The Hemodynamic and Systemic Efficacy of Enhanced External Counterpulsation (EECP)
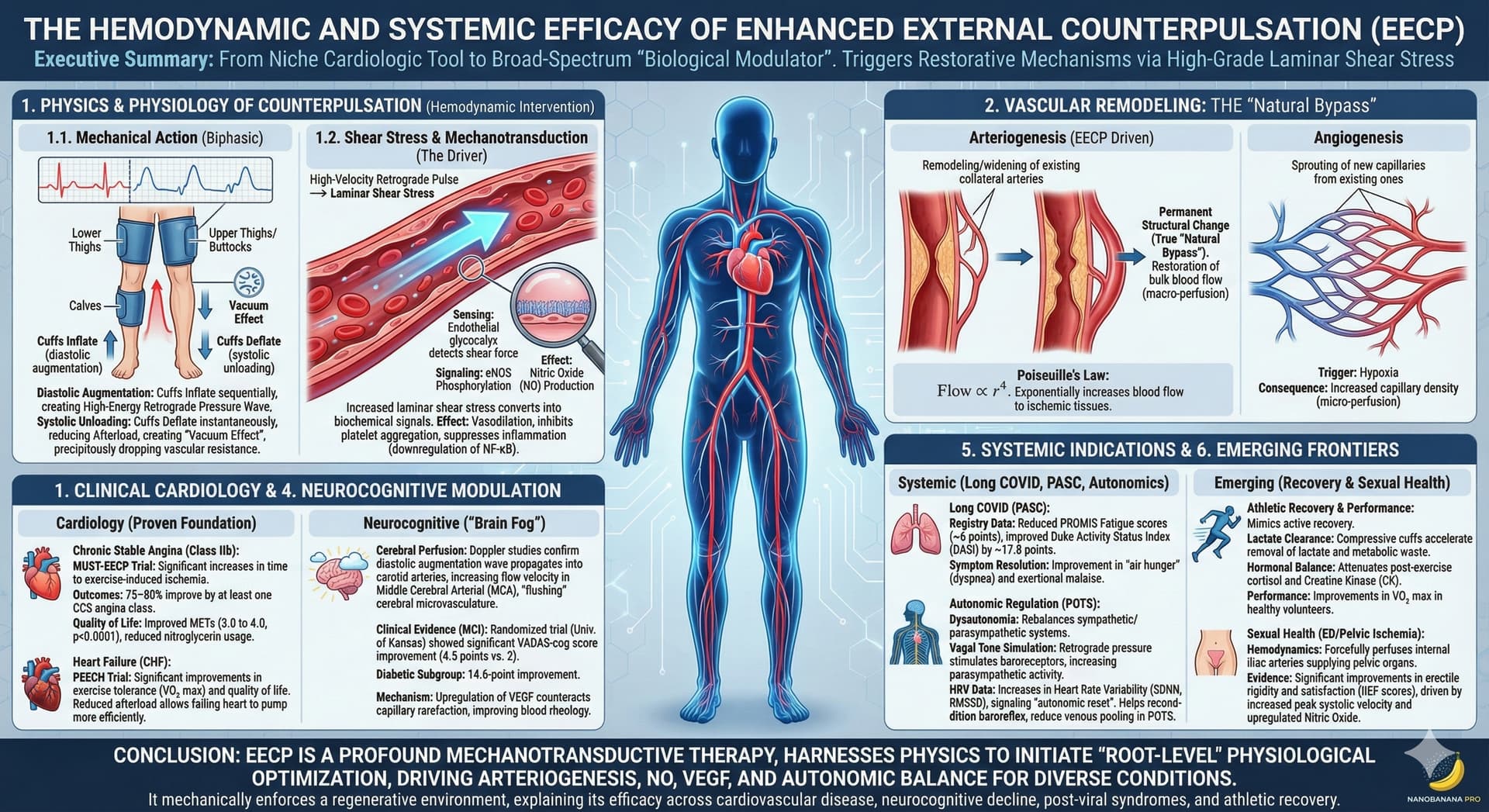
Enhanced External Counterpulsation (EECP) is evolving from a niche cardiological tool into a broad-spectrum physiological intervention. While historically FDA-cleared for refractory angina and heart failure, the aggregated literature suggests that EECP functions as a systemic “biological modulator.” By manipulating hemodynamics to generate high-grade laminar shear stress, the therapy triggers a cascade of restorative mechanisms—ranging from arteriogenesis and endothelial repair to autonomic balancing.
This review synthesizes the physics, physiological mechanisms, and clinical evidence supporting EECP. It critically examines the therapy’s role in treating cardiovascular disease, neurocognitive decline, post-viral syndromes (Long COVID), and athletic recovery, while distinguishing between proven clinical outcomes and emerging therapeutic frontiers.
What’s EECP? It’s an FDA approved therapy for certain types of angina (chest pain) and heart failure.
Why should I care? Blood Circulation: The Overlooked Fountain of Youth
1. The Physics and Physiology of Counterpulsation
To understand the pleiotropic effects of EECP—how a therapy for the heart can clear “brain fog” or aid athletic recovery—one must understand the underlying physics. EECP is not a pharmacological intervention; it is a hemodynamic one. It acts by mechanically altering the pressure waveforms within the central and peripheral arterial trees.
1.1 The Mechanical Action
The therapy utilizes a pneumatic system of compressive cuffs wrapped around the calves, lower thighs, and upper thighs/buttocks. These cuffs are synchronized with the cardiac cycle via microprocessor-interpreted ECG signals. The mechanism is biphasic:
- Diastolic Augmentation: As the heart relaxes (diastole), the cuffs inflate sequentially from the calves upward. This creates a high-energy retrograde pressure wave that travels up the aorta, forcing oxygenated blood into the coronary arteries (which fill during diastole) at supranormal pressures.
- Systolic Unloading: Milliseconds before the heart contracts (systole), the cuffs deflate instantaneously. This creates a “vacuum effect” in the lower extremities, precipitously dropping vascular resistance (afterload). When the heart ejects blood, it does so into a low-resistance pathway, significantly reducing myocardial oxygen demand.
1.2 Shear Stress and Mechanotransduction
The most critical physiological driver of EECP’s systemic benefits is Shear Stress. This is the frictional force exerted by blood flow against the endothelial monolayer lining the vessel walls.
In sedentary or diseased states, blood flow is often low or oscillatory (turbulent), promoting inflammation. EECP generates a high-velocity retrograde pulse that subjects the endothelium to increased laminar shear stress. This physical force is converted into biochemical signals via mechanotransduction:
- Sensing: The endothelial glycocalyx detects the shear force.
- Signaling: This triggers the phosphorylation of Endothelial Nitric Oxide Synthase (eNOS).
- Effect: The production of Nitric Oxide (NO), a potent gasotransmitter that induces vasodilation, inhibits platelet aggregation, and suppresses inflammation via the downregulation of NF-\kappa B.
2. Vascular Remodeling: The “Natural Bypass”
A central claim of EECP therapy is its ability to create a “natural bypass” around blocked arteries. Scientifically, this relies on the distinction between two types of vascular growth: angiogenesis and arteriogenesis.
2.1 Arteriogenesis vs. Angiogenesis
While often used interchangeably, these processes are distinct. EECP primarily drives arteriogenesis, which is the remodeling of existing collateral vessels, rather than just the sprouting of new capillaries.
| Feature | Angiogenesis | Arteriogenesis (EECP Driven) |
|---|---|---|
| Definition | Sprouting of new capillaries from existing ones. | Remodeling/widening of pre-existing collateral arteries. |
| Primary Trigger | Hypoxia (Oxygen deprivation). | Shear Stress (Fluid force). |
| Primary Consequence | Increased capillary density (micro-perfusion). | Restoration of bulk blood flow (macro-perfusion). |
| Hemodynamic Impact | Low. | High (True “Natural Bypass”). |
2.2 The Physics of Flow
The clinical impact of arteriogenesis is explained by Poiseuille’s Law, which states that blood flow is proportional to the fourth power of the vessel radius (Flow ~ r^4).
By mechanically widening collateral vessels via shear stress, EECP can exponentially increase blood flow to ischemic tissues. This explains why angina patients often experience relief that persists for years after treatment cessation; the “bypass” is structural and permanent.
3. Clinical Cardiology: The Proven Foundation
The foundational credibility of EECP rests on rigorous validation for cardiovascular disease.
3.1 Chronic Stable Angina
For patients with refractory angina (those unresponsive to maximal medication and unsuitable for stents/bypass), EECP is a Class IIb recommended therapy (ACC/AHA).
- Efficacy: The MUST-EECP randomized controlled trial demonstrated significant increases in time to exercise-induced ischemia.
- Outcomes: Registry data indicates that 75–80% of patients improve by at least one Canadian Cardiovascular Society (CCS) angina class.
- Quality of Life: Retrospective analyses show significant improvements in METs (Metabolic Equivalents) from 3.0 to 4.0 (p<0.0001) and reduced nitroglycerin usage.
3.2 Heart Failure (CHF)
Though increasing venous return in heart failure seems counterintuitive, the simultaneous reduction in afterload allows the failing heart to pump more efficiently. The PEECH Trial demonstrated that patients with NYHA Class II-III heart failure experienced significant improvements in exercise tolerance (VO_2 max) and quality of life compared to medical therapy alone.
4. Neurocognitive Modulation: Treating “Brain Fog”
Emerging research suggests EECP may be a powerful intervention for cognitive decline and “brain fog,” predicated on the vascular hypothesis of neurodegeneration.
- Cerebral Perfusion: Doppler studies confirm that the diastolic augmentation wave propagates into the carotid arteries, increasing flow velocity in the Middle Cerebral Arterial (MCA). This “flushes” the cerebral microvasculature.
- Clinical Evidence: A randomized trial at the University of Kansas Medical Center evaluated EECP in patients with Mild Cognitive Impairment (MCI).
- Results: The treatment group showed a statistically significant improvement in VADAS-cog scores (4.5 points vs. the FDA benchmark of 2 points).
- Diabetic Subgroup: The effect was most profound in Type 2 diabetics, who showed a staggering 14.6-point improvement.
- Mechanism: Upregulation of VEGF (Vascular Endothelial Growth Factor) likely counteracts age-related capillary rarefaction, effectively changing blood rheology “from ketchup to tomato juice.”
5. Systemic Indications: Long COVID, POTS, and Autonomics
The systemic nature of endothelial repair makes EECP a viable candidate for post-viral and autonomic syndromes.
5.1 Long COVID (PASC)
Long COVID is increasingly viewed as a thrombotic endothelialitis—persistent inflammation of the vessel lining.
- Registry Data: Studies show that Long COVID patients treated with EECP experience clinically significant reductions in PROMIS Fatigue scores (~6 points) and improvements in the Duke Activity Status Index (DASI) by ~17.8 points.
- Symptom Resolution: Improvement is frequently observed in “air hunger” (dyspnea) and exertional malaise, likely due to the restoration of proper perfusion matching in the lungs and muscles.
5.2 Autonomic Regulation and POTS
Dysautonomia involves an imbalance between the sympathetic (“fight or flight”) and parasympathetic (“rest and digest”) systems.
- Vagal Tone: The retrograde pressure wave stimulates arterial baroreceptors, triggering a reflex that inhibits sympathetic outflow and increases parasympathetic activity.
- HRV Data: Research indicates increases in Heart Rate Variability (HRV) indices (SDNN, RMSSD) following therapy, signaling an “autonomic reset.” This is particularly relevant for POTS (Postural Orthostatic Tachycardia Syndrome), where EECP helps recondition the baroreflex and reduce venous pooling in the legs.
6. Emerging Frontiers: Recovery and Sexual Health
6.1 Athletic Recovery and Performance
Elite athletes utilize EECP for its ability to mimic active recovery without metabolic cost.
- Lactate Clearance: The compressive cuffs accelerate the removal of lactate and metabolic waste products.
- Hormonal Balance: Studies suggest EECP attenuates the post-exercise rise in cortisol and Creatine Kinase (CK), maintaining a more favorable anabolic environment for tissue repair.
- Performance: Surprisingly, even healthy volunteers have shown improvements in VO_2 max, suggesting that systemic endothelial conditioning can raise the ceiling of aerobic performance.
6.2 Sexual Health and Pelvic Circulation
Erectile Dysfunction (ED) is often the “canary in the coal mine” for systemic vascular disease.
- Hemodynamics: EECP forcefully perfuses the internal iliac arteries, which supply the pelvic organs.
- Evidence: Studies utilizing the International Index of Erectile Function (IIEF) show significant improvements in erectile rigidity and satisfaction, driven by increased peak systolic velocity in penile arteries and upregulated Nitric Oxide production. This mechanism applies equally to female sexual dysfunction related to pelvic ischemia.
7. Critical Appraisal and Safety
While the potential of EECP is vast, a critical scientific view is necessary.
- Safety Profile: EECP is non-invasive and generally safe. However, strictly defined contraindications exist, including severe aortic regurgitation (where retrograde flow would be detrimental), abdominal aortic aneurysms (>5cm), and deep vein thrombosis (DVT).
- Limitations of Evidence: While the cardiovascular data is robust (RCTs like MUST-EECP and PEECH), evidence for “biohacking,” longevity, and general wellness relies heavily on smaller studies, registry analyses, and mechanistic extrapolation.
- Realistic Expectations: The claim of creating an “entirely new vascular system” is hyperbole; EECP remodels and optimizes the existing collateral network. It is a biological amplifier, not a magic wand.
Conclusion
The synthesis of available literature confirms that Enhanced External Counterpulsation is a profound mechanotransductive therapy. By harnessing the physics of shear stress, EECP initiates a “root-level” physiological optimization that transcends its original cardiac indications.
The therapy works by mechanically enforcing a regenerative environment: it upregulates VEGF and Nitric Oxide, drives arteriogenesis, clears metabolic waste, and rebalances the autonomic nervous system. This singular mechanistic cascade explains its efficacy across diverse conditions—from restoring cardiac output in heart failure and clearing the “brain fog” of dementia, to resolving the endothelial inflammation of Long COVID and enhancing athletic recovery. For patients seeking to optimize vascular health and physiological resilience, EECP may represent a scientifically validated method to reverse endothelial dysfunction.
Detailed research & references: EECP Research: FDA Uses and Beyond - Google Docs