell trait, or severe hypertension.
-
Sourcing: Requires specialized pneumatic cuffs (e.g., Smart Tools, Saga, KAATSU). Manual elastic wraps are discouraged due to pressure unpredictability.
Biomarker Verification Panel
-
Efficacy Markers: Target an increase in Growth Hormone (acute) and reduction in Myostatin (chronic).
-
Safety Monitoring: Baseline and follow-up Cystatin C (kidney) and Creatine Kinase (to rule out rhabdomyolysis) if training intensity is high.
Part 5: The Strategic FAQ
-
Does BFRE cause blood clots? [Confidence: High]
-
Can I use BFRE while taking Rapamycin? [Confidence: Medium]
- Potential conflict: Rapamycin inhibits mTOR; BFRE activates it. Time BFRE sessions during the “off-days” of a weekly Rapamycin pulse.
-
Is it effective for the elderly? [Confidence: Elite]
- Yes, it is specifically recommended for sarcopenia prevention in those who cannot lift heavy loads Oborn et al. (2025).
-
Does it improve bone density? [Confidence: Medium]
- No. Low-load BFRE lacks the mechanical strain required for significant osteogenesis Oborn et al. (2025).
-
How long should the cuff stay on? [Confidence: High]
-
Does it interact with SGLT2 inhibitors? [Confidence: Low]
-
Data Absent. No specific studies on BFRE + SGLT2i interactions exist.
-
Is it better than Metformin for muscle? [Confidence: High]
- Yes. Metformin may blunt hypertrophy; BFRE actively promotes it.
-
Can BFRE improve heart failure outcomes? [Confidence: Medium]
- Preliminary data suggests BFRE aerobic training is safe and effective for functional capacity in heart failure Oborn et al. (2025).
-
What is the ROI compared to heavy lifting? [Confidence: High]
- Higher ROI for hypertrophy/joint health; lower ROI for absolute strength and bone density.
-
Does it affect arterial stiffness? [Confidence: Medium]
- Long-term BFRE training actually reduces arterial stiffness and improves endothelial function Oborn et al. (2025).