I was so happy to learn about these two supplements to add to my Rapamycin 3mg a week is all I can manage to take but got my scan done and it shows that I am not losing and after just 5 months on the Rapamycin and two months on the other two supplements. Next goal is to retest and hope I am increasing in bone density…. My dr had nothing to do with these results but supported me on letting me do what I wanted and just stumbling onto this Rapamycin drug and this group has help me so much!!! Thanks a million.
Nice to hear Carmen! Can’t wait to see the next scan results.
I too have been helped with a variety of longevity questions, sourcing supplements and options to consider thanks to many on this site. We all move backwards (in time) together. Lol
A month ago, I was diagnosed with osteoporosis, and the report indicated that it appeared fairly severe. However, I have always been slim and small-boned, with a BMI of 18, and that naturally makes a difference. A person with a smaller frame and lower BMI is going to have less bone density than someone with a BMI of 25 or 30. It’s also important to remember that your T-score is a comparison to the average 30-year-old, while your Z-score is a comparison to the average person your age. Because of this, I was neither surprised nor shocked by the diagnosis, and I don’t feel the need to be in emergency mode. I don’t expect my bone density to ever match that of the average person, but I do intend to work on the problem.
I’m also not planning to change my lifestyle dramatically out of fear of a fracture. In my opinion, bone quality is more important than bone density, as long as the osteoporosis is not extremely severe. I’ve already researched the causes of osteoporosis and the ways bone density can be improved, and I plan to make only minor adjustments. My analysis showed that I was getting only about 60% of the recommended daily allowance for calcium, so I’ll be making small changes to my diet and supplements to correct that. In addition, I’ll be adding more high-impact exercise to my routine to help stimulate bone density. I expect this combination to make a meaningful difference.
I’m also considering “the big guns”—various peptides, SARMs, and hormones—as possible ways to improve bone density. This is a complex area, with many potential benefits as well as side effects, so it requires careful study. I’ve looked into the standard medications for osteoporosis as well, but I’m not convinced they’re necessarily better options than peptides, SARMs, or hormones. They also carry the risk of side effects, and some require follow-up treatment with a bisphosphonate after the main drug protocol is completed. The possibility of osteonecrosis, even if rare, is enough to make me wary of bisphosphonates.
During this research phase, I also sought out YouTube doctors who specialize in osteoporosis. I came across Dr. Doug Lucas. Like most others on YouTube, he is promoting his own services, but his 20- to 30-minute videos generally provide useful information, with only a brief mention of self-promotion. He covers a wide variety of topics, and I recommend taking a look.
Here is what ChatGPT found on bone-building drugs for osteoporosis for anyone interested. The most common first-line prescription is usually a bisphosphonate, but that is not a bone-building drug, so it is not included in this table.
Note: Strontium ranelate is banned in Europe.
| Drug (Brand) | MOA | T½ | Dose | Eff % | Bone Impact | SFX | Therapy / Follow-up | Antiresorptive Follow-up | Cost/mo | Ins. |
|---|---|---|---|---|---|---|---|---|---|---|
| Romosozumab (Evenity) | ↑Wnt, ↓resorp | ~12 days | 210 mg SQ monthly ×12 | 100 | ↑↑ BMD, ↓ spine/hip fx | HA, arthralgia, ↑CV (rare) | 12 months; follow with antiresorptive | Denosumab (Prolia, Xgeva) | ~$2,500 |
|
| Abaloparatide (Tymlos) | PTHrP analog | ~1 hour | 80 mcg SQ daily ×24 mo | 90 | ↑ BMD, ↓ fractures | Dizziness, nausea, osteosarc (rat) | 24 months; transition to antiresorptive | Denosumab (Prolia, Xgeva) | ~$1,600 |
|
| Teriparatide (Forteo, Bonsity) | PTH analog | ~1 hour | 20 mcg SQ daily ×24 mo | 85 | ↑ BMD, ↓ fractures | Cramps, nausea, osteosarc (rat) | 24 months; must follow with antiresorptive | Denosumab (Prolia, Xgeva) | $1,300–2,000 |
|
| *Strontium ranelate (Protelos) ** | ↑ formation, ↓ resorp | ~60 hours | 2 g oral daily | 80 | ↑ Spine/hip BMD, ↓ fractures | GI upset, HA, ↑CV (if risk) | Long-term use possible | N/A | $100–200 |
|
| Vit D3 + K2 (Thorne, LE, Pure) | ↑ Ca²⁺, osteocalcin | D3: 15h, K2: 3d | D3 2–5k IU + K2 90–200 mcg | 50 | ↑ Remodeling, ↓ fractures | None or ↑ Ca (rare) | Continuous adjunct | N/A | $15–30 |
|
Good chart: except – no one should take strontium ranelate. It has been banned in Europe because it is carcinogenic. The problem is not the strontium – it is the ranelate. In the US, strontium is available OTC as strontium citrate.
Read the “COMB” study: “combination of micronutrients for bone.” recommends calcium, K (consider both K2-7 and K4),D, and calcium citrate.
Consider a linear vertical vibration plate. Must be vertical (up/down, not side-to-side)
@Agetron. Just had a DEXA scan done. My hip is normal, but my leg T score is -1.3. I take Taurine, Vitamin K, Boron, creatine and D3. The doctor recommended taking calcium and doing some leg exercises. I don’t take calcium, but I guess I need to start.
Bummer. But I wonder how could my pelvis be fine but my legs not?
Apparently, calcium supplements can aggravate heart disease.
From google …
Calcium supplements are linked to an increased risk of coronary heart disease (CHD), likely due to calcium deposits that clog and stiffen arteries. In contrast, dietary calcium intake from foods like leafy greens and dairy products is associated with a lower risk of heart disease. Therefore, it’s recommended to obtain calcium from food sources rather than supplements, especially for individuals at risk of osteoporosis. [1, 2, 3, 4, 5, 6]
How Calcium Supplements May Harm the Heart
Ectopic Calcification: High circulating calcium levels from supplements can lead to “ectopic” or out-of-place calcium deposits in the arteries and other soft tissues, contributing to coronary artery disease.Vascular Stiffness: Calcium deposits can stiffen the arteries, making them less flexible and potentially interfering with their function.Increased Risk: Studies, including meta-analyses of randomized controlled trials, have found that calcium supplements are associated with an increased risk of myocardial infarction (heart attack) and stroke, particularly in postmenopausal women.
The Role of Dietary Calcium
Lower Risk: Calcium consumed from food sources has been linked to a decreased risk of coronary heart disease.Benefits of Food Sources: Foods rich in calcium, such as low-fat dairy, leafy green vegetables, and beans, provide a “cocktail” of beneficial nutrients and minerals that are processed differently by the body than the large doses from supplements.
Recommendations
Prioritize Diet: Get the majority of your calcium from food rather than supplements.Consult a Doctor: Discuss any calcium supplementation with your physician, especially if you are at risk for osteoporosis or are already at high risk for heart disease.Consider Vitamin D: While not a replacement for dietary calcium, vitamin D supplementation may be considered alongside calcium to aid bone health, though its effect on cardiovascular risk is debated.
AI responses may include mistakes.
[1] https://www.health.harvard.edu/blog/study-links-too-much-calcium-to-heart-disease-20100812204
[2] https://www.sciencedirect.com/science/article/abs/pii/S1443950623042816
[3] https://pmc.ncbi.nlm.nih.gov/articles/PMC7276095/
[4] https://www.youtube.com/watch?v=Enr9upwhoxc
[5] https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/1568524
Yes. I wasn’t planning on taking supplements, but I need to incorporate higher calcium foods into my diet. For instance, more Greek yoghurt.
However, I have to balance the risks of dairy for my prostate. I don’t want to get cancer by avoiding osteopenia. Maybe just a lot more leafy greens, but I honestly thought I was eating enough of those!
Almonds supposedly have a lot of calcium too, and I eat handfuls of those a day. So maybe it’s not the calcium I’m lacking.
Looking at my blood work, it seems like more copper could be useful.
None of it makes sense to me, but I’ll share that, due to improvement, my hip is no longer osteoporosis/osteopenia, but my femur and spine are… so it tracks that your parts are not all the same.
Interestingly, it was just yesterday my husband was talking to an aprox 50 yo man who has osteopenia. He learned he broke his hip, and then at another time, he broke his femur. His doctor eventually tested his thyroid and that was his problem.
I am hypothyroid and it was the first time I learned that thyroid levels, hypo or hyper, can affect our bone health. So, on that note, if you haven’t, do check. I have learned this is not standard, especially for men.
@Elizabeth_Kirby I had always heard not to take calcium, but last fall when I was diagnosed with osteoporosis, my two doctors both encouraged me to take calcium, and I even ran it by two cardiologists… (yes, I was THAT nervous). FWIW, all of them said to take it. I take it with d and a lot of k. Fingers crossed this is causing no harm!
@DeStrider Also, I was eating vats of kale and almonds, but those were not enough for me ![]() I have no idea if the supplment makes a difference, though ?
I have no idea if the supplment makes a difference, though ?
Actually, I have a strong suspicion that my osteopenia is related to my incredibly low levels of free testosterone. So I have to solve that problem. Right now, I am only taking DHEA to do that. I may need to try something stronger.
Consider pregnenalone, which comes in at a different place upstream in the hormone synthesis pathway than DHEA. (Some of us use both DHEA & pregnenalone to cover more of the pathway.) Or you could get testosterone supplementation. (Though that requires a willing and certified doc, whereas DHEA & pregn do not.)
When I looked into the calcium heart thing, I got the impression that it’s a timing thing. That is, if the body gets a blast of calcium, it stores it whereever it can, including in plaque. If it’s trickled in, it stores it in bone.
So I still do take calcium, but a small bit of powder mixed in with food. I’m hoping that is a good enough mimicry of a trickle to help & still avoid the blasting too much at once thing.
What was your free T? I also have osteopenia, follow a perfect diet with boron, vit k, etc my spine improved but my femur didnt.
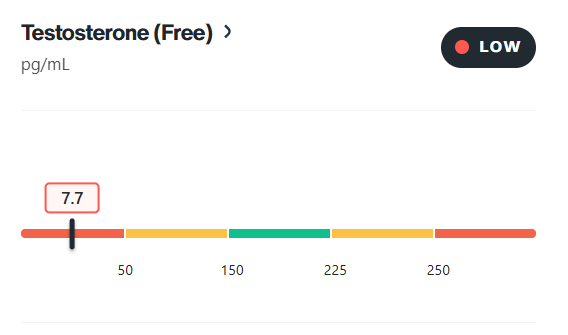
I believe his level is around 95 pg/mL. I’ve seen his results posted on X before, but I can’t seem to find them again. I remember comparing it to my own results, which were quite high at 274 pg/mL.
Thank you for the correct numbers. I had gotten my numbers from a Siimland video, and it may have been European units. I guess I have my work cut out for me to raise my free testosterone.
Btw, is your total T okay?
My total T is in range at 579 Ng/DL. I just don’t have enough freeT
Is your SHBG high? How about estradiol or thyroid levels? Do you do resistance training?
Keep in mind that bioavailable testosterone may be a better measure than free T alone, some testosterone is bound to albumin, but it’s still usable by the body.
Also worth noting: the combination of metformin, empagliflozin, and dutasteride can significantly raise SHBG. That could explain why your free T is disproportionately low, even though your total T looks solid if your SHBG is elevated.
SHBG - in range, but on the low side of optimal.
All thyroid markers are in range or optimal. Albumin is optimal.
I don’t do regular resistance training (but I should).
I feel like my blood report is a detective mystery. What lowered (killed) my free Testosterone, and which medication(weapon) is the culprit? ![]()