Ursodeoxycholic acid (UDCA), also known as ursodiol, comes from bear bile and has been used in traditional Chinese medicine since the 7th century. It has been used in Western medicine since 1955 to dissolve gallstones. Ursodoxicoltaurine or tauroursodeoxycholic acid (TUDCA), also known as taurursodiol, is the taurine conjugated form of UDCA.
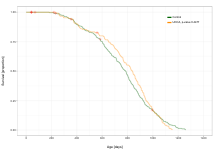
UDCA failed the ITP: Longer lifespan in male mice treated with a weakly estrogenic agonist, an antioxidant, an α-glucosidase inhibitor or a Nrf2-inducer 2016. However, they noted:
Treatment with the bile acid, UDCA, has been reported to have a wide variety of effects that are compatible with extended lifespan in mammals, including protecting against metabolic derangements such as diabetes, and suppression of tumor formation (Oyama et al., 2002; Lukivskaya et al., 2004). Nevertheless, no previous lifespan studies have been reported for UDCA. At the dose used in this study, there were significant reductions in body weight across the lifespan in both male and female mice, suggesting that UDCA treatment had biological or physiological effects. However, there was no effect of UDCA on median or maximal lifespan in either sex. Given the wide range of positive effects reported for UDCA on measures of healthspan, it is unclear why it had no effect on lifespan. It is possible that higher or lower doses of UDCA may be effective. On the other hand, as we observed with NDGA in the present study, the effects of specific interventions on lifespan may be distinct from effects on age-sensitive physiological changes in specific organ systems.
In males, UDCA treatment showed early protective effects during pre-median lifespan stages but at later ages manifested significant negative impacts: MPD: ITP survival analysis: ursodeoxycholic acid
They used 5,000 ppm = 833 mg/kg (mice) => ~67 mg/kg in humans (HED). So, about 5 g/day for the average adult. 67 mg/kg is a lot. UDCA in a dose of 28–30 mg/kg/day increases the risk of death and need for liver transplant by 2.3-fold among those with primary sclerosing cholangitis, despite a decrease in liver enzymes: High Dose Ursodeoxycholic Acid for the Treatment of Primary Sclerosing Cholangitis 2010
The normal UDCA dose for gallstones is about 10 mg/kg, typically 750 mg/day (DDD, according to the WHO).
The prevalence of gallstones is approximately 10–15% of adults in Europe and the US: CKS is only available in the UK | NICE
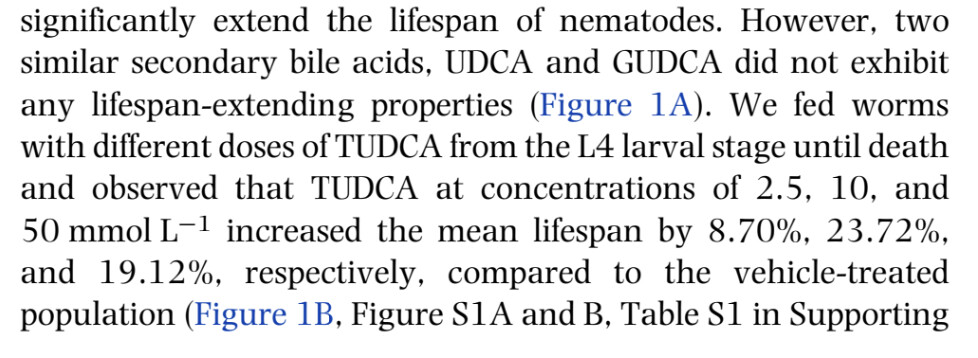
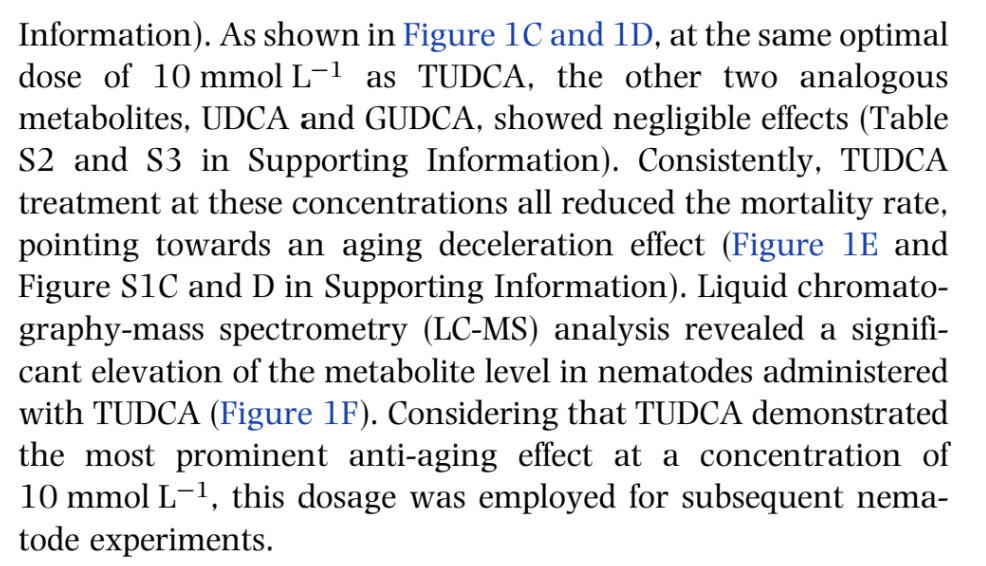
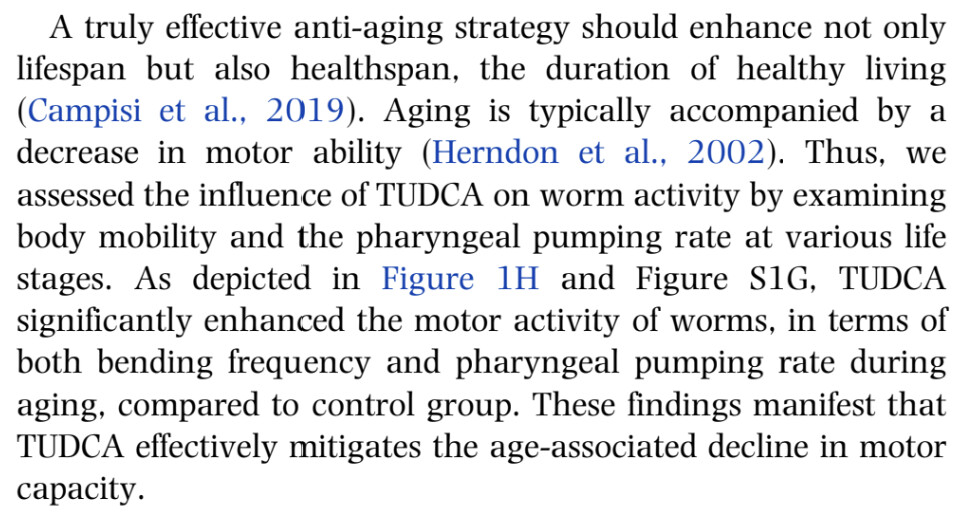
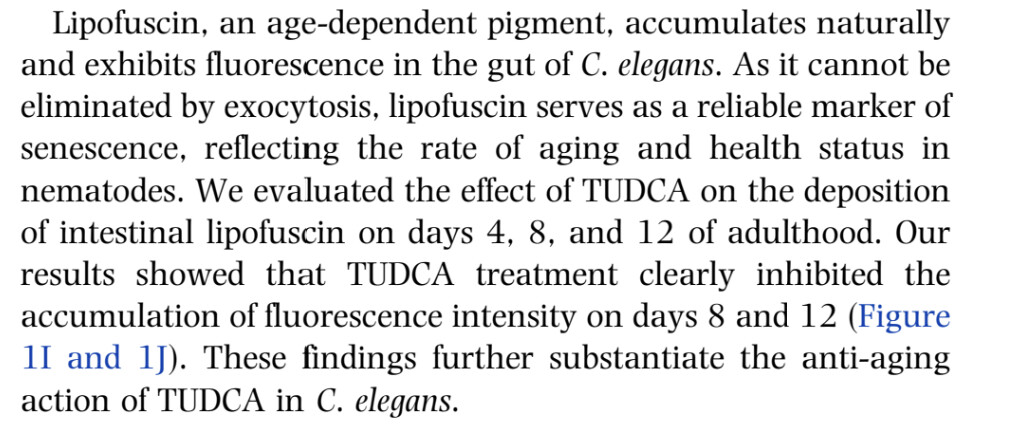
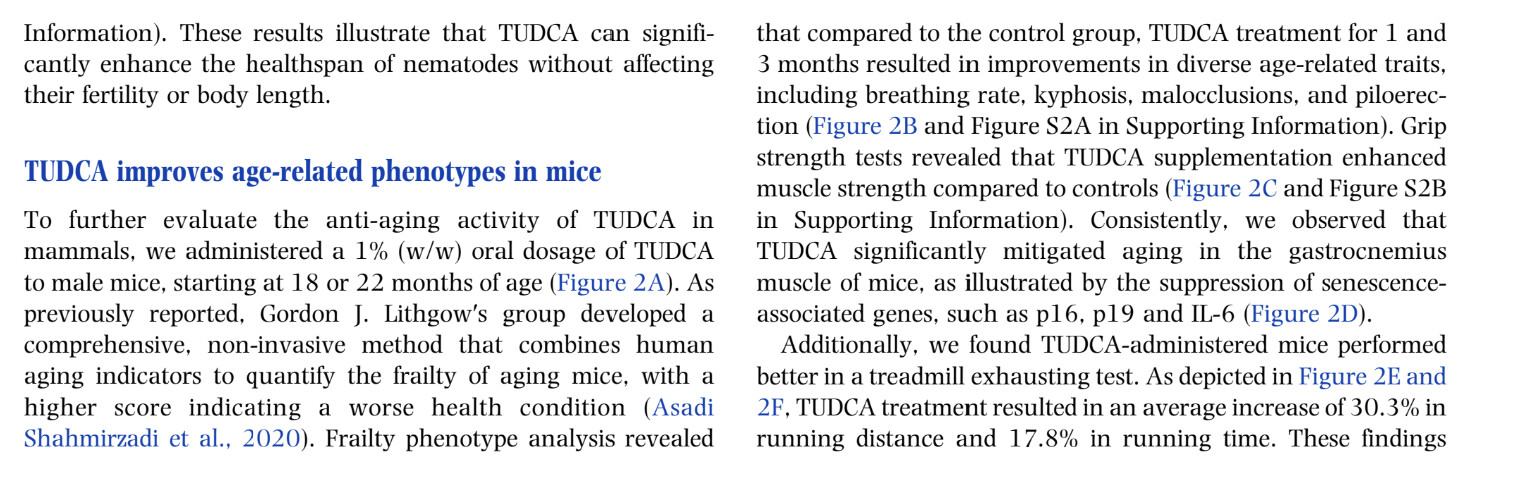
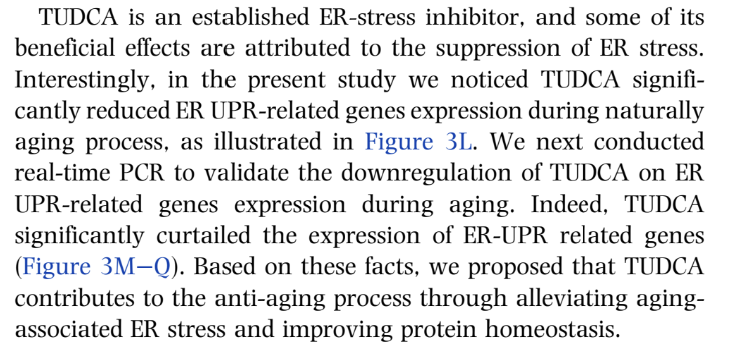
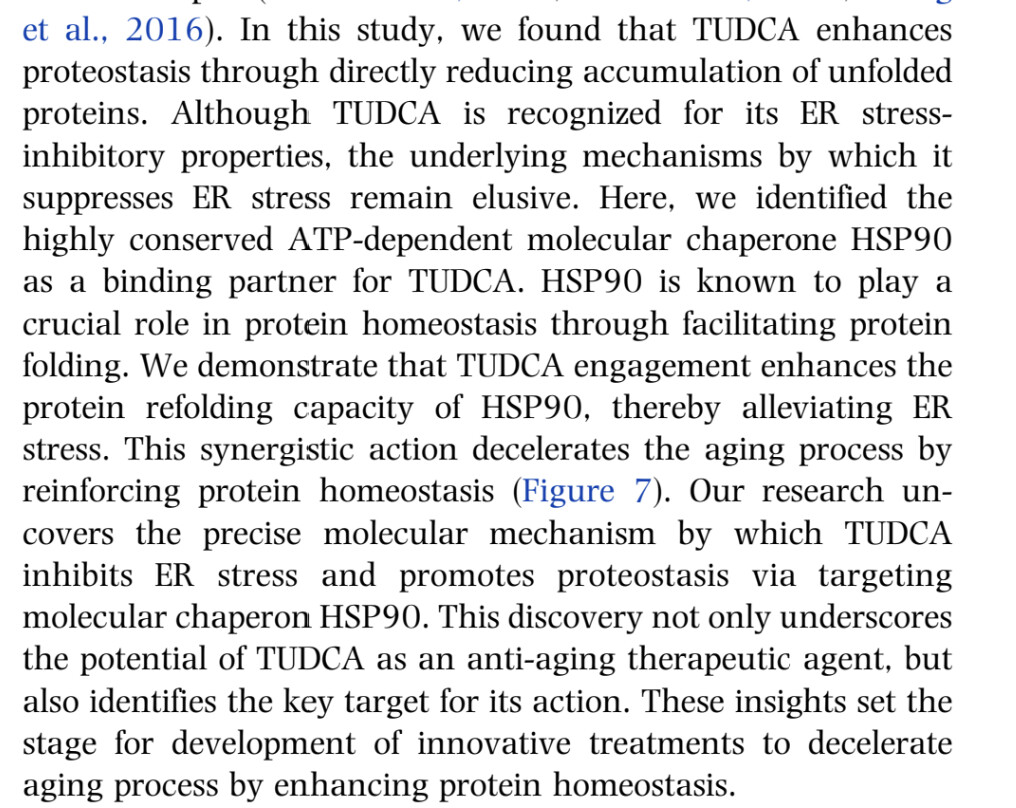
A recent Chinese paper claims that: Tauroursodeoxycholic acid targets HSP90 to promote protein homeostasis and extends healthy lifespan 2024
TUDCA extends the lifespan and healthspan of C. elegans . Importantly, oral supplementation of TUDCA improves fitness in old mice, including clinically relevant phenotypes, exercise capacity and cognitive function. Consistently, TUDCA treatment drives broad transcriptional changes correlated with anti-aging characteristics. Mechanistically, we discover that TUDCA targets the chaperone HSP90 to promote its protein refolding activity. This collaboration further alleviates aging-induced endoplasmic reticulum (ER) stress and facilitates protein homeostasis, thus offering resistance to aging. In summary, our findings uncover new molecular links between an endogenous metabolite and protein homeostasis, and propose a novel anti-aging strategy that could improve both lifespan and healthspan.
(I’ll try to replicate their findings with Ora Biomedical.)
This Brazilian paper found: The bile acid TUDCA reduces age-related hyperinsulinemia in mice 2022
Here, we evaluated the actions of TUDCA upon glucose-insulin homeostasis in aged C57BL/6 male mice (18-month-old) treated with 300 mg/kg of TUDCA or its vehicle. TUDCA attenuated hyperinsulinemia and improved glucose homeostasis in aged mice, by enhancing liver insulin-degrading enzyme (IDE) expression and insulin clearance. Furthermore, the improvement in glucose-insulin homeostasis in these mice was accompanied by a reduction in adiposity, associated with adipocyte hypertrophy, and lipids accumulation in the liver. TUDCA-treated aged mice also displayed increased energy expenditure and metabolic flexibility, as well as a better cognitive ability. Taken together, our data highlight TUDCA as an interesting target for the attenuation of age-related hyperinsulinemia and its deleterious effects on metabolism.
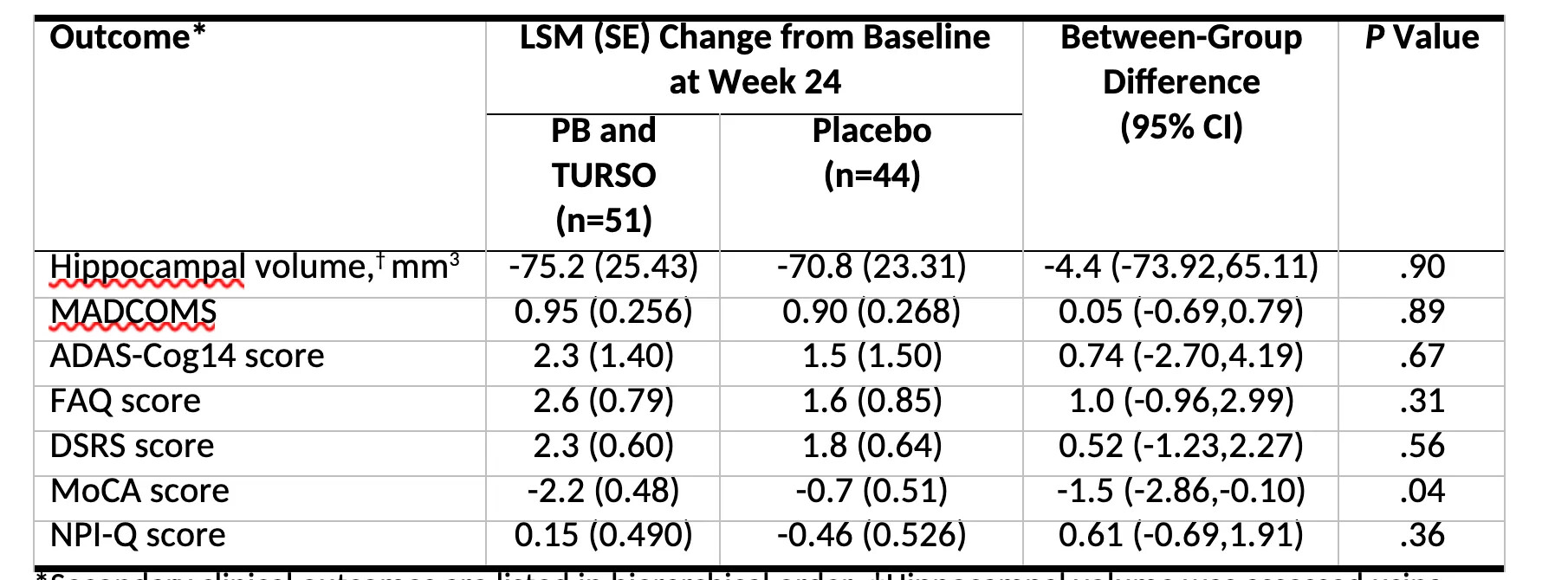
So, it’s been speculated that UDCA and TUDCA could have neuroprotective effects. However, this year, a combination including TUDCA famously failed in ALS and was withdrawn from the market: https://www.nytimes.com/2024/03/08/health/als-drug-relyvrio.html
There’s an upcoming trial in Parkinson’s disease using UDCA 2.5 g/day: Parkinson's disease - #342 by adssx This trial follows a small one using 30 mg/kg: A Double-Blind, Randomized, Placebo-Controlled Trial of Ursodeoxycholic Acid (UDCA) in Parkinson’s Disease 2023:
The UP Study has confirmed that UDCA at a dose of 30 mg/kg is safe and extremely well tolerated in PD with no SAEs and only mild, transient side effects reported in the UDCA treatment group (primary outcome). This is reflected by the high compliance rate (mean of 97.6%) of those participants in the UDCA-treated group who completed the full treatment duration.
In contrast, we observed either an improvement in the UDCA treatment group or comparatively less worsening in gait over the treatment period.
The action of UDCA might be pleiotropic and is yet to be fully elucidated. Changes in the PD gut microbiome are associated with alterations in the bile acid pool. Intriguingly, reductions of (endogenous) UDCA and TUDCA have been reported in an experimental model of prodromal PD; in addition, UDCA treatment partially restores the gut microbial profile in other conditions.48-50 A beneficial effect of UDCA in PD may therefore not be limited to mitochondrial rescue but also an additional, as yet speculative, effect on the microbiome and the gut–brain axis.
Some bodybuilders apparently take TUDCA to reduce muscle fatigue and improve performance: Tudca: 5 Key Benefits For Bodybuilders & Liver Support – NutraBio Brands (any thoughts on this @LukeMV?)
Eric Berg doesn’t provide sources but claims that TUDCA has a lot of benefits: Benefits of TUDCA: Benefits of bile salts on gut health ![]()
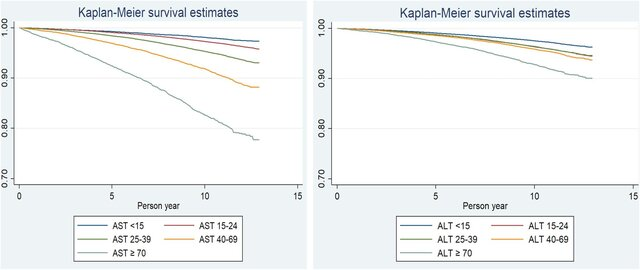
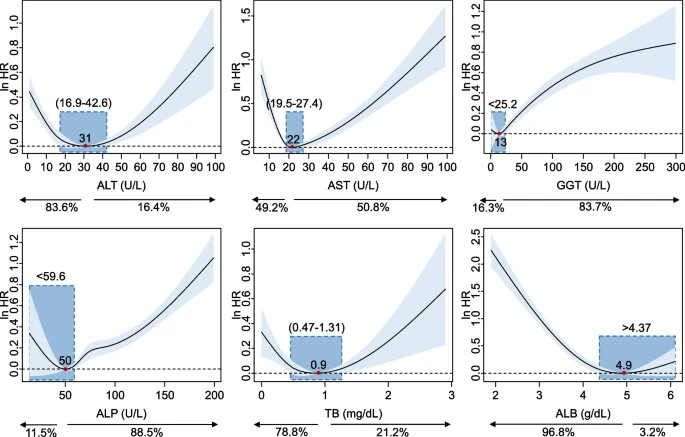
What is clear is that UDCA (and TUDCA?) significantly reduce serum liver parameters: alanine aminotransferase (ALT: –15 U/L), aspartate aminotransferase (AST: –16 U/L), gamma-glutamyl transferase (GGT: –23 U/L), alkaline phosphatase (ALP: –94 U/L) and bilirubin (–0.2 U/L): Effect of ursodeoxycholic acid on liver markers: A systematic review and meta-analysis of randomized placebo-controlled clinical trials 2020
It seems that for all-cause mortality, the lower, the better for ALT and AST: Loss of Life Expectancy by 10 Years or More From Elevated Aspartate Aminotransferase: Finding Aspartate Aminotransferase a Better Mortality Predictor for All-Cause and Liver-Related than Alanine Aminotransferase 2019
Same for GGT: Gamma-glutamyl transferase and risk of all-cause and disease-specific mortality: a nationwide cohort study 2023
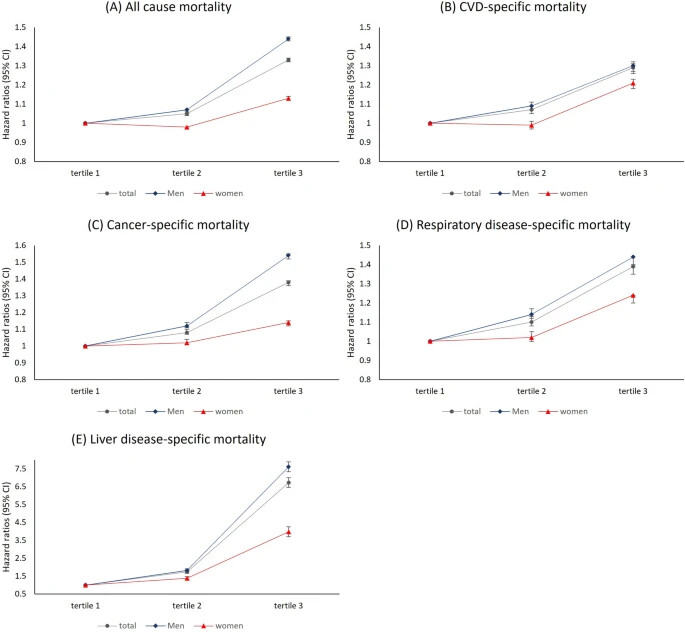
Level of serum GGT was categorized by sex-specific tertiles as follows: low tertile (< 25 IU/L), middle tertile (25–43 IU/L), and high tertile (≥ 44 IU/L) for men and low tertile (< 14 IU/L), middle tertile (14–20 IU/L), and high tertile (≥ 21 IU/L) for women.
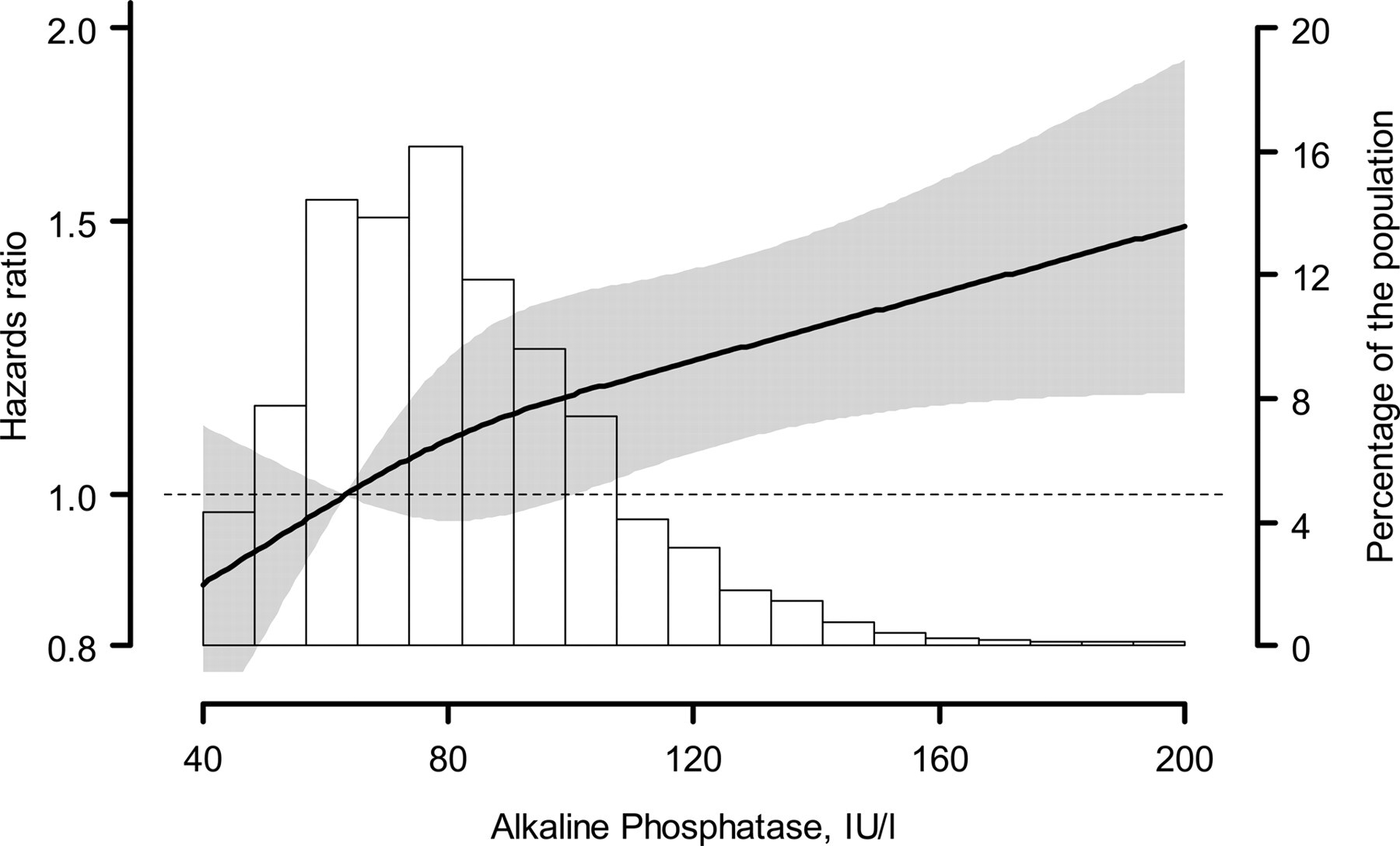
Same for ALP? Relation Between Alkaline Phosphatase, Serum Phosphate, and All-Cause or Cardiovascular Mortality 2009
However, another paper found J-shaped correlations: Associations between serum levels of liver function biomarkers and all-cause and cause-specific mortality: a prospective cohort study 2024
So I wonder:
- If one has elevated serum liver markers, is (T)UDCA the best intervention?
- If so, when should one start the intervention? (AST > 40? ALT > 70? ALP > 60?)
- Is there a case for UDCA or TUDCA beyond liver marker optimization?