Pioglitazone and ceramides.
Pioglitazone reduces cardiovascular events and dementia but increases bone fracture in elderly patients with type 2 diabetes mellitus: a national cohort study
“In results, the pioglitazone group (n = 17,388) exhibited a lower rate (per person-years) of major advanced cardiovascular events MACCE (2.76% vs. 3.03%, hazard ratio [HR]: 0.91, 95% confidence interval [CI]: 0.87–0.95), new- diagnosis dementia (1.32% vs. 1.46%, HR: 0.91, 95% CI: 0.84–0.98) but a higher rate of new-diagnosis bone fractures (5.37% vs. 4.47%, HR: 1.24, 95% CI: 1.19–1.28) than the non-pioglitazone group (n = 174,549). In conclusion, using pioglitazone may reduce the risks of MACCE and dementia but increases the probability of bone fractures in the elderly DM population.”
This study was mentioned further up in this thread:
Pioglitazone use increases risk of Alzheimer’s disease in patients with type 2 diabetes receiving insulin
Note, these are insulin dependent diabetics.
What if insulin was removed from the equation:
Effect of pioglitazone medication on the incidence of dementia
"Long-term use of pioglitazone was associated with a lower dementia incidence. Relative to nondiabetics, the cumulative long-term use of pioglitazone reduced the dementia risk by 47% (RR = 0.53, p = 0.029). If diabetes patients used pioglitazone <8 quarters, the dementia risk was comparable to those of nondiabetics (RR = 1.16, p = 0.317), and diabetes patients without a pioglitazone treatment had a 23% increase in dementia risk (RR = 1.23, p < 0.001). We did not find evidence for age effects, nor for selection into pioglitazone treatment due to obesity.
Interpretation: These findings indicate that pioglitazone treatment is associated with a reduced dementia risk in initially non-insulin-dependent diabetes mellitus patients. Prospective clinical trials are needed to evaluate a possible neuroprotective effect in these patients in an ageing population."
Lower risk of dementia with pioglitazone, compared with other second-line treatments, in metformin-based dual therapy: a population-based longitudinal study
Effects of pioglitazone on the incidence of dementia in patients with diabetes
“Pioglitazone is a time- and dose-dependent protective factor against dementia in patients with diabetes. The risk of dementia is lower in long-term and high-dose pioglitazone users than in never users of pioglitazone.”
Pioglitazone Use and Reduced Risk of Dementia in Patients With Diabetes Mellitus With a History of Ischemic Stroke
“Pioglitazone use was associated with a reduced risk of dementia, compared with nonuse (adjusted hazard ratio [aHR] = 0.84, 95% CI 0.75–0.95); the risk reduction in dementia was greater among patients with a history of ischemic heart disease or stroke before DM onset (aHR = 0.46, 95% CI 0.24–0.90; aHR = 0.57, 95% CI 0.38–0.86, respectively). The incidence of stroke was also reduced by pioglitazone use (aHR = 0.81, 95% CI 0.66–1.00). However, when the stroke developed during the observation period of pioglitazone use, such lowered risk of dementia was not observed (aHR = 1.27, 95% CI 0.80–2.04).”
Ralph DeFronzo Banting Hall lecture from some years ago, getting into the details of insulin resistance in the context of atherosclerosis. There is a lot of cellular and molecular information which I think gives us a good picture of the processes involved. There is also light thrown on pioglitazone, as he says “the only true insulin sensitizer”:
Banting Hall - Dr. Ralph A. DeFronzo (via Diavcon 2020)
This is very interesting. However we must look at it in a nuanced way. Pioglitazone is definitely associated with greater rates of bladder cancer (cumulative dosage and time dependent), so it would be a big mistake to see pioglitazone as anti-cancer in general. That said, in limited circumstances, for PPAR-gamma mediated cancers like PC, it may have some use. Given the relative incidence of PC vs bladder cancer, this might be an interesting drug.
The anti-diabetic PPARγ agonist Pioglitazone inhibits cell proliferation and induces metabolic reprogramming in prostate cancer
“Our findings suggest that using metabolic drugs such as PPARγ agonists could improve PCa treatment outcomes by reducing tumor growth, reprogramming metabolic pathways, and promoting a more benign epithelial phenotype.”
Note, we are talking extant PC, which is distinct from primary prevention.
If I remember well that is the reason why it has be removed from the market in France and in a lot of EU countries.
Yes. That was the reason. There was some controversy about the exact risk numbers, but longer term use can elevate relative risk to 1.75 times. In absolute numbers over the span of years it may be a risk worth taking compared to benefits. That said, pioglitazone is definitely contraindicated in those who have previously had bladder cancer or strong risk factors for it. This is the next biggest risk after the risk of bone fractures. It’s a drug that needs careful consideration and close monitoring. That’s why I’m still researching it and not just jumping in. Preliminarily my plan is to try it at a low dose of 7.5mg/day later this year and evaluate it along the way for effectiveness vs A1c and fasting blood sugar.
Comparison of the Effects of Pioglitazone and Metformin on Hepatic and Extra-Hepatic Insulin Action in People With Type 2 Diabetes
(1) “Insulin-induced stimulation of glucose disappearance did not differ before and after treatment with either pioglitazone (23 ± 3 vs. 24 ± 2 μmol · kg−1 · min−1) or metformin (22 ± 2 vs. 24 ± 3 μmol · kg−1 · min−1). In contrast, pioglitazone enhanced (P < 0.01) insulin-induced suppression of both glucose production (6.0 ± 1.0 vs. 0.2 ± 1.6 μmol · kg−1 · min−1) and gluconeogenesis (n= 11; 4.5 ± 0.9 vs. 0.8 ± 1.2 μmol · kg−1 · min−1). Metformin did not alter either suppression of glucose production (5.8 ± 1.0 vs. 5.0 ± 0.8 μmol · kg−1 · min−1) or gluconeogenesis (n = 9; 3.7 ± 0.8 vs. 2.6 ± 0.7 μmol · kg−1 · min−1). Insulin-induced suppression of free fatty acids was greater (P < 0.05) after treatment with pioglitazone (0.14 ± 0.03 vs. 0.06 ± 0.01 mmol/l) but unchanged with metformin (0.12 ± 0.03 vs. 0.15 ± 0.07 mmol/l).
CONCLUSIONS - Thus, relative to metformin, pioglitazone improves hepatic insulin action in people with type 2 diabetes, partly by enhancing insulin-induced suppression of gluconeogenesis. On the other hand, both drugs have comparable effects on insulin-induced stimulation of glucose uptake.”
(2) “We report that, whereas pioglitazone and metformin have comparable effects on insulin-induced stimulation of glucose uptake, pioglitazone improved hepatic insulin action at least in part by enhancing insulin-induced suppression of gluconeogenesis.”
(3) “Treatment with pioglitazone resulted in an marked increase (P < 0.01) in both total and high molecular weight (HMW) plasma adiponectin concentrations (Fig. 6). In contrast, neither total nor HMW plasma adiponectin concentrations changed after treatment with metformin.”
(4) “Taken together, these data suggest that in the presence of low physiological insulin concentrations, the effects of pioglitazone on hepatic insulin action is likely as important, if not more important, than the effects of pioglitazone on extra-hepatic insulin action in the regulation of glucose metabolism.”
(5) “Thus, the common belief that pioglitazone improves glycemic control in people with type 2 diabetes primarily by increasing glucose uptake whereas metformin does so by suppressing glucose production needs to be reexamined.”
Effect of pioglitazone on abdominal fat distribution and insulin sensitivity in type 2 diabetic patients
“These results demonstrate that a shift of fat distribution from visceral to sc adipose depots after pioglitazone treatment is associated with improvements in hepatic and peripheral tissue sensitivity to insulin.”
I think the bone fracture risk was largely in women.
It’s hard to get away from the bladder cancer risk. Here is a 2018 meta-analysis that compute an OR of 1.84 in RCT’s and show evidence of both time and dose dependence. I was thinking of trying it to but given surveillance for bladder cancer is not great I don’t think I’ll go there. Bummer because I like that it significantly up-regulates Klotho as well.
Pioglitazone and bladder cancer risk: a systematic review and meta‐analysis - PMC
Looks like the 1.84 OR was not significant. Am I missing something?
95% CI was 0.99 to 3.42. So meta was pretty much significant. Both individual studies didn’t quite reach significance. Significance isn’t really binary anyway since even a 95% confidence leaves a 5% risk of being random. So call it significant with a 94.9% CI. The data showing correlation with dose and time is further support of cause → effect. Like I said given surveillance is insensitive or expensive it just doesn’t seem like a chance I would take unless there were more definitive studies.
There’s conflicting data on that. Earlier in this thread a study was posted showing the opposite, substantially higher risk for men, especially serious events.
Pioglitazone and Risk for Bone Fracture: Safety Data From a Randomized Clinical Trial
“Risk for serious fracture in the pioglitazone group compared with placebo was significantly elevated in men (5.4% vs 2.2%; HR, 2.34; 95% CI, 1.45 to 3.76) but not women (7.8% vs 6.4%; HR, 1.18; 95% CI, 0.76 to 1.83) (Supplemental Table 2 (283.1KB, docx) ). When serious fractures were restricted to low-energy, nonpathologic events, the risk remained elevated in men (3.8% vs 1.4%; HR, 2.64; 95% CI, 1.46 to 4.77) and was further reduced in women (6.6% vs 6.2%; HR, 1.03; 95% CI, 0.65 to 1.63). For both any serious fractures and low-energy, nonpathologic serious fractures, HRs for men were significantly higher than for women (P for interaction of treatment with sex = 0.04 and 0.01, respectively).”
Re: bladder cancer - both dose and duration were positively associated with increased incidence in pioglitazone users.
For me both fractures and bladder cancer are a concern. I will still go ahead and use this drug, but at a very low dose 7.5mg/day (see other posts in this thread regarding dosage), if empagliflozin and other measures don’t bring my A1c below the prediabetic range. The other thing, is I will try to limit the duration of exposure to get my A1c to 5.6 or below, and hopefully shift any visceral adipose tissue to less deleterious location, which will hopefully result in better insulin sensitivity. Then stop. If the glucose issues come back, I’ll do another spell of pio to get to target again. My hope would be that if I can limit exposure to, say, three months once a year, I can limit the corresponding risks. But of course plans are one thing, it will all have to be tested in practice. I intend to possibly go on pio 7.5mg October at the earliest.
I think this sounds like a reasonable plan. Given the bladder cancer and fracture risk I’ve put it on the back burner, but I think it’s still a good option for folks that are pre diabetic/diabetic that can’t resolve with SGLT2-inhibitors or other diabetic medications (or lifestyle).
I do wonder if the bone fracture and bladder cancer risk is due to PPAR-gamma activation or something else. Presumably you would have similar risks with Telmisartan and other partial agonists?
From the meta study:
“Pioglitazone exerts its anti‐hyperglycemic effects through activation of PPAR γ 1, which is highly expressed not only in adipocytes but also in several other tissues (e.g., urinary bladder) 47. Furthermore, PPAR γ is also expressed on cancer cells 48. It has been reported that activation of PPAR γ may alter tumor growth and progression in nonadipose cells 49. Preclinical research in rats showed that high doses of pioglitazone for 2 years increased risk of bladder tumors among male rats but not among female rats 50. Recently, one study performed on 120 mice showed that prolonged use of pioglitazone might induce significant abnormalities in several biomarkers and hematological indices associated with histopathological changes in the bladder, depending on dose 51. In accordance with the findings from animal studies, our meta‐analysis indicated that greater dose or longer duration of pioglitazone was associated with higher risk of bladder cancer, which supported the notion that pioglitazone’s risk of bladder cancer is dose‐dependent, in terms of cumulative dose or cumulative duration.”
I realize its a different mechanism but it seems metformin is a safe effective way to reduce glucose levels caused by overly active gluconeogenesis. Unless you’ve already tried that I think that might be a better option. Having a similar problem (fasting glucose usually ~100) I think I’ll first try metformin. I’ll admit pio is attractive for other reasons. I’m not suggesting you can’t reduce risk by using lower dose and time limitation but also you are unlikely to achieve your goal with a lower dose and what is the point if you can’t continue taking it?
I tried metformin for a year - did absolutely nothing for me. However, I used a 500mg/day dose, never higher. No side effects that I could tell, just no effect positive or negative. My FBS is usually around 108 mg/dL these days (until a few years ago, was in the 99-102 range), and A1c 5.8% (ranges from 5.7-5.9). Nothing moves it.
Regarding pioglitazone vs metformin for gluconeogenesis, it appears pioglitazone suppresses the production of glucose by the liver, but metformin does not. This was shown in the study I posted a few posts above:
As to the low dose pioglitazone 7.5mg/day, there appear to be studies showing it effective in lowering A1c and being a valid therapeutic dose for intended purposes. I posted a paper to that effect earlier in the thread:
It’s well worth reading, because it concludes that there’s almost no difference in measured benefits of the 7.5mg dose vs higher doses, but having much lower adverse effects. Of course, a giant caveat here - we all react differently to drugs. I may try the 7.5mg dose and it may do absolutely nothing for me, or I might have a bad reaction to pioglitazone. So this absolutely has to be verified in the real world with a given patient.
I’m interested in pioglitazone precisely because it suppresses gluconeogenesis (which metformin does not!), which I suspect is my problem. It also increases insulin sensitivity. That’s my interest. Other things like cardio protection is a bonus, but not something that’s a deciding factor for me, and futhermore, I believe odds are rapamycin will abolish the cardio benefits of pioglitazone (unless I take a rapa holiday for the three months or so of pio exposure). Again, all this is theory. How it will work in practice I’ll find out, should I move forward with pio.
FWIW, I’m trying to investigate whether low dose bisphosphonate concurrently with pioglitazone might not ameliorate at least some of the bone fracture risk - this is something that I’m doing a deep dive on currently. There is also a somewhat intriguing possible signal of bisphosphonates being mildly geroprotective, though obviously it’s a very thin ledge to go out on, as there are distinct risks too.
@CronosTempi Fair enough, I’m equally intrigued by Pioglitazone, just a little more worried about the bladder cancer risk. I still think if I were you I might try a higher dose of Metformin first, it should reduce fasting blood glucose even though I agree with you the data suggests it is not through an increase in insulin sensitivity.
I’ll have to read more of the paper you linked above, thanks for that link. Have you looked at bladder cancer risk (perhaps meta analysis) for patients on the 7.5 mg dose? That might help both of us feel better. I’ll keep a look out. Pioglitazone is an older drug so I’m guessing large studies using it are getting less common since the patent protection is done.
I’m going to re-listen to Attia’s podcast interview with Ralph DeFronzo (#337) but I think he recommends hitting the problem with pio, sglt2i, and glp1a. He’s pretty convincing and perhaps you are more likely to achieve success with adding sglt2i and glp1a as well? If you haven’t heard that interview I recommend it. Sorry if I haven’t thoroughly reviewed all the comments in this thread.
Thanks. Yes, that’s a great Ralph DeFronzo interview, that’s when I became interested in pioglitazone. I have not seen any data on the 7.5mg dose and bladder cancer, but note that this is lower than the lowest dose (15mg) used in the West, so there wouldn’t be much data. The 7.5mg dose is used in India as far as I know - I have even bought pioglitazone from India in the 7.5mg dose tablets. However, keeping in mind that both length of exposure and cumulative dose increase blader cancer, it would make sense for a lower dose to represent less risk. From the data it appears that the danger of bladder cancer climbs around 28,000mg cumulative dose - if you’re on 7.5/day that’s over 10 years ![]() - of course, length of time is a factor all by itself.
- of course, length of time is a factor all by itself.
And yes, I’m already on 25mg empagliflozin, so SGLT2i is covered. I’m staying away from GLP-1 drugs for now.
Dr DeFronzo comments on side effects of pioglitazone (40 min).
Bladder cancer is a “misconception” and osteoporosis is only a risk for post menopausal women.
Not sure if he’s right.
Pio discussion starts at 40 min:
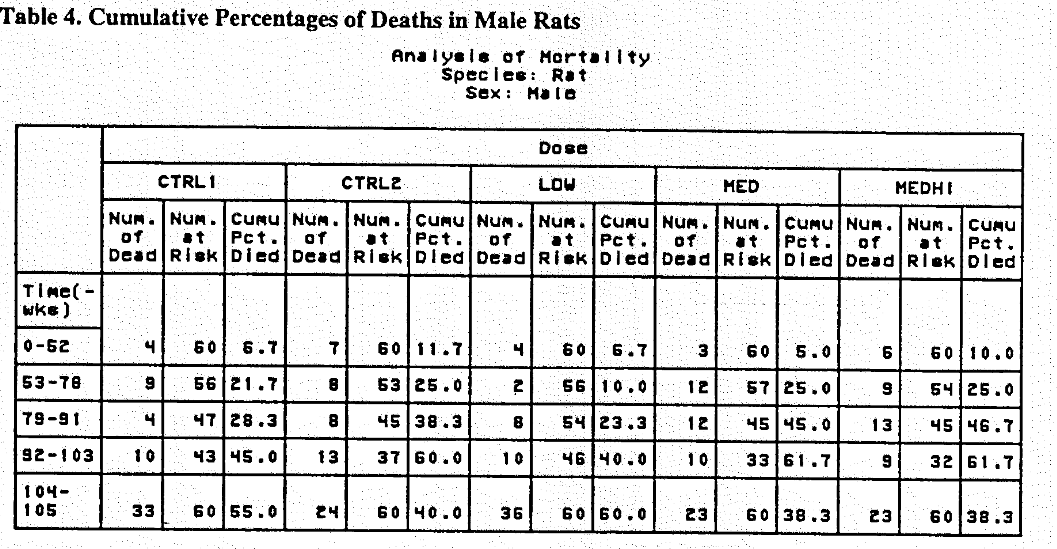
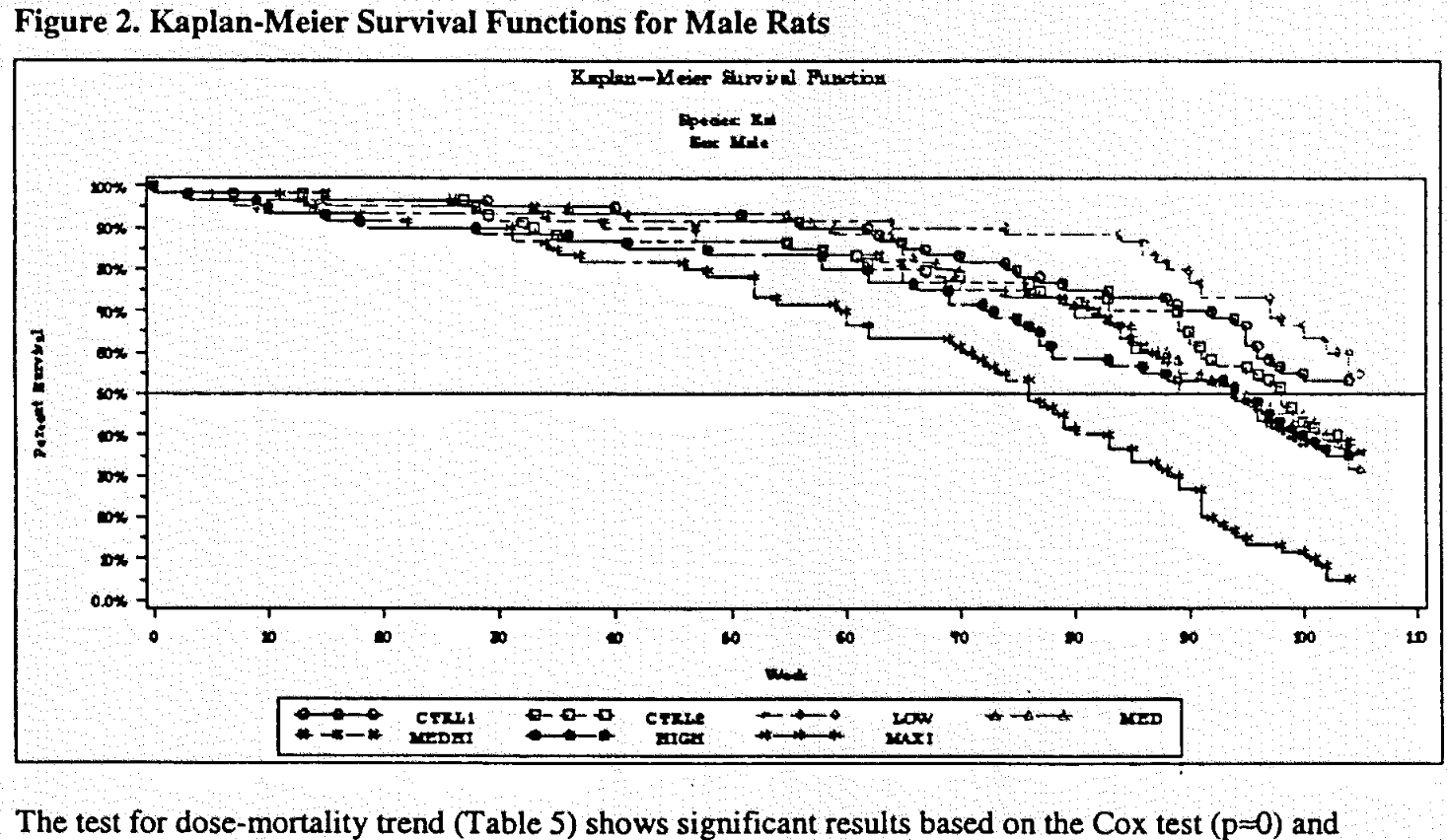
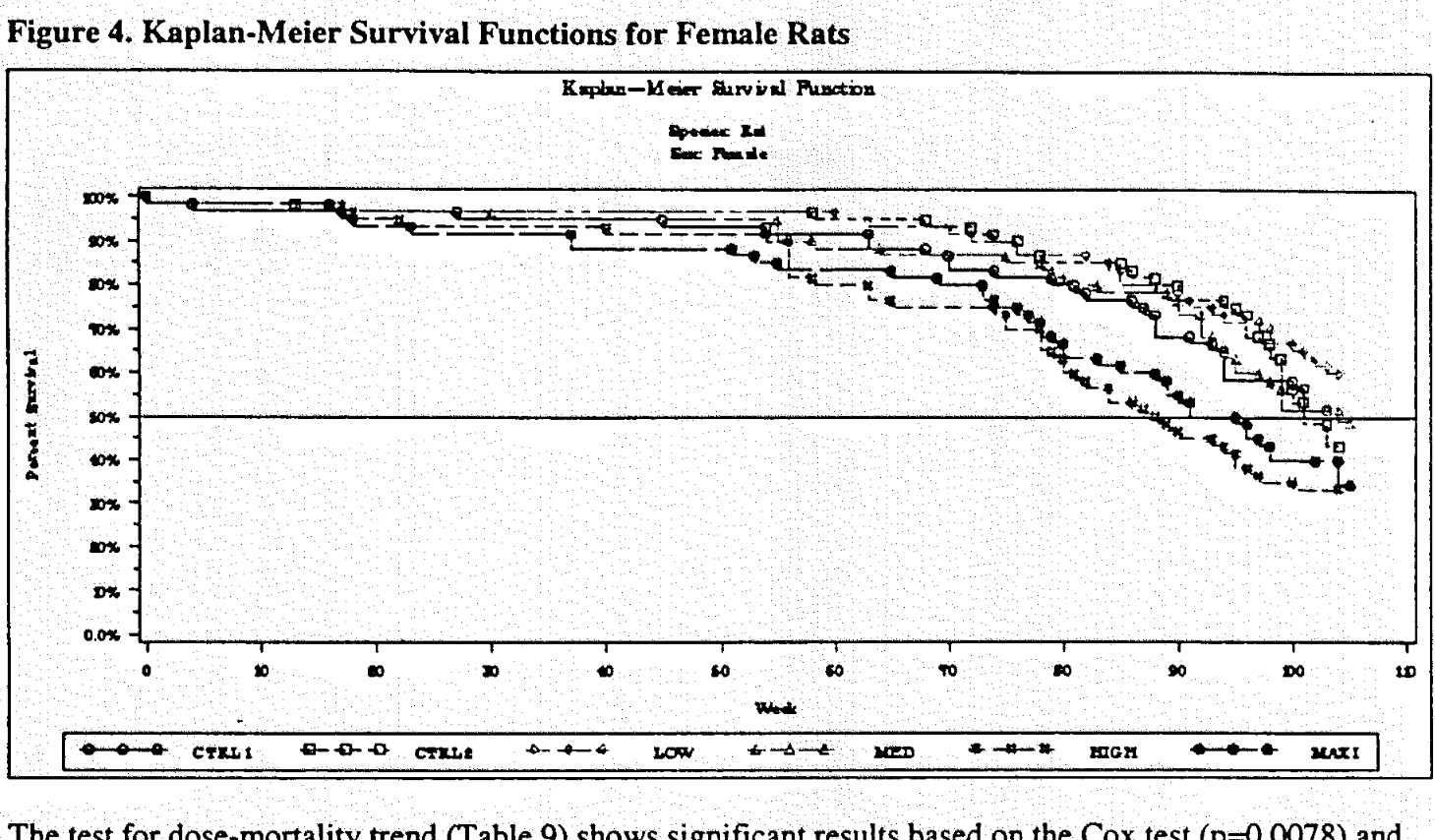
2 year lifespan studies in rats for pioglitazone?
(source: https://www.accessdata.fda.gov/drugsatfda_docs/nda/99/021073A_Actos_phrmr_P7.pdf)
(source: https://www.accessdata.fda.gov/drugsatfda_docs/nda/99/021073A_Actos_phrmr_P8.pdf)
I respect the heck out of Ralph DeFronzo, but he’s clearly wrong here. Bladder cancer is very real with increasing time and cumulative dose (28,000mg). And so is bone fracture risk, in fact esoecially among men. I posted the studies, solid RCT. No way around it. He might be operating on old information.
Again dose is important. However, the differences are not substantial, so hard to make definitive conclusions. Low/medium doses appear best, depending on sex. But one has to be particularly careful in using cancer mortality in rats/mice as the determinant, because cancer very frequently is triggered differently in humans and rodents - a good example was the thyroid cancer in rats on GLP-1RA, humans don’t have the type of cells in the thyroid that cause cancer in rats.
Bottom line, unfortunately, this doesn’t tell us much of anything about pioglitazone in humans long term.