OK, let’s assume so. However, I would highlight another sentence from your quote:
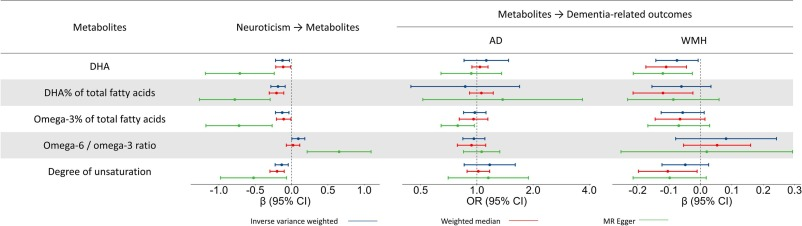
“Mendelian randomization analysis suggested that high levels of neuroticism reduce DHA levels, which, in turn, contribute to white matter pathology, a hallmark of VaD.”
Neuroticism —-> Low DHA —-> VaD.
In this scenario, the problem with “neuroticism” is that it leads to “low DHA”, and if “low DHA” leads to, i.e. is causative (rather than just associated with) per the passage you quoted and I highlighted, of Vascular Dementia, then if we can prevent the lowering of DHA, then assuming this is the causative mechanism, we should be able to prevent the white matter pathology that’s a hallmark of VaD.
Neuroticism can be characterized as “cognitive issues” as you have done in your statement I quoted first. But note, neuroticism in and of itself is not diminishment of intellectual ability like in dementia, but more along the lines of a personality disorder. If you can abolish the downstream effect of prolonged neuroticism (in this scenario) resulting in the lowering of DHA, then prolonged neuroticism should not result in white matter pathology development in vascular dementia and will just remain a personality disorder.
That would argue for finding a means of preventing the decline of DHA (which according to the mechanism that paper outlined) leads to VaD downstream from neuroticism.
But whether supplementing with DHA in fishoil form is the optimal way of raising DHA levels in the brain (or other tissues) is a whole different question - and I have previously posted the paper showing the paradoxical impact of exogenous DHA on the endogenous status of DHA. Yes, DHA in the brain (and other tissues) is important, but that doesn’t mean you can just supplement with DHA in pills and have that translate to proper incorporation into brain tissue.
So even if “low DHA” —-> “VaD”, doesn’t mean “supplemental DHA pills” —-> “adequate DHA levels”. IOW, a neurotic person supplementing with DHA pills might not prevent the development of VaD.
Bottom line, the story of DHA function and levels in the brain (and other tissues), must be considered within the context of “and how exactly do we control those levels”, because it’s not simply by supplementing with DHA pills. We can also ask “does serum DHA translate into DHA incorporation in brain (and other) tissue”? Because maybe supplemental DHA raises serum levels while suppressing incorporation into tissue. Endogenous DHA conversion incorporates DHA into tissues (including brain) - we know this, because even people who don’t consume any long chain marine (or animal) omega-3 FA, don’t lack DHA in their tissues - if they did lack, then all vegans would be dead because omega-3 FA are essential FA. And we have lifelong vegans in many cultures on a multigenerational scale. They do it by converting short chain ALA n-3 to DHA. Studies show that vegans DHA status is just as high (and according to many studies higher!) than omnivores. And again as in the paper I posted previously, supplemental exogenous DHA interferes with that conversion, thus being a net negative. It is therefore crucial to make a distinction between the importance of “tissue DHA” status and “supplemental exogenous DHA”.