This is a post pulling together my pre-op protocol, in the hope that anyone who is interested in the subject in the future, when searching may come across this and may find something useful. This is a work in progress, and I will come back after the operation and assess what worked and what not (at least for me).
Your surgeon, insurance and the team
This may be obvious, but your surgeon is going to be key. Vet them shamelessly. Have they done the procedure often enough. Is there patient feedback. What’s the reputation. Talk/email them - I did so, I asked for the number of procedures he did and complication rates - it’s just due diligence. He answered comprehensively with all percentages including patient satisfaction rates. He came highly recommended with a stellar reputation. I read the pubmed papers he was a co-author on. I talked to people.
Insurance. You really want to be clear on costs and coverage ahead of time. No surprises. There’s nothing worse than dealing with claims and financial complications when you’re trying to recover.
What’s the team like? I’m having my operation at UCLA a teaching hospital with excellent staff. So far, my pre-op care has been excellent.
Medication, Supplements
I take several meds which are not prescribed by my physician. Some of these have counterindications for surgery. In any case, my thought is that I don’t want anything in my system that is not officially in my charts - this less because of some known complications and more because I may not be aware of all subtleties regardless of my own exhaustive research. Therefore, I have looked up how long it takes for the various meds to clear out of the system, and I intend to stop them all with a safety margin. The same for all supplements.
Crucially, a few days before the surgery, I have already booked a blood test with LabCorp to look at my various biomarkers and to make sure that sirolimus is out of my system completely.
However, leading up to that stoppage, you might want to nourish your body with minerals, vitamins and supplements for a few weeks, which might be helpful. I won’t list the full protocol for each, just mention a few such supplements: various forms of calcium and magnesium, vitamin D3, vitamin K1 and K2 (mk4. mk7), vitamin A, B12, manganese, soy isoflavones, zinc, boron, glucosamine, astaxanthin etc. Obviously, you should develop a protocol to fit these into your stack without too much conflict.
Exercise
In general, you are going to be restricted for some time after the surgery, and also, you want to be in as good a shape as possible going into the surgery. For this I divide the exercise into two parts.
General conditioning
I’m doing a lot of cardio and some muscle weight bearing with emphasis on functionality. So, jogging almost every day, with HIIT-like bursts in two of those sessions a week, plus a high tempo very strenuous hiking up hill once a week. Then the regular squats and other functional muscle exercises.
Pre-hab
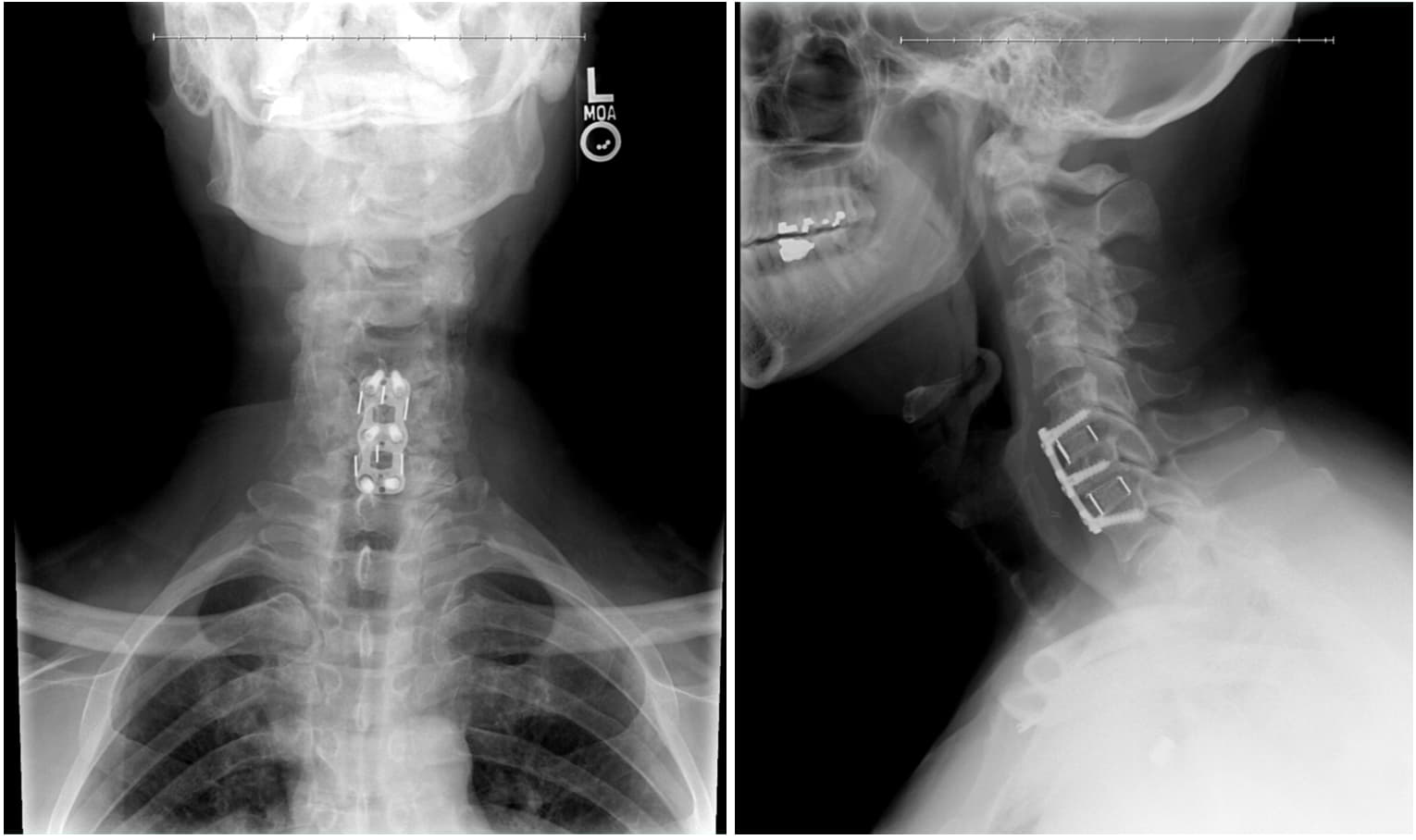
There are a range of exercises prescribed as PT for rehab after surgery. There are also a range of exercises you can do pre-surgery which will prepare your musculature for the challenges ahead, so you get a jump start on the rehab exercises. You do them now, so that you can learn them well and they become part of your regular exercise and you hit the ground running after your surgery. These you can find from your PT pre-surgery and from yt videos on rehab after ACDF surgery. I have both resources and I’m doing these daily.
Education
Read up on your surgery. Understand what is being done and why. There are tons of studies on pubmed, and demos on yt and patient testimonials. Learn what the possible complications might be and prepare ahead of time, and try to avoid risk factors insofar as possible. You should be fully prepared for what to expect. Let the experience of those who came before you prepare you for what’s to come.
Hardware and med supplies
Get enough of these to not have to hunt for them or buy once you’re back home. Scar tissue creams - there are dedicated ones out there for purchase on Amazon. Good quality bandaids that are waterproof and easily removable. Numbing lozenges such as sucrets. Cervical neck pillow. Hot and cold compresses (for some cold works, for some heat). Remember: you will be limited in motion, bending, raising arms, twisting neck, turning etc. Get slip on shoes, the kind you just need to put your foot in, without bending, looking down, tying shoelaces etc. they sell a bunch on Amazon (I bought Sketchers). Prepare a bunch of clothing you can take on and off easily - buttons and zippers, nothing you need to pull overhead - button shirts, zippered hoodies, wife-beater undershirts you can just slip off your shoulders and down, not up over the head. Also, more open neck shirts - you will have a scar on your neck, don’t irritate it with clothing. Get a bunch of straws and also sports bottles you can sip from without throwing your head back.
You will be put on antibiotics and painkillers. This means you will need to stimulate your BM - stock up on magnesium oxide, stool softeners, and gut biome restoring agents, fiber, fermented foods, maybe tributryn (antibiotics might wipe out gut bugs, but you still want butyrate!). Why stock up? Because you don’t want to start assembling once you need it immediately and find out they’re out of your favorite low salt kimchi or sauerkraut etc. Get new manual toothbrushes and heads for your electric - you will be extra vulnerable to infections in your throat and your cervical spine - you don’t want germs insofar as you can help it, so all new implements should wait for you when you come back from surgery, new interdental brushes and so on.
Get your diet dialed in. Prepare all the soft stuff you will need when swallowing is hard. But you don’t want it to be unhealthy. Preparing ahead of time, will make that easier.
Modify your home environment
You won’t be able to bend your head, twist or turn the neck for some time, or lift heavier objects (5-10lbs). No overhead items. Purchase a soft neck brace (as little as $10 on amazon), not because you will necessarily wear it after surgery (depends on your surgeon), but because it will immobilize your neck in a way that will mimic your limitations immediately after surgery. With this neck brace - wear it for a couple of full days and walk and work around your house. Quite eye opening. Get everything you need at eye level, not high up on some shelf - you won’t be reaching. You won’t be able to look down at your feet much. Clear away stuff that you may bump into - stuff in the way, slippery carpets etc. The bathroom as well as the kitchen can have quite a few traps and surprises. Is your bed ready for you to roll out of without sitting up? Is your night table within reach and items on it accessible to blindly reaching for? The neck brace will reveal a lot.
This can be extended to you outside environment too - your garden and also your neighborhood. You will be walking quite a bit. Put on the brace and walk around. You will soon map out which paths to take - no bumps, no obstacles, low hanging branches, dog parks where dogs can enthusiastically jump on you or playing kids can bump into you. Clear views without having to turn or twist your neck, safe from cars or joggers around corners who might crash into you. Walk around, map out, prepare.
Even if you won’t wear a neck brace post surgery, it might still be useful for sleeping or being outside - there, you wear it to signal “glass - handle with care”, so people don’t slap you on your back or expect you to move swiftly, or bump into you with a cart at a store or such. Crazy example: just last weekend I was hiking in the local hills and a couple of guys were throwing a football around, one of them playfully threw it at me as I was passing, and I had to throw it back. Umm, hopefully he wouldn’t do it if I had a neck brace on advertising - NO SUDDEN MOVEMENTS PLEASE!
Look around the house. Does anything need to be done that will be harder post surgery? Need to change lightbulbs? Bring something from upstairs to downstairs? Put away something on a high shelf for storage? Pull something OUT of high shelf storage? Fix something high up or paint something? Fix stuff around the house that will be a hassle otherwise, even trivial stuff - you will need to focus on recovery, not exchanging an uncomfortable chair or doing some mundane task that needs concentrating. Mow the lawn, fix the window, trim the hedge ahead of time.
Prep - body, procedures, after care
You won’t be able to be at the dentist with your neck for some time. Even after a few weeks, you will still need to be on antibiotics if any dental procedures need to be done. So, why not get it all out of the way ahead of time?
1)Get all your dental work done ahead of time - teeth cleaning and gum care also. You don’t want to have excess germs in your mouth (your throat, and more importantly your newly fused spine!). Your dental hygiene should be impeccable. No bleeding gums, no gingivitis, no periodontal issues, no decayed teeth - these are germ volcanoes. And you don’t want a dental emergency just after surgery. You should get your mouth in tip top shape, so you don’t need to visit a dentist for at least 6 months and not have to gobble up antibiotics to do so.
2)Get a haircut. You don’t want to have hair irritating and a nuisance when you can’t turn your head or have it manipulated. Get it out of the way ahead of time.
3)Cut your toenails, trim dead skin and sort out any problems with your feet - you won’t be able to bend easily and it’s just a hassle - having your significant other do it or hiring a pedicure/manicurist.
Assistance
Do you live alone? Your significant other hopefully is going to be free for a few weeks (unless they work), but make sure to get help around the house, hire somebody if you have to - zero in on candidates ahead of time. You may find yourself needing assistance, perhaps unexpectedly. You can’t anticipate everything, so you will need others to pitch in.
Have your significant other drive with you in the passenger seat from the hospital or wherever your surgery takes place to your home AHEAD of time, so that you can anticipate traffic patterns, unpleasant surprises, potholes and the like. The drive home after the operation should be smooth and free from shocks.
Odds and ends
Everything should be put on a flowchart - dates and actions that need to be taken at any given point. That way, you only need to refer to it to see what needs to be done on any given day and into the future.
Prepare a checklist before you go in for the surgery. Everything needs to be on the list. The items you want to take, including documents, actions to complete (charge phone etc.), phone calls to be made. Whom to inform of what. What to hand off to your significant other when you are ready to be taken.
Sanity check
All of this prep is fiddling at the margins. 99.99% is up to the skill of your surgeon, your condition and blind luck. All of the above is 80% psychological to give you the feeling of at least some control over your fate (even if illusory) - this makes it mentally easier to take charge of your recovery and maintains an active stance in your healthcare (and life). You are not a passive subject, but an active participant in your own care.
One thing is certain: there will be surprises. Take them as they come, because your conscience is clear: you’ve done all you could to prepare and have no regrets. What cannot be anticipated is not material for self-reproach. You’ve done your part. But life still has its say.
To be revised as needed, and revisited post surgery for assessment!