For some years I had been using Sulforaphane several times a week. Sometimes as Avmacol but mostly with sprouts and heating them to 158 deg F. prior to consumption as per Jed Fahey and R. P. My thought was to increase NRF2 expression, I never thought about being an mTOR inhibitor. I was surprised to read the other day that Sulforaphane is a stronger mTOR inhibitor as compared to Rapamycin. I was unaware of that fact. It would be pretty important to consider if taking both as you may not want to risk overdoing mTOR inhibition as this could be counter productive. I do get some side effects from Rapa (sleep issues, some fatigue and scalp acne). I never had these issues with Sulforaphane. Rapa does seem to really lower inflammation markers to a much greater level than sulforaphane (just looking at bloodwork with CRP), and it also seems to alter WBC counts. I wonder what other peoples thoughts are as to one vs the other. mTOR inhibition is always discussed with rapa but if that is the goal an easy alternative could be SFN.
Sorry, not answering your question but research BROQ, much higher levels of Suforaphane than Avmacol.
Co-signed on the BROQ being more potent than Avamacol. It isn’t cheap but if you’re just using it three times a week, it’s more cost effective.
I was not aware of its mTOR lowering capabilities but I do think it’s one of the most under-researched supplements with major potential just waiting to be uncovered. I would make the sprouts but I’m a little too lazy to do all that.
I don’t see anything suggesting sulforaphane is a stronger mTOR inhibitor than rapamycin. Here is what I see.
| Property | Rapamycin | Sulforaphane |
|---|---|---|
| Binding | Direct FKBP12–mTORC1 inhibitor | No direct binding; upstream AMPK/Akt effects |
| mTORC1 suppression | 80–95% in target tissues | 20–50% in responsive cells |
| mTORC2 effect | Indirect with chronic dosing | No clear consistent effect |
| Duration | Days to >1 week after single dose | Hours after ingestion |
| Selectivity | mTOR-focused | Multi-target: Nrf2 activation, HDAC inhibition, redox signaling |
| Geroprotective overlap | High (direct mTORC1 suppression) | Moderate (partial mTORC1 suppression + other cytoprotective pathways) |
Based on comments here, I looked at BROQ. I did not know about it. The mechanism for delivering sulforaphane seems sound – based on well-studied sulforaphane pathways – and validated in vitro for stability and delivery. Nonetheless, I could find no independent clinical trial data that directly evaluates its physiological effects in humans. Its claims are inferred from the general literature on sulforaphane.
Before placed confidence in this expensive product, I would want to see at least one well designed and executed independent study conducted on healthy adults or mild metabolic syndrome taking BROQ (25 mg SFN) vs placebo for 4–8 weeks. Primary endpoints might be Nrf2 target gene expression (NQO1, HO-1, GCLC) in PBMCs and plasma/urinary SFN and dithiocarbamate metabolites. Secondary endpoints might be CRP, IL-6, and maybe oxidative stress markers (F2-isoprostanes, 8-OHdG). Based on what I can see, I would expect affirmative results but they do not appear to exist at this time.
I always thought Sulphorophane main activity was through Nrf2, not mTOR, though I’m not entirely positive about that. But still, one is a well-researched, powerful prescription drug manufactured under GMP conditions, and the other is a supplement where the purity, activity etc is far less known. (Though I do think the Avmacol would be the best option in terms of probably actually getting what it says on the bottle)
Thank you gents for your thoughtful replies. Rob T I like the chart that you had. I tend to agree that while SFN does significantly inhibit mTOR that it is not a stronger inhibitor of mTOR than rapa. The half life is much shorter. From what I can find the half-life if SFN is about 1.9 hours. Jed Fahey was at Johns Hopkins where they did much of the initial work on its action. He said that most of the studies that they did they used the Avmacol because it is a tricky molecule because the glucoraphanin has to react with the myrosinase at the time of consumption and cant be stored in the form of SFN. They had tested the Avmacol and it checked out to have the active ingredients. He said that many formulations did not check out as having what they purported to have. The NRF2 aspect of it seems very beneficial to help clear toxins that build up in tissues, and they have a lot of solid data to show that it works well in that aspect.
I’m still working through this as I have been taking Life Extension’s formulation for several years without knowing exactly how much SFN I was getting. I had GPT 5.0 produce this table. One next step would be to calculate a mg/dollar value. Some sources are much more variable in their effect than others, so there is that to consider. :
Estimated SFN Yield – Clinical or PK-Based Ranges
| Product / Source | GR dose (mg) | Myrosinase? | Conversion efficiency (typical) | SFN yield (mg) | SFN yield (µmol) | Notes |
|---|---|---|---|---|---|---|
| BROQ (stabilized SFN) | N/A (pre-formed SFN) | N/A | N/A | 25 mg | 141 µmol | Delayed-release capsule; bypasses conversion. Bioavailability reported ~90–100%. |
| Avmacol (2-tablet clinical dose) | ~34–40 mg |
|
35–70% | 5–11 mg | 28–62 µmol | Range from Fahey et al., 2015 urinary metabolite data; large inter-individual variation. |
| TruBroc (38.5 mg GR, no myrosinase) | 38.5 mg | ✘ | 1–10% | 0.16–1.56 mg | 0.9–8.8 µmol | Gut microbiota conversion only; highly variable. |
| TruBroc + myrosinase (Life Extension “Optimized Broccoli with Myrosinase”) | 30–40 mg GR (typical LEF dose ~35 mg) |
|
35–65% | 4.8–10.2 mg | 27–58 µmol | Estimate based on GR content and typical conversion rates seen in GR+myrosinase studies. |
| 100 g raw broccoli florets (mid-range GR content) | ~200 mg |
|
20–40% | 8–16 mg | 45–90 µmol | Wide cultivar and storage variability; ~5–50% lower yield if cooked. |
| 10 g high-GR broccoli sprouts | 200–500 mg |
|
20–40% | 16–40 mg | 90–226 µmol | Can exceed BROQ in high-end cultivars; also high inter-batch variability. |
FWIW: It appears to be affected by the form taken.
In any case it should be gone from the system after 24 hrs.
ChatGPT 5 thinking:
So, did I miss a discussion about possible synergy between taking sulforaphane and rapamycin? Currently I am dosing with rapamycin once weekly.
Could I add sulforaphane to increase mTORC1 suppression for a short time? Or could I add sulforaphane and take a smaller dose of rapamycin? This could be a plus for people who want to conserve their supply of rapamycin instead of using GFJ. As I’ve mentioned before, I’m attempting to strike a balance between my exercise regimen and my rapamycin intake.
This is a good point and one I had not thought of when comparing the sources in the above table. Therefore (I think) BROQ delivers free sulforaphane (SFN), so systemic clearance is governed by human SFN pharmacokinetics, not the brand. A delayed-release capsule can shift Tmax (where/when absorption starts), but it won’t change the elimination half-life once SFN is in circulation. In contrast, because conversion unfolds in the intestinal lumen over hours, formulations such as Life Extension’s would produce a broader, lower peak with a somewhat longer “tail” for the same nominal SFN yield, even though once SFN is absorbed its t½ is still ~2 h. A third option, possibly the best, might be BROQ BID.
Charles, It does seem that they both inhibit mTOR, but I guess I would be a bit cautious of taking them together myself. It just seems that together you would be adding too many possible synergies or unknowns. Maybe a cycle of rapa and then a cycle of SFN. I am just thinking out loud here. For me I get more side effects from rapa than I do with SFN, so I can use the SFN more regularly.
I take sulforaphane several times a week, Broccomax, usually 2 capsules, and always at night. It’s not the most potent sfn supplement, but it is reliable and cost effective. I take it if/when I awaken because it reliably makes me fall back asleep. When I used to have H. Pylori, Sulforaphane would cause me some stomach cramping. There are studies showing that it has activity against h pylori, so I imagined that there was a battle going on in my stomach. I like the idea of taking it at night on an empty stomach.
My question to the forum is whether sulforaphane makes anyone else sleepy?
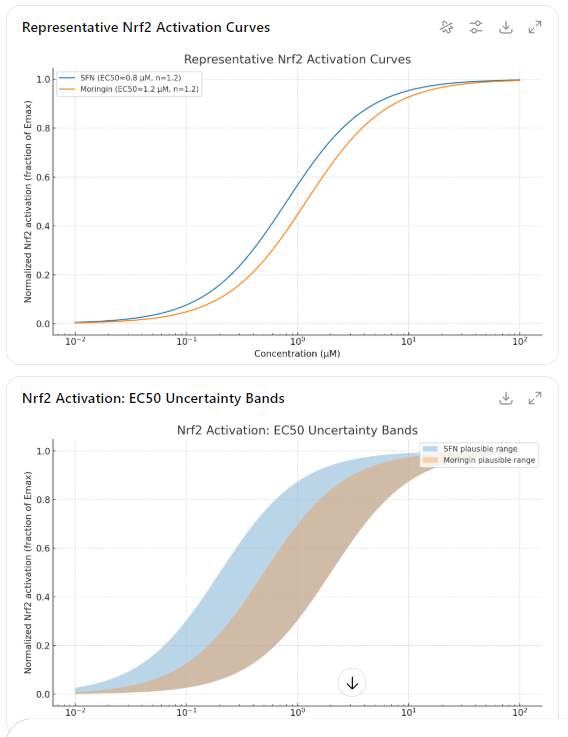
Another way to stimulate something similar to Sulforaphane, according to Jed Fahey, is Moringa. The chemical is Moringin. If you live in a place with little to no freezing, it’s incredibly easy to grow. I used to grow broccoli sprouts, but Moringa is so much easier. I grow it in a pot and simply add the leaves to a smoothie, though you could also toss them into a salad or mix them with greens. Happy Nrf2 pathways!
No, I wish it did because I take mine (was using Broccomax, now upgraded to Broq) at about 3am when I get up to go to the bathroom.
Are your inflammatory metrics high? Sulforaphane can have a mild tiring effect in such cases, particularly if taken on an empty stomach.
Thank you for the tip on Moringa @Tom_Wallace. There are some notable differences in other areas but the Nrf2 curves are fascinating – and it is apparently more stable.
No, not that I’m aware of. I’m intrigued now. Where did you learn that and which inflammatory markers should I be testing? Thanks!
I recall coming across a few related points in my reading. The argument is that because SFN is a potent Nrf2 activator and NF-κB suppressor, downregulation of pro-inflammatory cytokines (e.g., TNF-α, IL-1β, IL-6) can alter central fatigue pathways — cytokine shifts are known to influence arousal, especially in illness recovery phases. For people with high baseline inflammation, an acute shift might transiently produce a “let-down” or sedative-like feeling. I seem to recall a different reference to fatigue but can’t recall where I read it.
Good news for those of us who experience improved sleep after taking SFN! Here is an article about a study that shows that SFN increases melatonin levels and decreases inflammatory response in healthy adults.