Yes, I appreciate the feedback. With the jardiance and the candesartan, my systolic bp is around 120.
And yes, I weight train 2 days a week and virtual bike race 45min-1 hr 5-6 nights a week.
That’s very interesting about montelukast, I didn’t know that.
@mTORdocTOR @DrM Anti-lymphangiogenic effects of VEGFR-3 pathway inhibition and increased capillary permeability (not gonna talk in depth on basic fluid dynamics between capillary and interstitial space but I’ll leave it here for others) is my current understanding.
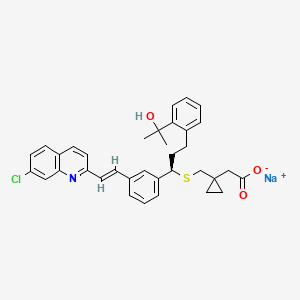
What’s the proposed MOA for montelukast? The molecule looks too big to cross BBB frankly.
That being said, from an initial search, it claims that it might:
“Although montelukast may penetrate the BBB, it is unclear if it enters the brain at concentrations sufficient to have effects in the central nervous system in humans at the doses currently used in asthma treatment. At these concentrations, LTRAs may be acting primarily on the vasculature which may explain the beneficial effects observed in vascular-related cognitive domains such as psychomotor processing speed but not necessarily domains most specific to AD such as memory.”
At that point, perhaps just the hydrophilic statin (assuming early on) or fenofibric acid/fenofibrate (has PPAR alpha functions as well) may be a better gamble if we’re aiming for cerebrovascular, if at least borderline indicated. Haven’t really looked in depth, so would be interested if you had other reasons for it not in that paper.
Not sure if empa has the same effect as cana, if tested in ITP. Empa is a more selective SGLT2i and it seems that cana does have some mild intestinal SGLT1i which might be significant.
If I were taking empa I’d check my CGM/glucose data carefully at the very least to see if at least glucose lowering effect was similar or different than my cana data.
“When compared with canagliflozin, empagliflozin had lower rates of progression of albuminuria, LLA, AKI, and bone fracture; similar rates of HHF, composite renal outcome, and GMI but higher rates of non-fatal MI and non-fatal stroke.”
Not sure if merely elevated creatinine perhaps secondary to multiple factors, such as rapa/ARB associated with "functional renal insufficiency” via inhibiting efferent renal arteriolar vasoconstriction → lowers glomerular filtration pressure → modest reduction in GFR (especially older adults), much higher than average lean mass when age and demographic matched, and ?creatine/high meat intake.
I suspect if we have 100 people with a similar situation, did a 1-month washout, with the newest creatinine and cystatin C algo and urine albumin:creatinine ratio, etc - maybe 5 people might be classified as the earliest stage of CKD and it might not be considered CKD for off-label empa - sounds like a job for nephrologist consult to get down to whether empa is even indicated or not (or inulin “gold standard” if one can find it just to be extra sure), rather than a general PA for that route - just my initial thoughts without enough relevant data or context in front of me, not med advice.
I’m not sure SGLT2i’s would really even do much in HTN without hyperuricemia/Hx of gout (assuming you already have some uricosuric effect from the ARB).
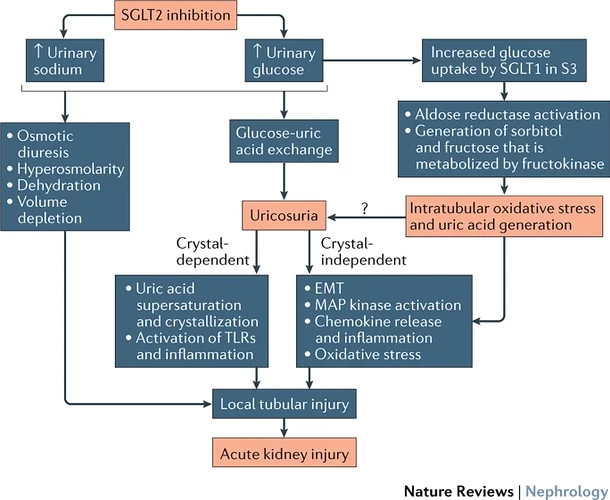
I generally avoid SGLT2i’s with ACEi/ARBs without a good reason due to the possible increased risk of AKI when we add in the hyperosmolarity and volume contraction from the main MOA.
An increase in uric acid excretion via mild to moderate exercise (exercise can induce AKI) and/or low oral intake/heat stroke, on top of 2 agents (ARB + empa) with somewhat uricosuric capabilities could promote a lot of uric acid precipitation in the tubules to cause crystal-dependent and crystal-independent damage - just saying from a risk-averse standpoint. If one does indeed have CKD on top of it (perhaps not likely) - it might predispose one for AKI.
https://www.nature.com/articles/nrneph.2016.159
Frankly, generally speaking, individual-level differences between estimated and measured GFR may be clinically relevant and large enough to impact CKD staging. See the newest data here:
Regarding potential benefit in nondiabetic CHF
“Therefore, the life span benefit of Cana is likely to reflect blunting of peak glucose levels, because similar longevity effects are seen in male mice given acarbose, a diabetes drug that blocks glucose surges through a distinct mechanism, i.e., slowing breakdown of carbohydrate in the intestine. Interventions that control daily peak glucose levels deserve attention as possible preventive medicines to protect from a wide range of late-life neoplastic and degenerative diseases.”
Yes, so I am making an assumption that empaglifozin will have similar benefits as canagliflozin
Try both, one at a time for a few weeks, to see which one is the best for you.
Maybe it is different “body chemistry” but Canagliflozin has been far superior for me.
Neither empagliflozin nor Canagliflozin had any side effects. As often is the case, unfortunately, the one that works better is more expensive. I also like the fact that, unlike Acarbose, I just have to take one tablet in the morning.
Good point to try both!
On what basis do you say Canag is far superior than empag for you?
I test my blood glucose throughout the day, once in the morning before my first meal, then 1 hour after each meal thereafter. Canagliflozin gave me a better fasting glucose level and lower peak glucose after meals. Acarbose is great but you have to take it more often and has unpleasant side effects for me. Empagliflozin was not as effective as Canagliflozin (N=1) in reducing blood glucose spikes after meals. This of course might be a matter of the dosage taken.
I do believe that reducing glucose spikes probably extends lifespan. That is why I believe a possible mechanism for lifespan extension from time-restricted feeding is the reduction of daily glucose spikes and the average amount of glucose in your blood, HbA1c, which of course is an average measurement.
Time-restricted feeding along with your glucose suppressor of choice, metformin, Acarbose, etc., is likely to increase healthspan and/or lifespan.
As we age fasting glucose increases. At 82, my fasting glucose is ~100mg/dL, with empagliflozin the reduction was to ~98mg/dL and with Canagliflozin the reduction was to ~91mg/dL
BTW: My primary physician thinks I am crazy sticking myself several times a day.
Of course, I mainly do it out of curiosity as I am not pre-diabetic.
I believe this theory is panning out as MOA even for us nondiabetics
If I were you I would use a CGM. I find it really informative.
I have been on doxycycline for my acne before rapamycin but rapa makes it much worse. The only antibiotic that works to cure the acne is bactrim. Works every time within a day or 2.
I don’t know if the with food effect with intestinal SGLT1i with cana matters or not since the ITP tested it with all meals yet cana is generally used at the start of the day. I believe some other chap mentioned it here already. Empa is much more selective SGLT2i so it may not have the same effect as cana. Both have potential for side effects in the long run that are not necessarily noticeable right away. Especially older adults in general.
There is no long-term safety data on the effects of chronic glucosuria on the urinary tract, but the FDA has initated postmarketing studies due to these risks from immune dysfunction to bladder cancer from a somewhat significant number of case reports. Hence, I personally only do intermittent cana (I’m trying to keep uric acid down to right under 5.8 while keeping well hydrated among other reasons).
If the core hypothesis is true on hyperglycemic environments - significant amounts of SGLT2i induced glycosuria seems to be potentially particularly problematic especially when we jump into urogenital infections that may accelerate aging phenotype even with the assumption of no urosepsis (or rare Fournier’s gangrene).
We already know that glycosylation of uroplakins (presumably from glycosuria) can be a potential part of immune dysfunction as it’s the main “barrier” for the bladder. There is a bladder-associated microbiome and perhaps the possibility of some rough threshold exists or some preexisting precancer lesions seems plausible in animal studies - particularly with empa over cana. On the other hand, the most common infectious agents - gram-negative bacteria ie E coli and P mirabilis produce nitrosamines where metabolites are known carcinogens. Chronic UTIs can be asymptomatic - with the molecular inflammatory subtype tending towards the more aggressive deadly form of bladder cancer.
There is more than enough evidence for a bidirectional relationship between UTI and new onset dementia.
Not worth doing the full deal for me or empa entirely for me until there is more data for certainty on some threshold, even if it potentially results in no life extension effect (which is not yet really evidenced much in the first place for healthy) for now. Trying to balance cardiorenal, immune, and pancreas/metabolic systems and those tend to age faster first with very high impact on mortality.
Presumably the montelukast is functioning to block leukotriene receptors on microglia, which are basically brain-resident macrophages. As with other macrophages, this presumably helps to prevent/limit M1 polarization of the neuroglia, which in turn would help to calm down an inflammatory situation.[Edit: Also, my understanding is that when there’s significant inflammation going on, the BBB may be substantially more permeable to many drugs than it normally would be.]
Canaglilozin looks good to me.
Mabe Canaflizon is a better choice for smokers and the elderly?
Possible increase in bladder infections, but no increase in cancer for Canaglifozin.
In fact, it might prevent or fight cancer.
“These data indicate that like the biguanide metformin, Canagliflozin not only lowers blood glucose but also inhibits complex-I supported respiration and cellular proliferation in prostate and lung cancer cells.”
"The current findings provide novel evidence and demonstrate that CANA effectively inhibits the growth of pancreatic cancer in addition to its anti-diabetic role. CANA is capable of suppressing pancreatic cancer growth by inhibiting glycolysis.
“A Review on the Relationship between SGLT2 Inhibitors and Cancer”
“No increased risk of overall bladder or breast cancer was noted for canagliflozin”
Yes, I’m aware of the “no increased risk” studies but keep in mind they are in the short term.
I’m talking about long-term exposures where animal studies still support the possibility as well as several plausible mechanisms of known shorter-term effects of SGLT2i from human studies on common infectious agents that are known to produce carcinogens or increase risk for bladder cancer.
Your same study also says “Relationship between SGLT2 inhibition and cancer formation is still inconclusive and studies with larger sample size, longer exposure duration, and different ethnicities are warranted” - we don’t know if canaglifozin over long-term studies may show some effect.
That’s why I said “There is no long-term safety data on the effects of chronic glucosuria on the urinary tract” and even the FDA is interested in postmarketing survelliance
“There is no long-term safety data”
That is true of many of the supplements we take.
In many of the studies, I have looked at, it seems dapagliflozin, not canagliflozin is the risk factor. There seems to be some other factor than just SGLT2 inhibition.
That’s partly why the supplements I take are generally well within the upper limit of what a diet in a studied subpopulation takes - i.e. creatine monohydrate (specifically Creapure), preferably in how it is typically absorbed as a very general heuristic. Most people are in fact taking things that do not have long-term safety data and have a real very likely potential for harm i.e. lead or other heavy metals that exceeds the limits by many times. One might not notice it in the short-term but there is strong potential for real likely long-term harm in excessive lead amounts, as an example.
I very sparingly make exceptions if there is a very compelling case, even then I’d carefully consider any individual factors or situations, the entire manufacturing process and quality control process, and what I’d like to test for or monitor. This might be surprising to some, but plenty of “third party” test results are bogus (supplement companies generally go extra cheap-o and/or false and misleading on testing regardless of one’s brand perception) and one can only easily figure it out by reading the fine print and whether it makes sense given enough context.
A lot of people like to go the “kitchen sink” route and don’t think about evaluating patient safety in depth on a case by case basis, mechanistic basis for these compounds, drug interactions, how it may affect pathophysiology, or all the possible interactions and such. There may not be apparent harm in the short-term - but the multivitamin and antioxidant studies showing increased mortality over the long run in “gold standard” Cochrane reviews give us more than enough pause for what was previously widely considered “safe”.
Now one can have very high risk tolerance and very high levels of optimism on an individual level - not necessarily anything inherently wrong with that assuming one is well informed of the risks.
Personally, I have a low risk tolerance that is only relatively overcome to some extent by the risk of doing nothing, while balancing the risks of over-interventionalism with cautious levels of optimism.
Would you please share which supplements you do take?
See @tongMD supplement stack here: Can you share your Longevity / HealthSpan Regime? - #68 by tongMD
I’ve changed exactly what I’m taking somewhat and currently not taking rapamycin as I’ve developed symptoms that may be related with 6 mg/week - mild polyarthalgias (intermittent, 1-2/10, symmetric in the extremities) and positive serology that may or may not be a false positive. Normal hs-CRP/ESR. (Stopped in a few days right after it was clear not an one-off mild polyarthralgia)
If it is induced by rapamycin, it may take months to recover from what is possibly reversible drug-induced arthralgias, and we shall see. It seems to be related to rapa and is a common symptom in transplant patients. Or it could be “pre-RA”/“pre-lupus” unrelated to or indirectly associated with rapa, but my rheumatologist thinks either is possible and we came to believe that an infectious agent (ie rare but possible unconfirmed parvo B19 chronic arthalgia) causing false positive is also plausible, but not an easy way to distinguish when false positives are possible with none of the high specificity tests turning positive. These are very mild symptoms that don’t affect my daily life, but if it is indeed a rheumatoid disease - prognosis probably isn’t particularly horrible either when early DMARDs are started. Just better to get the right diagnosis first before revisiting whether to continue perhaps very low dose rapa.
I’ll eventually detail in a separate blog, along with my clinical reasoning involved for each selection in detail