I have just posted this:
People who study NCD (Non Communicable Diseases) and particularly those that focus on the diseases of aging (which I think include many of the NCDs, but not all of them) have a concept of someone having a biological age as well as a chronological age. This guides things like how frail someone is, how well their cognition works, whether they are at the risk of cancer or diabetes or indeed how they look.
Human beings are quite good at judging each other’s general health by appearance. That is because the various NCDs tend to correlate with how well the body maintains the skin and when someone is frail it is quite easy to see this by how they move around.
Regular readers of my blog will know that I think this is because the genome stops functioning properly as people get older. In essence cells stop producing the right proteins. I provide full details of this hypothesis on this web page Further thoughts from the world of independent researchers.
Various approaches have been used to calculate a biological age. Some look at methylation marks on DNA. Others take various biomarkers and try to calculate an age from those. These are always done in years (or months).
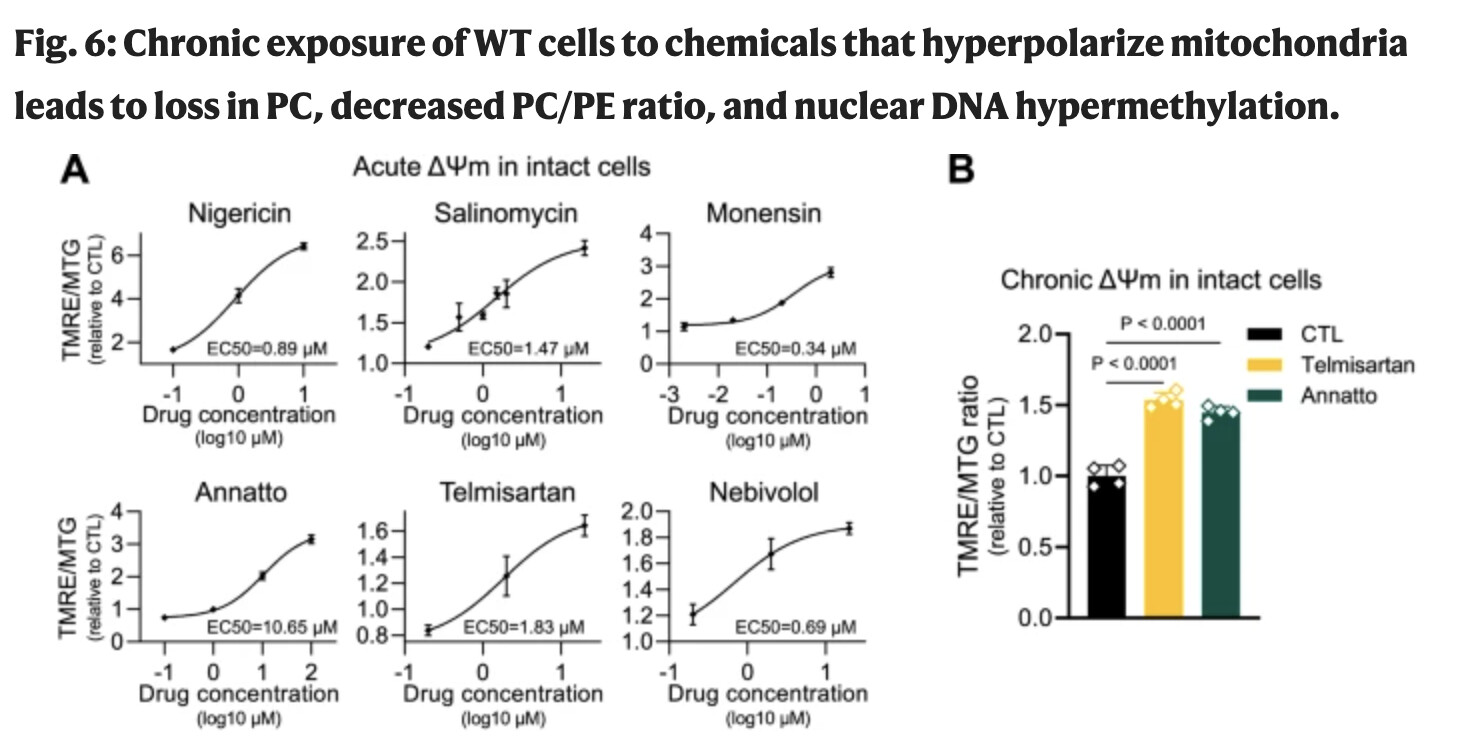
However, if the biological age actually primarily depends upon the efficiency of the mitochondria and the membrane potential of mitochondria then perhaps the biological age should reflect that. The membrane potential of mitochondria is measured in millivolts. (normally in the low 100s) Although practically measuring the combination of the membrane potentials of all of the mitochondria in all of the cells is not practical the question is still raised as to whether there is a reason for looking at things this way. I think there is.
What is obviously the case although not necessarily thought about that much is that the average membrane potential of a human egg mitochondria when fertilised is not constant. It is this, however, that drives where development goes both as the egg becomes an embryo and then gets born as a baby. Also when the baby grows up. There is solid scientific research that demonstrates that this starting position is a key foundation as to how good someone’s health will be. Also it would sound a bit odd that a baby would be born at a varying biological age.
There are good reasons why it is worth people knowing the state of their mitochondria. There is plenty of evidence that the state of the mitochondria can be improved (and also made worse). Therefore for people who start out with a lower membrane potential it is more important to them to look for interventions that will help prevent cancer or diabetes in later years. In a sense this moves away from the concept of biological age as “age”, but more towards it being a health and development status.
At the same time the fact that people start out with different membrane potential averages shows that the links between membrane potential and development are not just linked to an absolute value. The variation in membrane potential links to hormones and the variation in hormones drives development. Hence although for example a lower membrane potential will tend to speed up development such that puberty happens earlier, it probably won’t link directly to a multiple of the membrane potential.
People will still want to work out where they are compared to the average and there will be a mechanism to associate an average membrane potential to an age. However, understanding what is happening with the biology is perhaps more useful to people who want to improve their health.