Thank you! I’m trying to understand all of the better! @Joseph_Lavelle has been very helpful as well! I love this place.
Turkish paper + MDPI so low quality but:
Results: The empagliflozin group showed significant improvements in HbA1c, fasting plasma glucose, body weight, waist circumference, and fat mass (p < 0.05 for all). No significant changes were observed in the empagliflozin group after 6 months in appendicular skeletal muscle mass index (from 7.81 ± 1.33 kg/m2 to 7.84 ± 1.38 kg/m2, p = 0.154). No statistically significant changes were observed in handgrip strength in either group.
Conclusions: Empagliflozin treatment over six months led to favorable changes in metabolic parameters and fat mass without detrimental effects on skeletal muscle mass or muscle strength. In clinical practice, the selection of antidiabetic therapies should consider individual glycemic targets, cardiovascular and renal risks, weight management, comorbidities and sarcopenia risk. Resistance exercises and adequate dietary protein intake should be recommended to preserve muscle mass in at-risk patients. Larger randomized trials are needed to confirm the long-term effects of SGLT2 inhibitors on body composition particularly in older adults.
Sodium-glucose cotransporter-1 inhibition and depression: A Mendelian randomization study 2025
Results: Our results indicated that genetically predicted sodium-glucose cotransporter-1 inhibition was negatively related with depression risk (ORIVW = 0.78; 95% CI: 0.67–0.91, p = 0.002) in the European population. However, we did not find a causal association between sodium-glucose cotransporter-2 inhibition and depression (OR IVW = 0.98; 95% CI: 0.71–1.36, p = 0.919).
Just spit balling but this points to gut health as a possible mechanism here, given SGLT1-inhibition occurs in the GI. I wonder if there have been any studies looking at SGLT1-inhibitors and gut health specifically.
Personal anecdote:
I’ve been on dapagliflozin a little over a month and I’ve worked up to taking 5mg from 2.5 initially. I’m now able to tolerate restaurant meals without any fluid gain. I still try to make the best choices (lowest sodium) possible when eating out and stick with a no added salt diet otherwise but it’s a very welcome change to not deal with 2-3 pounds of fluid that would stick around for several days. I had gotten to the point of dreading dining out which was a shame because it’s a somewhat regular social activity amongst my family and friends. I do not have diagnosed cardiovascular or renal disease and I’m not diabetic but this medication has turned out to actually be my favorite longevity intervention. Obviously something wasn’t working optimally in my body. I also no longer have sock marks when I take my socks off which is pretty neat. My BP and weight haven’t changed and both were already optimal so I’m happy.
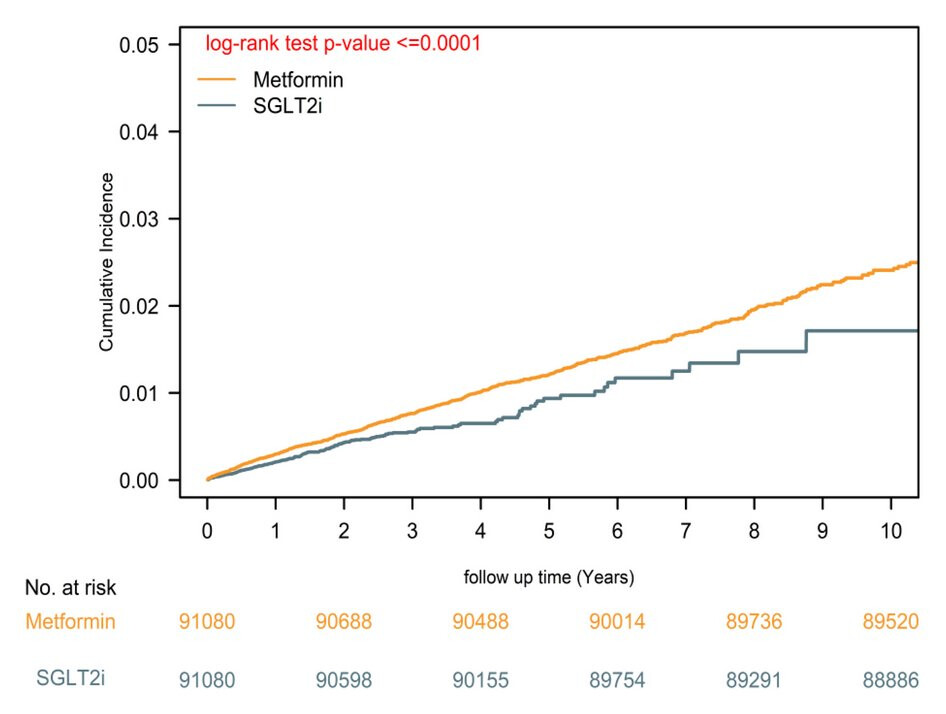
SGLT2 inhibitors vs. metformin for Parkinson’s disease risk reduction in type 2 diabetes 2025
SGLT2i use was associated with a 28% lower PD risk than metformin (aHR = 0.72; 95% CI, 0.62–0.84; p < 0.0001). Dementia, a positive control, also showed reduced risk (aHR = 0.73; 95% CI, 0.68–0.78; p < 0.0001), reinforcing the neuroprotective effect. Negative controls confirmed specificity. SGLT2i users had significantly lower all-cause mortality (aHR = 0.85; 95% CI, 0.83–0.89; p < 0.0001).
Nice study, thanks. The ACM benefit was small, but good to see it, 15%.
In the forest plot of figure 2, we can see that these were beneficial in statin users. And the confidence intervals were good. Does that tell us anything about statins and PD?
Do we know which specific SGLT2i are commonly used in China, or in this particular setting? I’m wondering if this is a broad class effect or there is some particular drug that predominates here.
I don’t think we can conclude anything from that.
It seems that dapagliflozin has the vast majority of the Chinese market: 2024年七大类降糖药解析:SGLT2i为何成指南首选?_摩熵医药(原药融云)
OK, so a common one used in the West. I was afraid it might be some obscure one only used in China.
I wonder about the effect in early stage PD. They got a good group of patients there, should be possible to do some data mining.
Interesting paper about MR: The paradox of SGLT2 inhibitors in heart Failure: Caution with drug target Mendelian randomization 2025
Mendelian randomization (MR) is a well-established technique in epidemiological research. Despite its utility, several challenges in drug target MR applications remain underexplored. This study investigates the association between sodium-glucose cotransporter-2 inhibitors (SGLT2i) and heart failure (HF), employing various selections of instrumental variables (IVs) for SLC5A2 and emphasizing the necessity of positive controls. Initial summary data-based MR analysis showed that increased expression of SLC5A2 (equivalent to a one standard deviation [SD] increase) was significantly associated with Type 2 diabetes (T2D) (OR: 0.76, p = 0.038). The association with HF was not statistically significant (odds ratio [OR]: 1.30, p = 0.107). Subsequently, inverse variance weighted (IVW)-MR analysis demonstrated the association between SLC5A2-mediated HbA1c (one SD increase) and T2D (OR: 1.40, p = 0.196) and HF (OR: 0.61, p = 0.026). These IVs potentially indicated the invalid of positive control. We further constructed IVs based on the mRNA expression of SLC5A2 (p < 0.001, primarily in human blood) and assessed the association of each variant with HbA1c. IVW-MR analysis revealed significant associations between SLC5A2-mediated HbA1c (one SD increase) and T2D (OR: 2.37, p = 2.30E-7) and HF (OR: 0.45, p < 0.001). Finally, we constructed IVs from the most significant SNPs within all tissues, yielding significant associations for both T2D (OR: 3.05, p = 2.30E-7) and HF (OR: 0.44, p = 0.003). Therefore, we advocate for researchers conducting MR analysis of drug targets to report their instrumental variables, comprehend the pharmacological mechanisms involved, present positive control results and cautiously interpret their conclusions.
Sodium‐glucose cotransporter 1/2 inhibition and risk of neurodegenerative disorders: A Mendelian randomization study
“SGLT1i exhibited a significant association with decreased risk for ALS and MS. Conversely, SGLT2i were linked to an increased risk of AD, PD, and MS. Elevated HbA1c levels, independent of SGLT1 and SGLT2 effects, were associated with an increased risk of PD. Sensitivity analyses supported the robustness of these findings.”
“Our study suggests that SGLT1i may confer protection against ALS and MS, whereas SGLT2i could elevate the risk of AD, PD, and MS. Additionally, elevated HbA1c levels emerged as a risk factor for PD. These findings underscore the importance of personalized approaches in the utilization of SGLT inhibitors, considering their varying impacts on the risks of neurodegenerative diseases.”
Sorry, wasn’t aware of that. Like I said, we ought to have a PMID database we can input and check against. Apologies.
Separately, I do try to read whole threads, but because I read so many studies, I don’t always remember where I saw a study first - on this or some other site or on PubMed, as I access PubMed every day.
No worries at all. In this case, searching for the paper’s title would point you to the previous post. But it doesn’t always work (poke @RapAdmin to update the search and fix the bugs ![]() ).
).
Anyway, this MR study is interesting but I find it weird due to the effect being so large and contradicting many longitudinal studies and some models. The previous paper pointing to the risk of MR makes me even more skeptical considering the weak institution it originates from: Canagliflozin - Another Top Longevity Drug - #1625 by adssx
“SGLT2i use was associated with a 28% lower PD risk than metformin (aHR = 0.72; 95% CI, 0.62-0.84; p < 0.0001). Dementia, a positive control, also showed reduced risk (aHR = 0.73; 95% CI, 0.68-0.78; p < 0.0001), reinforcing the neuroprotective effect. Negative controls confirmed specificity. SGLT2i users had significantly lower all-cause mortality (aHR = 0.85; 95% CI, 0.83-0.89; p < 0.0001)”
“Sodium-glucose cotransporter 2 inhibitors showed increased reporting odds ratio for bladder cancer (ROR 4.46, 95% CI 3.23-6.17) and kidney cancer (ROR 1.84, 95% CI 1.25-2.69)”
“SGLT-2is are associated with an increased risk of reporting bladder and kidney cancer. There is a need of an urgent clarification of this signal with further long-term observational studies”
*Important note: multiple other published reports show NO increase risk, or even a decreased risk in the case of renal cell carcinoma: Decreased risk of renal cell carcinoma in patients with type 2 diabetes treated with sodium glucose cotransporter-2 inhibitors - PubMed
Thanks for sharing. Some other papers did not find an increased risk (e.g., Sodium–Glucose Cotransporter 2 Inhibitors and the Short-term Risk of Bladder Cancer: An International Multisite Cohort Study 2022, SGLT2 inhibition and three urological cancers: Up-to-date results 2024, Sodium-glucose cotransporter 2 inhibitors and cancer: a systematic review and meta-analysis 2024) but one Mendelian randomization paper confirmed the increased risk! Deciphering the Causal Relationship between Sodium-glucose Cotransporter 2 Inhibition and Cancer Risks: A Comprehensive Mendelian Randomization Study 2024. Is it clinically meaningful though? ![]()
Btw, be aware that PubMed will not be available July 25 for 24+ hours:
“Service Alert: Planned Maintenance beginning July 25th
Most services will be unavailable for 24+ hours starting 9 PM EDT”
Heavy users of PubMed (moi!) please prepare accordingly. Get to the papers you may want ahead of time and stock up to survive the blackout period.