Glucose hyperglycemia caused by rapamycin is not related to insulin resistance but to hepatic glucose production, at least in my case study.
First here is my 24h average glucose level measured by CGM calibrated with finger glucose.
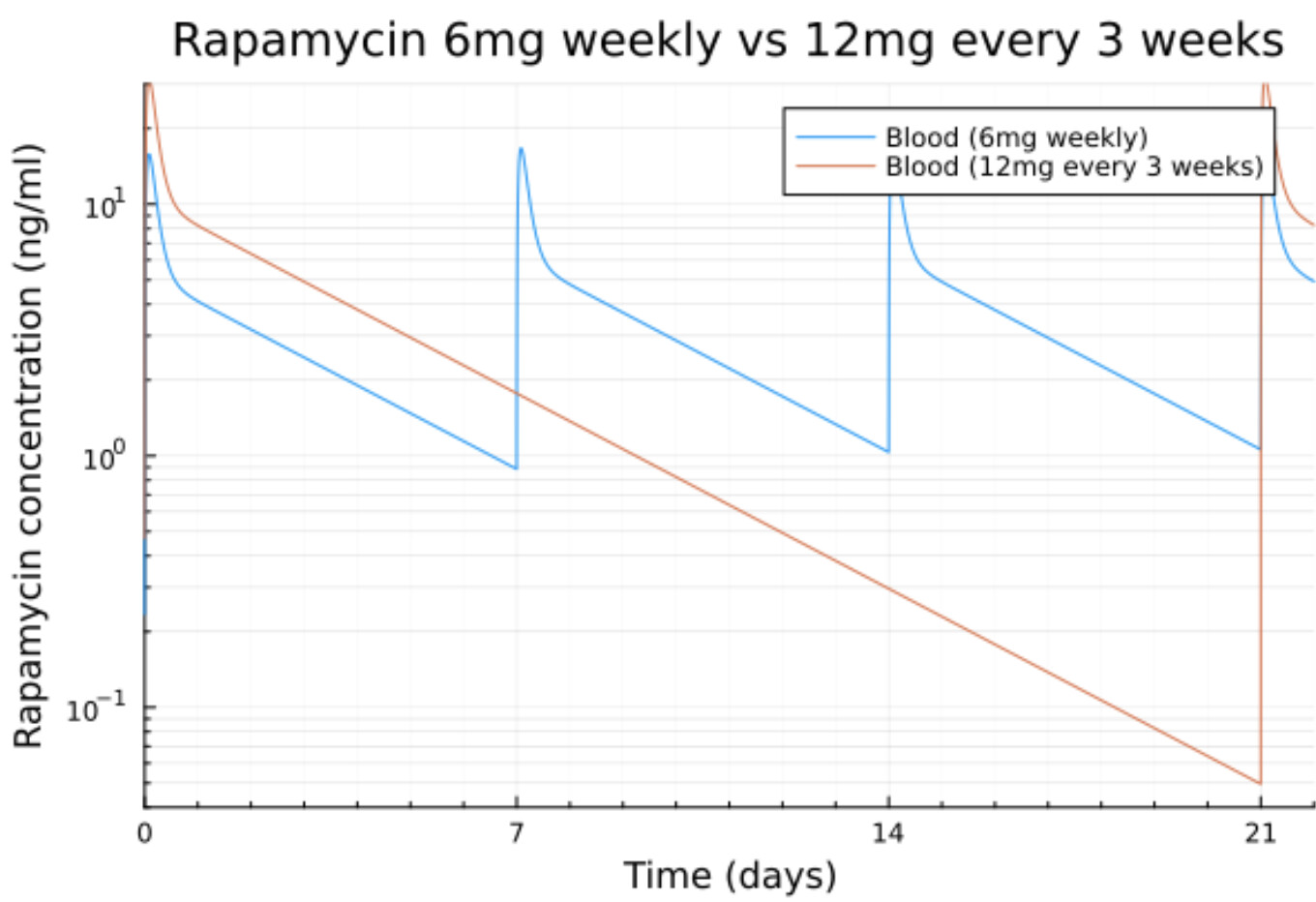
I was off rapamycin for a few months and restarted 12mg every other week in May.
The flat part are when I didn’t wear a CGM.
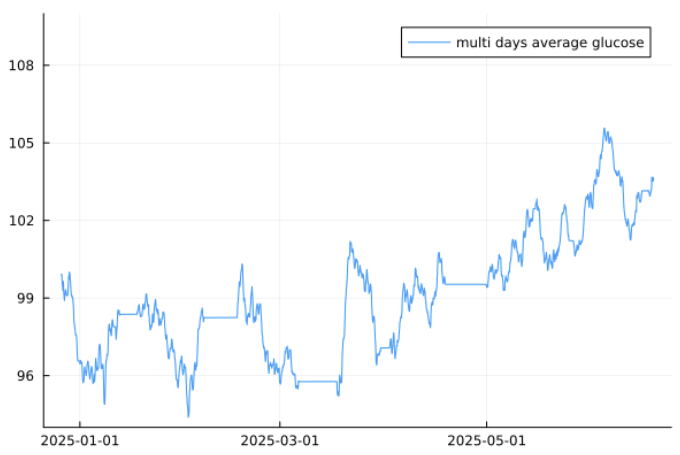
Clearly not good for sure.
BTW I’m taking a SGLT2i (empagliflozin 12.5mg/day then 25mg/day from May), Tirzepatide 4mg/week and Acarbose 100mg/meal.
All that did not prevent the glucose rise.
Then I did an Oral Glucose Tolerance Test (OGTT) which is ingesting a bolus of 75g of pure glucose in 300ml of water. That was a horrifying experience for somebody eating low carbs!
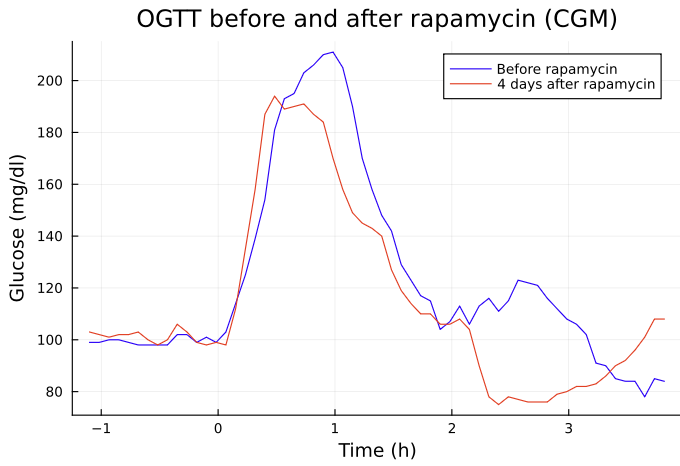
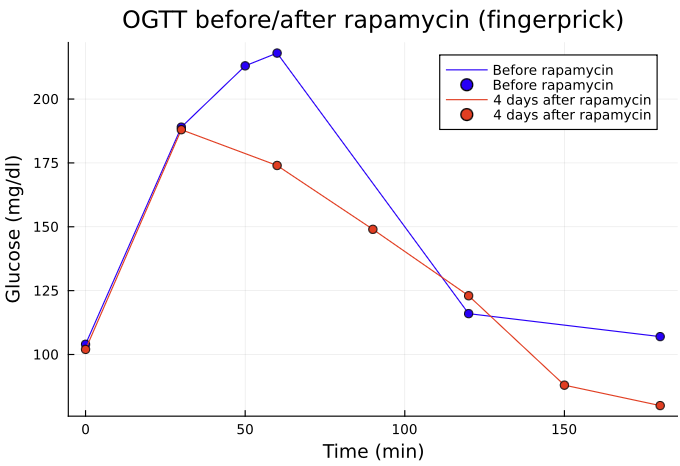
I was really surprised to see that it was better after rapamycin. I think the theory here is that as I eat low carbs, my pancreas is not used to such a large bolus of glucose and so the first OGTT primed it for the second one. In fact it’s recommended that low carbs [people eat at least 150g of glucose for 2 days before an OGTT.
My fasting insulin was 5.8 before rapamycin and 6.8 after which a rather mild increase.
Fasting glucose at the same time (7:30AM) was 99 then 97.
HOMA-IR went from 1.4 to 1.6 which is still OK.
Clearly rapamycin did not cause a high insulin resistance.
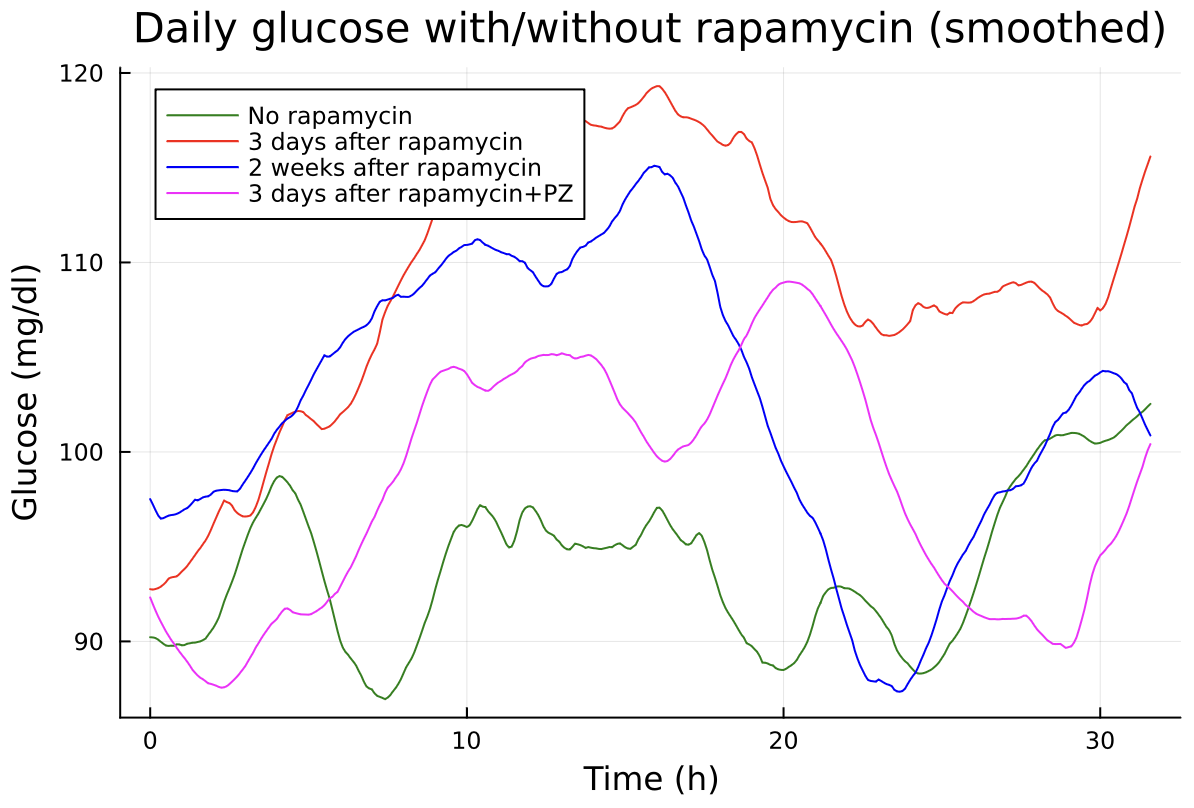
Let’s look at the liver glucose production below:
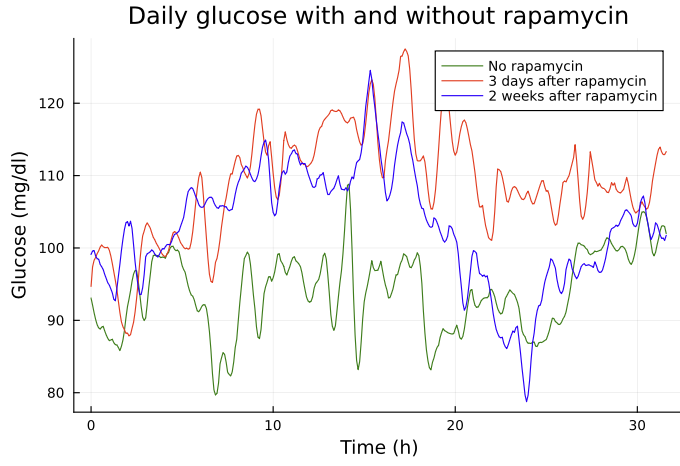
As it’s rather noisy with the peaks due to eating (noon and 6) and exercising (around 9~10) I used a low pass filter to smooth it:
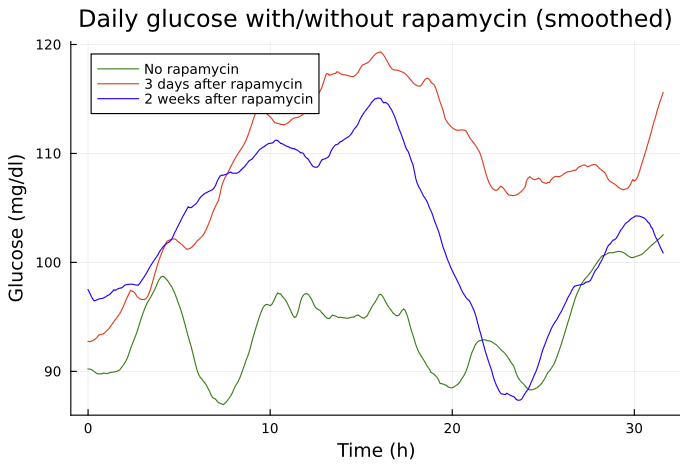
The green one is after 3 months without Rapamycin and stays below 100mg/dl on average which is rather good.
The green one is 3 days after rapamycin and clearly it’s very bad. It even stays above 105 mg/dl at night.
2 weeks after rapamycin there is some improvement but it’s still very bad.
We know there is no issue with the insulin resistance because the OGTT is completely OK so the glucose could go down. It’s really an issue with regulation here where the liver generates all that glucose independently of the meals.
Now after 3 weeks my hepatic glucose is around 105 during the day which is still not good.
All that with 25mg/day of Empagliflozin which makes me pee glucose like crazy (Checked with urine strips).