I would consider it but being somewhat conservative, I prefer to use Pfizer’s rapamycin due to its well studied pharmacokinetics. It’s only available in 1 mg doses from my supplier. I just saw they do make a 0.5 mg dose as well as an oral solution. The oral solution would work.
Pfizer produced 0.5 Rapamune pills (as well as 1 mg and 2 mg), however it discontinued production and sale in the U.S. on Dec 31, 2024 (patent expires and generic sirolimus is available). Are you sure you receive brand- name Rapamune by Pfizer from your supplier?
Yes, it is sourced from Pfizer / Turkey. Thanks for your concern as there is a lot of contraband out there!
Below is a link to the LAM foundation letter regarding discontinued Rapamune in the U.S.
Just an observation that may not be of any importance. Since revising my rapamycin schedule from 4 to 5 mg every two weeks taken with grapefruit juice to 6 mg once weekly without grapefruit, I’ve noticed a definite rise in side effects:
- Post-dose fatigue: marked grogginess and a flare-up of my baseline chronic pain the day after dosing.
- Oral ulcers: previously rare, now frequent (sometimes two at once). A stubborn sore beneath my tongue is currently making eating difficult.
Because this change reduced my expected systemic exposure, I hadn’t anticipated new or worsening symptoms. Any thoughts or experiences?
I was getting rapamune from Greenstone pharmacy when I started rapamycin in 2020. Then got switched to zydus.
I liked rapamune best!
I’m not sure why we get mouth ulcers. Usually only inflammation cause that.
The higher the dose the more side effects. I can tell the difference between the doses. When my dose goes too high, I get hives. The more I take, the more hives I get.
AIUI the ulcers arise from a reduction in WBC.
I thought I would ask chatGPT and I copy the answer below. However, I know from my personal experimentation that the Neutrophil count drops really rapidly as a result of mTOR inhibition because they have a short half life. So that part of chatGPT that says WBC goes down slowly is not accurate.
Short answer
There is little direct evidence that rapamycin-associated mouth ulcers (mTOR-inhibitor–associated stomatitis, mIAS) are caused by the fall in white-blood-cell (WBC) count. Both events can appear in the same patient, but the bulk of clinical, pharmacokinetic and laboratory work points to a local, cytokine-driven epithelial toxicity that is largely independent of systemic myelosuppression.
What the data actually show
| Evidence stream | Key findings | What it says about WBC ↓ as cause of ulcers |
|---|---|---|
| Large oncology trials (e.g. BOLERO-2, solid-tumour meta-analysis) | Stomatitis in 59-70 % of everolimus-treated patients; 80 % of first episodes occur within 8 weeks, often before any grade ≥ 2 cytopenia appears. allianceforclinicaltrialsinoncology.orgAnnals of Oncology | Timing argues against leukopenia as trigger. |
| Population PK study (n = 67 cancer pts) | Severity of stomatitis tracks drug exposure (AUC, Ctrough); haematologic values not predictive. PubMed | Exposure–response, not WBC–response. |
| Prospective LAM cohort on sirolimus (n = 50) | 89 % developed stomatitis. Low baseline haemoglobin and evolving micro-cytosis predicted ulcers; WBC counts had no association. PubMed | Again, no link. |
| Regulatory safety datasets & expanded-access programmes | Stomatitis and leukopenia listed as separate adverse events; they often co-occur but are not graded together. FDA Access DataPMC | Co-incidence ≠ causation. |
| Mechanistic/ in-vitro work | Organotypic oral-mucosa models and biopsy studies show mTOR inhibition → keratinocyte cell-cycle arrest, ↑TNF-α / IL-2, and aphthous-like ulceration; no role for neutrophil depletion. JAMA NetworkJomos |
How to read these findings
-
Temporal dissociation
2.Ulcers usually appear in the first 1–3 weeks*, long before significant leukopenia is measurable. -
Dose- or exposure-response, not cell-count-response
The best-demonstrated predictor of ulcers is higher rapamycin (or everolimus/sirolimus) exposure; adjusting the dose or using mouth-rinse prophylaxis lowers ulcer rates even though blood counts are unchanged. - Pathobiology is local and inflammatory
- mIAS lesions are small, shallow, and histologically resemble recurrent aphthous ulcers rather than classic mucositis.
- mTOR blockade slows keratinocyte turnover; local trauma + increased TNF-α & IL-2 create an exaggerated aphthoid response.
- Corticosteroid or dexamethasone mouthwashes prevent/short-circuit the lesions without affecting systemic immunity.
-
Leukopenia still matters—but mostly for healing & infection
Severe neutropenia can prolong ulcer healing or allow secondary infection, so monitoring counts is still prudent; it’s just not the initiating event.
Bottom line for clinicians & patients
- Expect ulcers even when the CBC is normal.
- Manage exposure (lower peak/trough rapamycin levels if ulcers are dose-limiting).
- Start prophylactic topical steroids in high-risk settings (strong evidence in SWISH and other trials).
- Reserve WBC support (e.g., G-CSF) for true cytopenia; it will not, by itself, stop the ulcers.
In sum, current research does not support a causal WBC-driven mechanism; mouth ulcers arise from direct mucosal effects of mTOR inhibition and local inflammatory mediators, with leukopenia playing at most a secondary, complicating role.
I’ve never experienced hives, at least as far as I’m aware, sounds nasty! This painful mouth ulcer under my tongue just won’t go away. Normally, when I get ulcers, they’re not painful, but this one has been quite difficult, possibly because it’s in an aggravating location. I’ve started rinsing with salt water and I’m using a lidocaine gel sparingly to manage. Hopefully it heals soon.
I’ve noticed an increase in mouth ulcers since switching to a weekly dose regimen. For me, it might be more about the frequency. I’m planning to try three weeks of 1mg per day next to see how that affects things. Will report back.
What can we do to mitigate it?
I don’t think you can mitigate the reduction in WBC. That is part of inhibiting mTOR. I think the reason I don’t get those side effects although I take higher doses (intermittently) is primarily other things I am doing to strengthen my immune system and secondarily that I drop my rapamycin levels really low before the next dose not just for a day, but for some weeks (at the moment).
Aphthous ulcers are a likely a sign of immune dysregulation, according to the literature on the subject, which is why I titrated my rapa dose to a level where they do not manifest.
It doesn’t happen to me all the time but at times it is annoying. My only remedy is to use mouth wash during those time. But then again I don’t like using Listerine too often. Because we have different beneficial bacteria in the mouth too.
It seems there are many potential contributing factors when it comes to apthous ulcers…
From chatgpt
Aphthous ulcers (also called canker sores) are small, painful lesions that occur inside the mouth. Their exact cause is not fully understood, but several causal and contributing factors have been identified:
1. Local Trauma
- Biting the inside of the cheek or lip
- Brushing too hard
- Dental work or ill-fitting dentures
- Sharp or broken teeth
2. Nutritional Deficiencies
- Iron
- Vitamin B12
- Folic acid
- Zinc
3. Stress and Hormonal Changes
- Emotional stress or anxiety
- Hormonal fluctuations (e.g., during menstruation)
4. Immune System Factors
- Dysfunctional immune response (hypersensitivity reaction)
- Autoimmune conditions (e.g., Behçet’s disease)
5. Food Sensitivities
- Spicy, acidic, or salty foods
- Certain food additives (e.g., sodium lauryl sulfate in toothpaste)
- Allergens like chocolate, coffee, nuts, strawberries, or gluten
6. Infections
- Viral infections (though aphthous ulcers are not caused by herpes)
- Secondary bacterial infection may worsen the lesion
7. Genetic Predisposition
- Family history increases risk
8. Systemic Diseases
- Celiac disease
- Crohn’s disease
- Ulcerative colitis
- HIV/AIDS
9. Medications
- NSAIDs
- Beta-blockers
- Chemotherapy drugs
If aphthous ulcers are frequent, persistent, or unusually severe, it may indicate an underlying systemic issue that should be evaluated by a healthcare provider.
[Immune dysregulation linked to several triggers may facilitate the development of RAS. The roles of the immune system and inflammatory processes have been confirmed in recent large-scale bioinformatics analyses (14,15). It is known that a Th1-type hyperimmune response favors the appearance of inflammatory reactions that precede ulcerations (Fig. 1) (16,17). In addition, genetic risk factors can determine individual susceptibility to RAS; in particular, several DNA polymorphisms of the NOD-like receptor 3(18), toll-like receptor 4(19), interleukin (IL)-6(20), E-selectin (21), IL-1β and TNF-α genes (22). However, despite the large number of factors examined, the underlying cause triggering the episodes of ulcers remains to be elucidated. Therefore, clinically, the emergence of new lesions cannot be avoided at present.](Essentials of recurrent aphthous stomatitis - PMC)
For treatment, while quite messy and somewhat distasteful but not too unbearable, I applied a topical steroid clobetasol propionate 0.05%, and after an hour or so, some good old clove oil which stings at first but last a few hours.
It may be that rapa at particular doses in particularly sensitive individuals (raising hand) may induce a hyperimmune response, much as seen in older folks having better responses to flu vaccination post rapa dosing. I reckon I’m conservative and don’t really want a hyperimmune response (if that is what causes the ulcers) if I don’t need it, plus it hurts, a lot!
I forgot to add that I also avoid toothpastes that contain sodium lauryl sulfate, which is also used to solubilize cells and “straighten out proteins for electrophoresis” i.e. disrupt secondary protein structure, and is known to be a risk factor for development of aphthous ulcers in some people.
Absolutely that seems likely for some people. I’ve only had one in the past 5 years, and at one of the lower doses that I’ve taken during that period, so I really can’t say I understand it. Others, like Peter Attia, have commented that if his young son head-butted him accidentally, the stress might cause Peter to get an apthous ulcer.
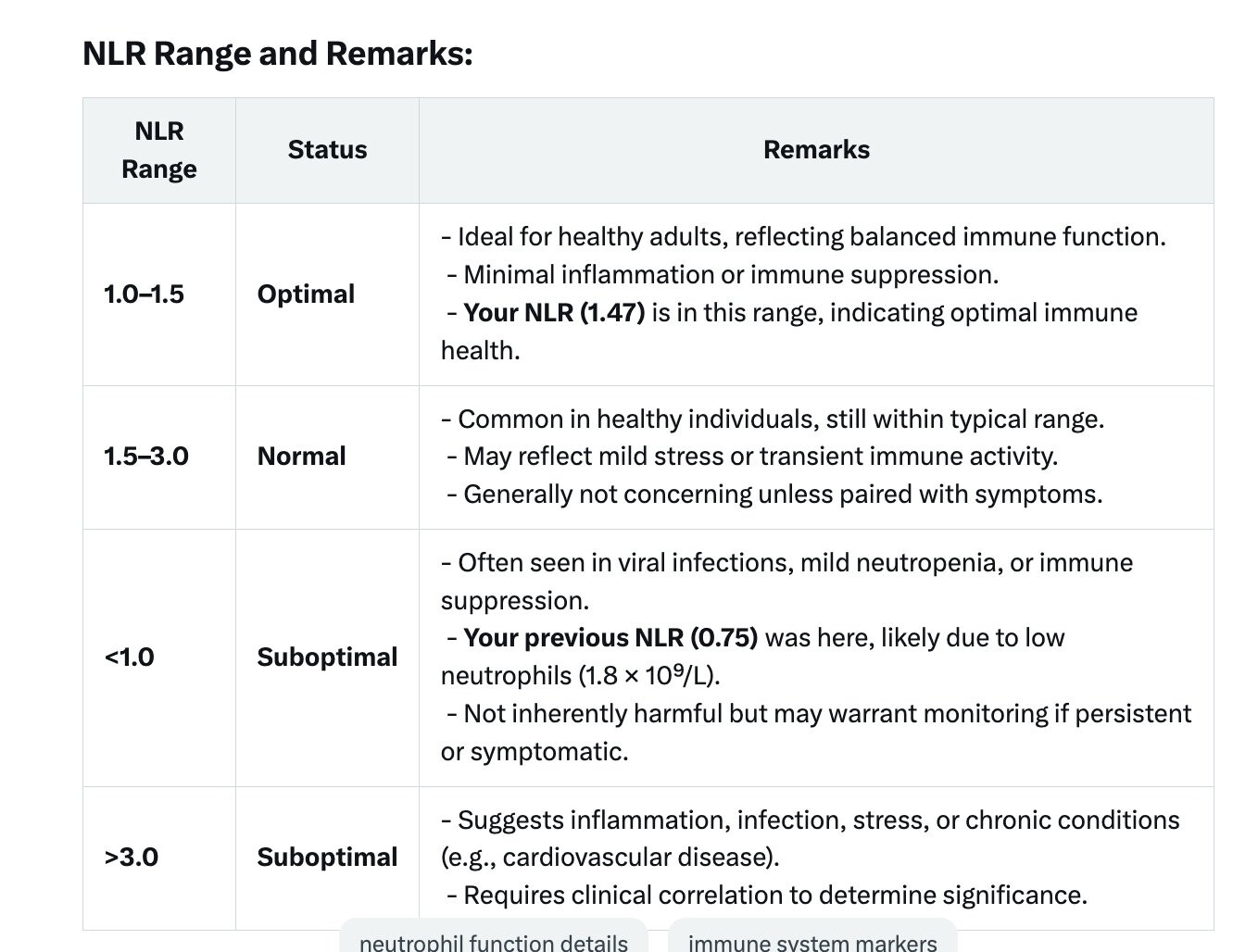
For practical purposes, I have decided to follow my NLR as a dosing guide, all things being equal. NLR can easily be calculated from a simple Hematology panel.
-
Neutrophils: White blood cells that fight infection and are elevated in acute inflammation or stress.
-
Lymphocytes: Immune cells involved in adaptive immunity, often decreased in chronic stress or inflammation.
NLR is a marker of systemic inflammation, stress, and immune balance, used in contexts like cardiovascular disease, cancer prognosis, and autoimmune disorders.
-
Target: An NLR of 1–2 is optimal, indicating minimal inflammation and good immune balance.
-
Actionable Thresholds:
-
If your NLR is >3, it might suggest underlying inflammation and pathology.
-
If your NLR is <1, it’s less likely but could indicate immunosuppression, which might be relevant if you have other signs (e.g., frequent infections).
-
Some real data tracking: