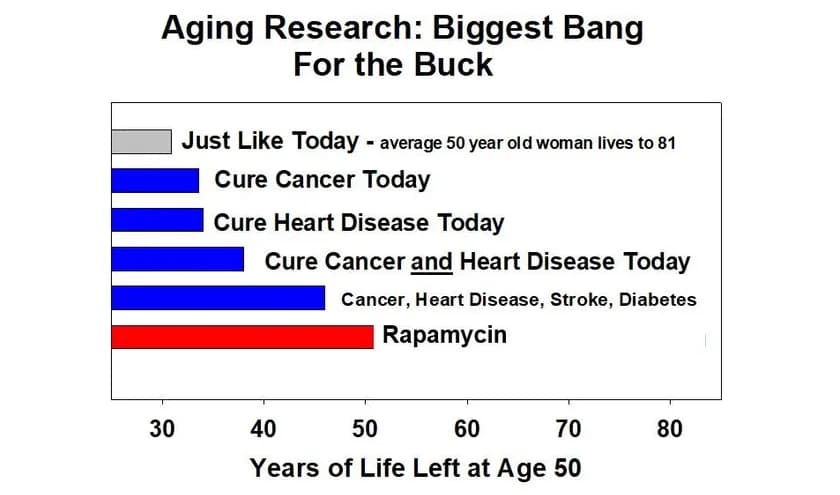
Richard Miller, the leader of the National Institutes on Aging Intervention Testing Program, has the above image on his lab website to emphasize the importance of research into the biology of aging, and the potential for age and disease prevention drugs like rapamycin (vs. the traditional “sick care” model focus of the NIH and US national healthcare system, in which they wait for disease to happen, and only then work on the care / disease of the patient). If rapamycin proves to be as effective in humans as it has been in mice, it will be a bigger impact than curing cancer, heart disease, stroke and diabetes. This is because, even if these cures were found, there are many other diseases that people would succumb to. By comparison the benefit of a preventative, age-slowing strategy such as may be possible with rapamycin, would delay all age-related diseases.
At Rapamycin News we believe the primary focus should be on prevention of disease (by slowing aging), and the data quite clearly show that this would provide the greatest benefit to the most people. Somehow the old adage of our grandparent’s age that “A ounce of prevention is worth a pound of cure” has been lost, and virtually all of the NIH budget of $49 Billion a year is spent on trying to identify that “cure”, while ignoring the role of prevention. This has to change as the global society ages.
The typical rapamycin user here pays perhaps $30 to $60 per month for their rapamycin (or approx. $7,000 to $14,000 for 20 years of rapamycin), and if the results seen in mice and other organisms transfers to humans then we can expect an additional 20 years of disease free healthspan and lifespan. Compare that to the $13,600 cost per day to stay in the typical US hospital and the economic benefits (to say nothing of the social benefits) are clear. If rapamycin keeps a person out of the hospital for just 1 day over 20 years, then the healthcare system as a whole is at break-even point. The potential for healthcare system savings of drugs like rapamycin is monumental given the annual national healthcare expenditures in the USA of $3,453 billion. The savings are even more immediately realizable in all the developed countries of the world that have national healthcare systems (Canada, Europe, Japan, etc. - every country other than the USA) because the single payer (the government) reaps the rewards/savings from disease prevention.
The National Institute on Aging sponsors the multi-institutional “Interventions Testing Program,” or ITP, to evaluate agents, such as drugs or nutriceuticals, that might slow aging and extend healthy lifespan in mice. The initial protocol focused on lifespan as the key endpoint. Agents that pass this screen are then evaluated in follow-up studies that include a wide range of age-sensitive tests, mid-life pathology, and ideas about mechanism of effect. More information about the program can be found here,including a list of drugs tested or in progress, links to tissues that can be provided for collaborations, and information about how to propose an intervention. Published work has documented major benefits from treatment with rapamycin, acarbose (males > females), and 17a-estradiol (males only), and smaller but significant benefits from three other agents (NDGA, Protandim, glycine).
For more information see: Drugs that Slow Aging (ITP)