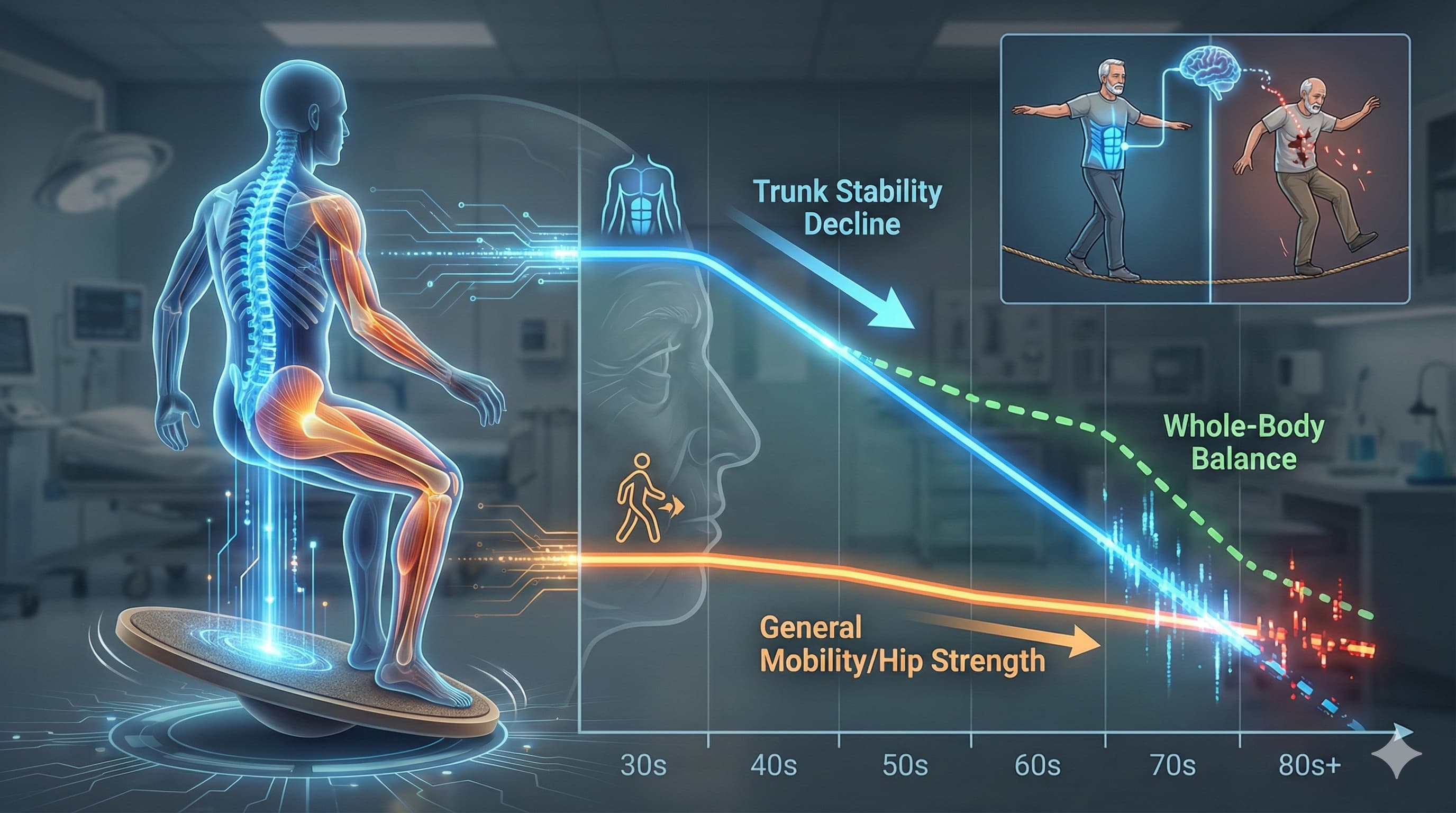
A new study has identified trunk stability (core control) as a rapidly deteriorating physical capability that outpaces declines in general mobility and hip strength during aging, particularly in males. While traditional metrics like the “Timed Up & Go” (TUG) test remained relatively stable in physically active older adults, trunk stability—measured by the ability to control the upper body on an unstable seat—showed a steep, linear decline starting as early as age 30. Crucially, this study reveals that trunk stability is the primary predictor of whole-body dynamic balance, suggesting that “core control” is not just about strength, but is a critical neuro-mechanical prerequisite for preventing falls. This implies that standard gym routines focusing on gross strength may fail to address the specific proprioceptive and fine-motor degradation of the trunk that compromises longevity.
Source:
- Open Access Paper: Understanding the effects of aging on whole-body dynamic balance, trunk stability, functional mobility, and hip strength
- Institution: Miguel Hernández University of Elche, Spain
- Journal: Scientific Reports
- Impact Evaluation Journal Impact Factor (JIF):** ~3.8 (2024/2025 data), Therefore, this is a Medium impact journal. It is a high-volume, peer-reviewed mega-journal that validates scientific rigor rather than novelty or significance alone.
Part 2: The Biohacker Analysis
Study Design Specifications
- Type: Cross-Sectional Observational Study
-
Subjects: Human (N=127).
- Demographics: Healthy, physically active adults aged 30–80 years.
- Sex Distribution: 42 Males, 85 Females.
- Activity Level: 120–300 minutes of physical activity per week.
Mechanistic Deep Dive
This research dissects the biomechanical “inverted pendulum” model of human aging, identifying Trunk Stability as the weak link in the kinetic chain.
- Neuromuscular Decay: The study differentiates between “Global” functional mobility (TUG test) and “Local” fine motor control (Unstable Sitting). The rapid decline in trunk stability (R^2=71% variance in males) suggests that general physical activity preserves gross motor function (legs/hips) but fails to arrest the decay of fine neuromuscular control in the core.
- Proprioceptive Failure: The authors posit that the degradation is driven by age-related reductions in proprioception and reaction time, which are critical for the micro-adjustments required to stabilize the torso.
- The “Core” Driver: Correlation analysis revealed that trunk stability is the strongest predictor of tandem stance balance (r=0.629, p<0.013). This suggests that “balance” exercises are downstream of “core stability.” If the trunk cannot be stabilized, the vestibular and visual systems cannot effectively orient the body.
Novelty
- Differential Decay Rates: This paper provides quantitative evidence that physical systems age at vastly different rates. In males, trunk stability deteriorated ~4.48% per year, whereas functional mobility (TUG) only declined by ~0.55% per year.
- The Male “Stiffness” Trap: The data identified a sex-specific vulnerability. Males showed a much sharper decline in trunk stability than females (R^2=71% vs R^2=46%). This supports the hypothesis that aging males rely on “rigidity” strategies rather than the dynamic control strategies seen in females, leading to a catastrophic loss of function when that rigidity fails.
- Unstable Sitting Protocol: The use of a specialized unstable seat isolates the trunk from lower-limb compensation, offering a purer metric of core neuro-control than traditional planking or standing tests.
Critical Limitations
- Cross-Sectional Confounding: As a cross-sectional study, it cannot distinguish between true aging effects and cohort differences (e.g., 80-year-olds today may have different lifelong activity patterns than 30-year-olds).
- “Healthy Survivor” Bias: The cohort was highly active (up to 300 min/week). The results likely underestimate the decline in the general, sedentary population.
- Sample Imbalance: The study suffered from significant imbalance in sex and age distribution, specifically a lack of males in their 50s and a 2:1 female-to-male ratio, limiting the statistical power of subgroup analyses.
- No Causality: The study identifies correlations (core stability to balance) but cannot prove that training core stability causes improved balance without a longitudinal intervention.
[Confidence: High]