I recommend you to get on an oral MMP inhibitor like doxycycline, but you could also use topical ilomastat.
It’s kinda interesting that a synthetic MMP inhibitor like ilomastat is allowed in skincare products.
I recommend you to get on an oral MMP inhibitor like doxycycline, but you could also use topical ilomastat.
It’s kinda interesting that a synthetic MMP inhibitor like ilomastat is allowed in skincare products.
Pioglitazone improves the dermis in aging skin
The skin is one of the sensitive tissue in aging and age-related morphological changes of the skin were observed by HE staining. Morphometric analyses of images taken from light microscopy also be used to determine the thickness of various skin layers. The epidermal thickness was measured from stratum basale to stratum granulosum, whereas the dermal thickness was the distance between the epidermis and the subcutaneous adipose layer. We found that skin aging appearance such as disruption of the extracellular matrix in the dermis, wrinkling, and laxity of the skin were improved, especially the thickness of the skin in the aged apoE−/− mice was increased in the Piog group, compared with the vehicle group. Quantitative analysis of the skin thickness showed that the dermis containing collagen, elastic fibers, and hyaluronic acid was much thicker in the Piog group than that in the vehicle group (252.4 ± 37.0 μm versus 196.6 ± 24.1 μm, P < 0.01), even if the epidermis and adipose layer had no significant difference between two groups.
Fig. 4. Photomicrographs showing hematoxylin and eosin (HE) staining of mouse skin (A) and liver (C). Histogram showing the quantitative analysis of the thickness of various skin layers (B) and hepatic lipid content including total cholesterol (TC), free cholesterol (FC) and triglycerides (TG). The data were analyzed by t-test. *P < 0.05, **P < 0.01 vs. vehicle group.
ITP is currently testing pioglitazone, so they obviously think it has potential.
Progeria is a rare genetic disease that causes accelerated aging and death in children at a mean age of 13.5 years. An aminobisphosphonate-statin combination has been shown to reduce the toxicity of the mutated protein, progerin, in progeria patient cell cultures and in a mouse model of the disease. This combination is currently being tested in a European Therapeutic Trial for progeria in Marseille (ClinicalTrials.gov identifier NCT00731016). Progerin has been shown to be produced by skin cells during physiological aging. The objective of this study was to assess the efficiency of a new and original cosmetic formulation containing alendronate and pravastatin sodium salts, reduce crow’s feet wrinkles, and cheek hollow in a double blind, randomized and placebo controlled comparative study. Three cosmetic preparations were evaluated using FOITS: one containing sodium alendronate and sodium pravastatin, a placebo, and a commercial anti-aging product. Fifty-seven female and twenty-five male volunteers between 51 and 71-year-old were selected. Each subject tested two of the three products once a day, in the evening, by spreading each selected product on one side of the face. Skin micro-relief was analyzed at 0, 28, 56 and 84 days. Statistical analysis of 7 clinical qualitative (left or right side of face, gender, and 3 skin types) and 6 quantitative parameters (age, weight at each test time, wrinkle clinical grade at inclusion time) showed no statistical differences between the three tested products. In contrast, most of the 8 quantitative FOITS parameters describing skin micro-relief were statistically improved by the alendronate-pravastatin combination compared to the placebo or to the commercial anti-aging product. A cosmetic preparation containing alendronate and pravastatin sodium salts exhibited anti-aging effects by reducing crow’s feet wrinkles and restoring cheek volume.
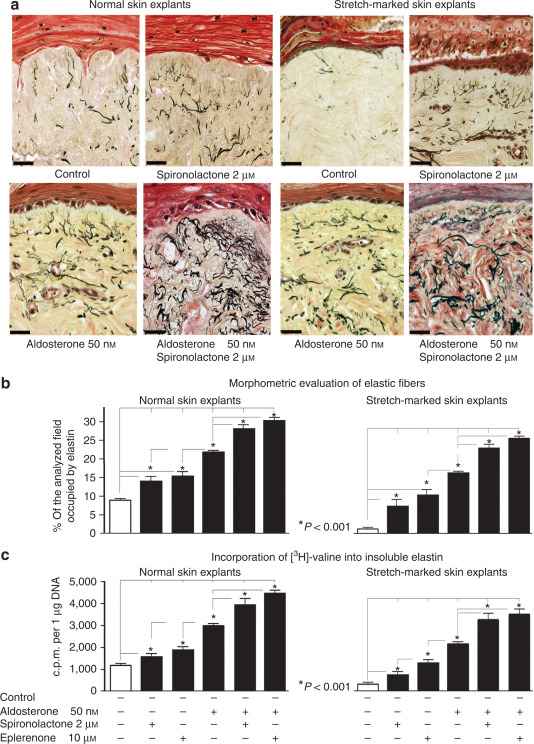
Human skin has been suggested as a new target for aldosterone because MR has been detected in the epidermis, in sweat and sebaceous glands, and in hair follicles. Targeted skin overexpression of MR in mice causes epidermal atrophy, premature skin barrier formation and alopecia. In this study, we have reported that MR is also present in human skin fibroblasts and that treatment of cultured fibroblasts with aldosterone in addition to induction of collagen type I production via MR activation induces an increase in elastin expression and consequent elastic fiber deposition in a MR-independent manner. We have also shown that blocking MR with spironolactone or eplerenone intensifies the elastogenic effect of aldosterone in dermal fibroblasts. To our knowledge these effects of aldosterone and MR-inhibitors have not been previously reported in skin. Although aldosterone has been shown to stimulate the production of other ECM components via cross-activation of glucocorticoid receptor, EGFR, angiotensin II type I receptor, and TGF-β1 receptors, we have shown that the beneficial elastogenic effect of aldosterone in the skin is solely executed via IGF-IR signaling.
The aim of the study was to assess an Ectoin formulation with regard to the antiageing properties. The study was designed as a monocentric, randomized, double-blind application test, in order to ensure the compatibility and the efficacy of Ectoin in comparison to a vehicle emulsion. A total of 104 voluntary healthy female test subjects were included in the study. Moisturizing properties as well as other parameters of skin ageing, like skin surface structure and skin elasticity, were determined for treatment A (vehicle) and treatment B (with 2% Ectoin) versus an untreated control. Statistical evaluations according to the Wilcoxon rank-sum test indicate a general preference for the Ectoin treatment by the test subjects in both the application and the efficacy tests. None of the participating test subjects had any side effects throughout the study. In terms of antiageing properties, previous in vitro studies could be confirmed by this clinical trial, clarifying that the natural cell protection concept of Ectoin is transferable to skin care with manifold benefits.
Introduction
Inflammatory skin diseases are a significant burden on affected patients. Inflammation is caused by various stress factors to the epidermis resulting in, e.g., dryness, redness, and pruritus. Emollients are used in basic therapy to restore the natural skin barrier and relieve symptoms. A systematic review was performed to evaluate the efficacy and safety of ectoine-containing topical formulations in inflammatory skin diseases characterized by an impaired skin barrier.
Results
A total of 230 references were screened for eligibility, of which six were selected for inclusion in the review (five studies on atopic dermatitis and one study on prevention and management of retinoid dermatitis). The application of topical formulations containing 5.5–7.0% ectoine positively influenced skin dryness and, consequently, pruritus and dermatitis-specific scores in patients with atopic dermatitis. Especially in infants and children, who belong to the most frequently affected group, the formulations were well-tolerated when applied for up to 4 weeks. In studies where ectoine was used as an adjuvant therapy, application was associated with a decreased need for pharmacological therapy and also improved the effectiveness of, e.g., topical corticosteroids. In patients undergoing isotretinoin therapy, ectoine was as effective as dexpanthenol in reducing retinoid dermatitis or improving symptoms.
Conclusion
Ectoine is an effective natural substance with an excellent tolerability and safety profile, representing a beneficial alternative as basic therapy or to increase the efficacy of the pharmacological treatment regimen for patients with inflammatory skin diseases, including infants and children.
Prolonged exposure to UV light can lead to photo-ageing of the skin. Therefore, the development and application of anti-photoaging drugs is urgent. In this study, we co-loaded apigenin (Apn) and doxycycline (Doc), a broad-spectrum inhibitor of matrix metalloproteinases (MMPs), into flexible liposomes to exert anti-photoaging effects by combating oxidative stress, anti-inflammation, reducing the activation of MMPs and preventing collagen loss. The results showed that we prepared a flexible liposome (A/D-FLip) containing Apn and Doc. Its appearance, particle size and Zeta potential were normal and it had good encapsulation efficiency, drug loading, in vitro release and transdermal efficiency. In cellular experiments, A/D-FLip could inhibit oxidative stress damage, reduce inflammatory factors and decrease the activation of MMPs in Human immortalized keratinocytes (HaCaT) cells; in animal experiments, A/D-FLip could inhibit skin damage and reduce skin collagen loss by decreasing the activation of MMPs, thus inhibiting skin photoaging in mice. In conclusion, A/D-FLip has good anti-photoaging effects and it has the potential to become an effective skin care product or drug against UV damage and skin photoaging in the future.
Purpose
The topical application of antioxidants has been shown to augment the skin’s innate antioxidant system and enhance photoprotection. A challenge of topical antioxidant formulation is stability and penetrability. The use of a targeted drug delivery system may improve the bioavailability and delivery of antioxidants. In this ex vivo study, we assessed the effects of the topical application of a liposome-encapsulated antioxidant complex versus a free antioxidant complex alone on skin photoaging parameters and penetrability in human skin explants.
Results
Compared to healthy skin, irradiated skin experienced increases in IL-6, IL-8 (p < 0.05), and MMP-9 (p < 0.05) secretion. After treatment with the encapsulated antioxidant complex, there was a 39.3% reduction in IL-6 secretion, 49.8% reduction in IL-8 (p < 0.05), and 38.5% reduction in MMP-9 (p < 0.05). After treatment with the free antioxidant complex, there were no significant differences in IL-6, IL-8, or MMP-9 secretion. Neither treatment group experienced significant LDH leakage or reductions in metabolic activity. Liposomes passed through the stratum corneum and into the epidermis.
Conclusion
The topical application of a liposome-encapsulated antioxidant complex containing ectoin, astaxanthin-rich microalgae Haematococcus pluvialis extract, and THDA improves penetrability and restored IL-6, IL-8, and MMP-9 levels in irradiated human skin explants, which was not seen in the comparator free antioxidant complex group.
Whereas the intrinsic aging is believed to occur similarly in different ethnic groups [2], there are well-known ethnic differences in extrinsic skin aging [102–104]. They show higher rates of these processes in Caucasians than in Asians [103,105], which was generally connected with different melanin content and composition in these ethnic groups [2]. For example, the middle-aged Caucasian women demonstrate a much higher appearance of wrinkles as the Asian women from the same age group [103]. Severe wrinkles on the upper lip were found in 38% and 10% of French and Japanese women aged between 50 and 64 years, respectively. Some types of wrinkles were shown to appear approximately 15 years earlier in French than in Japanese women [103]. Similar differences were observed between German and Japanese women [106]. If dermal adipocytes are involved in the skin aging processes, these differences should be at least partly connected with ethnic variations in dWAT content.
Irradiation of human adipose-derived stem cells (ADSCs) with UVA in vitro demonstrated suppression of adipogenic differentiation potential of these cells. Such suppression could be observed already by very low fluence of 0.05 J/cm2 and was gradually more severe as fluence increased up to 5.0 J/cm2 [41]. This effect was connected with an observed significant down-regulation of PPARγ expression caused by UVA and demonstrated strong dose- dependent effects. Accumulation of triglycerides in UVA-irradiated cells in this study was also significantly reduced in a dose-dependent manner. Taking into account that UVA of such low fluence as 0.05 J/cm2 was able to induce the pronounced effect on the ADSCs, we can assume that a direct effect of UVR on dermal adipocytes is possible, since such fluences can easily be realized in vivo in the lower dermis. Later, the same group has shown that UVA in similar doses also modulates the “stemness” of ADSCs [42].
These results demonstrate that adipocytes can react even to low doses of UVR with a suppression of PPARγ expression and adipogenic differentiation as well as with a reduced accumulation of triglycerides in mature adipocytes. This additionally supports the idea that not only systemic pathways, but also direct local responses in dWAT, can be involved in the reaction of sWAT to UVR in vivo, as observed in [37].
Ergothioneine, a sulfur-containing micromolecular histidine derivative, has attracted increasing attention from scholars since it was confirmed in the human body. In the human body, ergothioneine is transported and accumulated specifically through OCTN-1, especially in the mitochondria and nucleus, suggesting that it can target damaged cells and tissues as an antioxidant. It shows excellent antioxidant, anti-inflammatory effects, and anti-aging properties, and inhibits melanin production. It is a mega antioxidant that may participate in the antioxidant network system and promote the reducing glutathione regeneration cycle. This review summarizes studies on the antioxidant effects of ergothioneine on various free radicals in vitro to date and systematically introduces its biological activities and potential mechanisms, mostly in dermatology. Additionally, the application of ergothioneine in cosmetics is briefly summarized. Lastly, we propose some problems that require solutions to understand the mechanism of action of ergothioneine. We believe that ergothioneine has good prospects in the food and cosmetics industries, and can thus meet some needs of the health and beauty industry.
Damage to this skin barrier function can lead to skin diseases or infections, such as atopic dermatitis (AD) and acne. Rizzo et al. [100] demonstrated that the p53 family p63 might be key in driving AD. Moreover, p53 affects cell proliferation and differentiation by regulating RUNX1, which is generally detected in the nucleus of epidermal cells but is not significantly expressed in patients with AD [101]. This may suggest that it is related to the reconstruction of the skin structure and the repair of the skin barrier.
Interestingly, OCTN-1 expression was strongly correlated (score = 0.999) with RUNX1 gene expression, reflected in the STITCH database, as shown in Figure 5. Moreover, a study has demonstrated that EGT has a positive effect on immune system diseases caused by abnormal RUNX1 expression such as rheumatoid arthritis (RA) [102,103,104] and non-alcoholic fatty liver disease [12]. Additionally, RUNX1 expression—similar to that of p63 and p53—can directly regulate the process of cell proliferation and differentiation and is also a vital regulatory factor for normal hematopoiesis in the body, which may be consistent with the result that the blood contains high concentrations of EGT [101]. Moreover, it is a key regulator of normal hematopoiesis in the body [105], which may be consistent with the abundant accumulation of EGT in blood [15]. Furthermore, the regulatory effect of RUNX1 on SLC22A4 and the activation effect of ROS on p53 may suggest that EGT is transported to clear excess ROS through the high expression of OCTN-1 or that the anti-inflammatory effect of inhibiting IL-33 alleviates AD after the skin barrier function is impaired. This may lead to the downregulation of the IL-33-mediated inflammatory markers (loricrin, keratin 1, and keratin 10) [106]. Overall, these findings suggest that EGT may play a significant role in remodeling skin barrier function and treating AD.
Figure 4. EGT potentially regulates RUNX1 via the protective skin barrier. Additionally, EGT can potentially downregulate the inflammatory factor IL-33 induced by MAPK kinase, reduce the production of inflammatory markers (loricrin, keratin 1, and keratin 10), and indirectly regulate apoptosis caused by p53/63 by inhibiting the excessive increase in ROS. Interestingly, EGT and RUNX1 protein expression induce a strong binding energy related to the proliferation and differentiation of keratinocytes or skin stem cells, and ultimately promote the renewal of skin barrier function.
Figure 5. Prediction of EGT binding with related proteins by STITCH database cluster analysis.
We document CDKis expression in vivo during hair follicle stem cell (HFSC) homeostasis and find p21 (cyclin-dependent kinase inhibitor 1a, Cdkn1a), p57, and p15 up-regulated at quiescence onset. p21 appears important for HFSC timely onset of quiescence. Conversely, we find that Runx1 (runt related transcription factor 1), which is known for promoting HFSC proliferation, represses p21, p27, p57, and p15 transcription in HFSC in vivo. Intriguingly, in cell culture, tumors, and normal homeostasis, Runx1 and p21 interplay modulates proliferation in opposing directions under the different conditions.

Of course it takes 3 years. He uses a testosterone ester of some kind. Does anybody know anything about this? He says he’s not selling anything, but it really seems like he’s selling something.
There’s an Ergothioneine skin serum available on Amazon. Will be trying it for a month.
Luteolin belongs to the group of flavonoids and can be found in flowers, herbs, vegetables and spices. It plays an important role in defending plants, for example against UV radiation by partially absorbing UVA and UVB radiation. Thus, luteolin can also decrease adverse photobiological effects in the skin by acting as a first line of defense. Furthermore, anti-oxidative and anti-inflammatory activities of luteolin were described on keratinocytes and fibroblasts as well as on several immune cells (e.g., macrophages, mast cell, neutrophils, dendritic cells and T cells). Luteolin can suppress proinflammatory mediators (e.g., IL-1β, IL-6, IL-8, IL-17, IL-22, TNF-α and COX-2) and regulate various signaling pathway (e.g., the NF-κB, JAK-STAT as well as TLR signaling pathway). In this way, luteolin modulates many inflammatory processes of the skin. The present review summarizes the recent in vitro and in vivo research on luteolin in the field of skin aging and skin cancer, wound healing as well as inflammatory skin diseases, including psoriasis, contact dermatitis and atopic dermatitis. In conclusion, luteolin might be a promising molecule for the development of topic formulations and systemic agents against inflammatory skin diseases.
https://sci-hub.se/downloads/2021-05-13//41/gendrisch2020.pdf?download=true
For each patient, the study lasted 90 days, with three assessments: (1) D0 ‒ Inclusion, AK count on each forearm, Forearm Photoaging Scale (FPS) and AK severity score(AKSS); (2) D14 ‒ assessment of tolerability and adverse effects; (3) D90 ‒ AK count, FPS and AKSS.
The FPS is a validated scale that measures the degree of aging of the forearms through the number of superficial and hypertrophic AK, quantity and severity of wrinkles, solar lentigines, visible purpura, stellar atrophic scars, elastosis, and loss of elasticity. Each criterion has a weight and, at the end of the evaluation, the values are added together, resulting in a number that varies from 0 to 192.
Regarding treatment of forearm photoaging, 5-FU has been previously shown to improve the visual appearance of the skin, in addition to increasing the expression of pro-collagen I in the evaluation carried out six months after treatment.27 Both treatments investigated in the present study led to improvement in FPS. This result makes one reflect on whether COL could also bring benefits in photoaging treatment, raising the importance of studies with a design dedicated to elucidating this issue.
Background/purpose: Changes in humidity are commonly known to influence the condition of the skin. Previous studies of the skin dealt with variations in relative humidity (RH) either through statistical analysis or by maintaining room humidity at a constant level; however, the range of humidity and the length of acclimation varied in each study. This study aimed to determine whether the generally used ranges of RH are truly acceptable for studies of human skin.
Methods: Skin conductance, elasticity and fine wrinkles were assessed on the eyelids of 20 volunteers, first after acclimation for 30 min in a high-humidity room (70% RH) and again after acclimation for 30 min in a low-humidity room (40% RH).
Results: The study found significant decreases in skin conductance and elasticity and significant increases in fine wrinkles after acclimation to low humidity compared with high humidity.
Conclusion: These results indicate that even a 30% difference in RH can affect skin properties in 30 min. The importance of humidity stabilization and the necessity of acclimation to the humidity, particularly when the study concerns wrinkles, were thus confirmed.
I think skin is a big extra cellular matrix issue. The question is the extent to which cells can maintain the ECM. I think properly functioning cells are good at maintaining the ECM.
I am not a fan of botox as that is just damaging cells in order to create a cosmetic change. However, using exogenous tools to improve the ECM such as creams seems reasonable. Underlying this, however, if the cells are not functioning properly the ECM will not be fixed. Also collagen and hyaluronic is probably worth supplementing to make the job of the cells easier.
The last time (which was the only time) when I had Botox done was 20 + years ago. My eyebrows dropped and I didn’t want to try again. I remember I was told by a dermatologist that if I don’t do it, in some 5 years if not earlier my face will be all wrinkly. It turned to be not true, as I still almost wrinkle free at age 69. Go figure out.
While it might even be true, and I don’t know if it is, the trend of using Botox as a preventative drives me up a wall. We have a generation of perfect looking people in their 20’s spending all their money on this when they can’t even pay their bills.
Brows drop due to the skill of the injector … but you obviously don’t need it, so no reason to change!!!
FYI, Nira is having a sitewide 30% off promotion for their 5-year anniversary. I just ordered a Nira Pro Laser. Offer ends in 2 days. They have a 90-day money-back guarantee (less return shipping cost).
Background
Facial aging is a complex process influenced by environmental factors, genetics, and lifestyle. The contribution of the skin microbiota to this process remains poorly understood.Methods
This two-sample Mendelian randomization (MR) study was performed using genome-wide genotype data from the UK Biobank and previously published studies on skin microbiota. The primary approach for MR analyses included inverse-variance weighting (IVW), MR-Egger regression, simple mode, weighted median, and weighted mode methods. Sensitivity analyses were performed to assess heterogeneity and pleiotropy, and reverse-direction MR analyses were performed to evaluate potential reverse causation.Results
The MR analysis identified ten skin microbiotas with potential causal relationships with facial aging. Protective skin microbiotas included Genus Finegoldia, ASV011 [Staphylococcus (unc.)], ASV008 [Staphylococcus (unc.)], phylum Firmicutes, Family Rhodobacteraceae, and ASV021 [Micrococcus (unc.)], which were negatively associated with facial aging. Conversely, Order Pseudomonadales, Family Moraxellaceae, ASV039 [Acinetobacter (unc.)], and phylum Bacteroidetes were positively associated with facial aging, indicating a risk factor for accelerated aging. Sensitivity analyses confirmed the robustness of these findings, and reverse-direction MR analyses did not suggest any reverse causation.Conclusion
This study identified specific skin microbial that may influence facial aging and offered new insights into the rejuvenation strategies.