Several articles were published this week in the prestigious European Heart Journal on (mostly high-dose) statin monotherapy vs (mostly low-dose) statin + ezetimibe combination (or some variations). I thought a dedicated thread could be useful.
Efficacy of lipid lowering therapy beyond statins to prevent cardiovascular events (Germany)
Treatment with ezetimibe or a PCSK-9 inhibitor was associated with a 19% risk reduction in cardiovascular events (OR [95%CI]: 0.81 [0.75; 0.86]). Effect sizes were similar for myocardial infarction (0.81 [0.74; 0.89]) and even more pronounced for ischemic stroke (0.77 [0.70; 0.84]). In contrast, all-cause mortality was not improved by the intensified lipid lowering therapy (0.99 [0.93; 1.04]). Stratifying by follow-up duration of < vs. ≥ 3 years, no improvement in all-cause mortality was observed in both groups (<3 years: 1.04 [0.93; 1.17]; ≥3 years: 0.97 (0.88; 1.06).
Analysis revealed significant MIS+EZT-associated with greater percentages in Low Density Lipoprotein (LDL) < 70 (Odds Ratio (OR) 1.76; 95% CI [1.26; 2.45]; p=0.001; I²=73%), LDL reduction (Mean Difference (MD) -5.05 mg/dL; 95% CI [-9.02;-1.07]; p<0.013; I²=56%;); Total Cholesterol reduction (MD -7.91 mg/ dL; 95% CI [-14.90; -0.91]; p<0.027; I²=60%); Triglycerides reduction (MD -8.20 mg/ dL; 95% CI [-13.05; -3.35]; p<0.001; I²=2%;); There was no statistical difference between groups in Drug Adverse reaction (Risk Ratio (RR) 1.19; 95% CI [0.79; 1.78]; p=0.404; I²=0%); and Drug intolerance (RR 0.78 ; 95% CI [0.32; 1.92]; p=0.584; I²=35%).
The upfront lipid-lowering combination therapy of statins and ezetimibe vs statin monotherapy in the reduction of cardiovascular outcomes. A meta-analysis. (US, UK, India, Poland)
Pooled analysis shows that combination LLT significantly reduces the LDL-C level from the baseline (MD, -12.13 mg/dl [0.31 mmol/l] (95%CI: -18.26 to -5.99 mg/dl), p<0.001), all-cause mortality (ACM) (OR, 0.75, 95%CI: 0.62 to 0.92, p=0.01), cardiovascular mortality (CVM) (OR 0.75, 95%CI: 0.66 to 0.84, p<0.001), major adverse cardiovascular events (MACE) (OR, 0.72 95%CI: 0.63 to 0.82, p<0.001), non-significant reduction in the incidence of stroke (OR 0.82, 95%CI: 0.66 to 1.01, p=0.06) when compared with statin monotherapy alone. Similarly, the therapy discontinuation rate was comparable between combination LLT and statin monotherapy groups (OR, 0.87 (95%CI: 0.53 to 1.40), p=0.56). The risk of adverse events related to the gastrointestinal tract (OR, 1.12 (95%CI: 0.93 to 1.36), p=0.23) and musculoskeletal system (OR, 0.88 (95%CI: 0.52 to 1.50), p=0.65) was comparable between both the groups of patients.
Ezetimibe use and mortality after myocardial infarction: a nationwide cohort study (Finland)
Patients with early ezetimibe after MI had lower all-cause mortality during follow-up (33.6% vs. 45.1%; adj. HR 0.77; CI 0.69-0.86; p<0.0001). Early ezetimibe use was associated with lower mortality irrespective of sex, age, atrial fibrillation, diabetes, heart failure, malignancy, revascularization, or statin use. Ongoing ezetimibe therapy during follow-up was associated with lower mortality in time-dependent analysis (adj. HR 0.53; CI 0.48-0.59; p<0.0001).
dual RE (rosuvastatin plus ezetimibe) and triple REB (rosuvastatin plus ezetimibe and bempedoic acid) combination LLT
The percentage reduction in LDL-C level was 44.4%, 55.5%, and 62.2%, respectively (p<0.001). REB enabled 70.8% and 95.2% of patients to achieve the Lipid Association of India, and American College of Cardiology recommended LDL-C targets of <50 mg/dl and <70 mg/dl within 4 weeks. These target levels were achieved in 67.6% and 88.7% of patients on the dual RE therapy and 50% and 81.6% of patients, respectively, on HIS alone.
None of the patients had taken lipid-lowering drugs in the previous 12 months. Patients were randomly assigned to one of two treatment groups: Group 1 - rosuvastatin 40 mg (n= 144) and Group 2 - rosuvastatin 40 mg and ezetimibe 10 mg (n= 120).
As expected, the combination therapy reduced LDL-cholesterol at one month significantly higher compared to high-dose statin monotherapy (-59.65% versus -37.54%; p< 0.0001). After one month of treatment, only 47.92% of patients in Group 1 reached the LDL-cholesterol target (<55 mg/dL) compared to 90.00% of the patients in Group 2 (p<0.0001; R.R.= 0.53).
Compared with a less intensive regimen, HI statin-ezetimibe was associated with reduced risk of all-cause mortality (HR 0.44 [0.21-0.89], P=0.023) and MACE (HR 0.71 [0.52-0.95], P=0.027), with no statistically significant effect on cardiovascular mortality (HR 0.43, P=0.142). Notably, the cardiovascular benefits of HI statin-ezetimibe were more pronounced in patients with elevated Lp(a); a greater reduction in risk of MACE was seen for patients with Lp(a) ≥70 nmol/L (HR 0.51, P=0.007) or Lp(a) ≥100 nmol/L (HR 0.36, P=0.009), and in all-cause mortality risk for those with Lp(a) ≥70 nmol/L (HR 0.24, P=0.025). Although LDL-C reduction >50% was associated with reduced risk of all-cause mortality (p=0.027), this could not fully explain the overall cardiovascular benefit of HI statin-ezetimibe use in patients with or without elevated Lp(a).
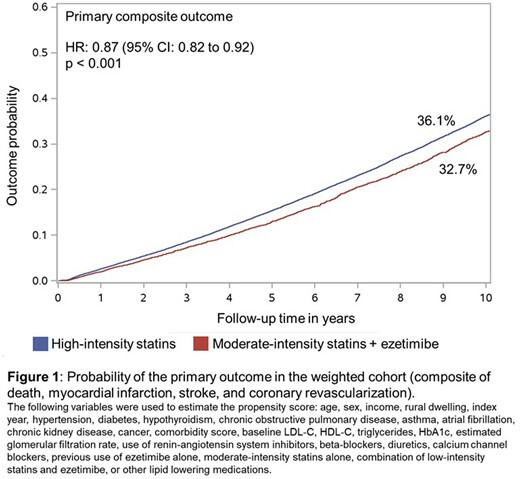
We included all adults aged ≥ 67 years (eligible for drug coverage) with a first prescription of either a combination of moderate-intensity statin with ezetimibe (“combination therapy”) or high-intensity statin alone between January 2010 and December 2022. Patients were excluded if they had not received any prior lipid lowering therapies or had a history of myocardial infarction (MI), stroke, heart failure, peripheral vascular disease or prior coronary revascularisation at any time before or within 3 months of treatment initiation.
The cumulative incidence of the primary outcome at 10 years in the weighted cohort was 32.7% in the combination therapy group and 36.1% in the high-intensity statin group (HR: 0.87; 95% CI: 0.82 to 0.92; p<0.001; absolute risk reduction: 3.5%; 95% CI: 0.8 to 6.1; Figure 1). This result was primarily driven by a lower risk of all-cause death (HR: 0.85; 95% CI: 0.80 to 0.91; p<0.001; Figure 2) and stroke (cause-specific [cs] HR: 0.86; 95% CI 0.74 to 0.99; p=0.04), whereas no differences were observed in the risk of MI (csHR: 0.97; 95% CI: 0.82 to 1.15) or coronary revascularization (csHR: 0.97; 95% CI 0.85 to 1.11).
Moderate-intensity statin combined with ezetimibe versus high-intensity statin monotherapy for secondary cardiovascular risk reduction: a systematic review and meta-analysis (Italy, US, Brazil, Taiwan, India)
Cardiovascular mortality (RR 0.83; CI95% 0.73-0.94; p=0.003), all-cause mortality (RR 0.90; CI95% 0.82-0.98; p=0.02) and non-fatal stroke (RR 0.83; CI95% 0.73-0.93; p=0.002) were significantly lower in patients treated with MIS+EZE compared to those treated with HIS. A significantly higher proportion of patients in the MIS+EZE group reached an LDL-C ≤ 70mg/dL (RR 1.26; CI95% 1.19-1.34; p<0.00001). No statistically significant difference was found for non-fatal myocardial infarction (RR 0.87; CI95% 0.64-1.17; p=0.36), coronary revascularization (RR 1.03; CI95% 0.78-1.35; p=0.83), heart failure (RR 0.95; CI95% 0.86-1.06; p=0.38) and unstable angina (RR 1.52; CI95% 0.62-3.75; p=0.36). A RCT sub-analysis was feasible for cardiovascular mortality and showed no statistically significant difference between the two groups (RR 1.01; CI95% 0.42-2.42; p=0.98).
Regarding safety endpoints, the risk of adverse events (RR 0.84; CI95% 0.74-0.95; p=0.004) and the risk of muscle-related adverse events (RR 0.67; CI95% 0.49-0.92; p=0.01) were significantly lower in MIS+EZE group. The significant reduction in muscle-related adverse events was maintained in the RCT sub-analysis (RR 0.61; CI95% 0.41-0.91; p=0.02). There was no difference between groups in the risk of liver-related adverse events (RR 0.63; CI95% 0.29-1.41; p=0.26) or new-onset malignancy (RR 0.99; CI95% 0.87-1.12; p=0.85).
All the above are from the European Heart Journal, while this one is from a less prestigious journal and research team: Efficacy and safety of double-dose statin monotherapy versus moderate-intensity statin combined with ezetimibe dual therapy in diabetic patients: a systematic review and meta-analysis of randomized controlled trials (India, Pakistan, Bangladesh, Ukraine, US)
Monotherapy showed no significant difference compared with dual therapy for low-density lipoprotein-cholesterol levels [mean difference (MD): −5.03; P = 0.37], high-density lipoprotein-cholesterol levels (MD: 0.01; P = 0.95), total cholesterol (MD: −2.38; P = 0.66), and triglycerides (MD: 5.37; P = 0.67) at follow-up compared to baseline. Monotherapy significantly reduced serious clinical adverse events (risk ratio: 0.21; P = 0.04), with no difference in treatment-related adverse effects, discontinuation due to treatment-related or overall adverse events.
Other similar papers published on this topic this year that reached similar conclusions:
- Cardiovascular Health - #1144 by adssx
- What's the best statin to take? - #469 by adssx
- What's the best statin to take? - #359 by adssx
To me, the topic is now closed, and low-dose statin + ezetimibe seems superior to high-dose statin. Thoughts @CronosTempi @Neo @A_User?