In reading tge above linked study its hard to understand their conclusionnwhen the author clearly makes this statement of findings from the largest collection of subjects and clinical trials
“the largest publicly available detailed data comes from the ARB Trialists Collaboration, which was a project dedicated to examine the risk of new cancers with ARBs. The sponsors of the randomized trials performed with these drugs provided the data to the ARB Trialists Collaboration [25]. This collaboration ultimately used comprehensive patient-level data, including a total of 138,769 patients from 15 randomized controlled trials [27–41] and concluded that there is no excess risk of new cancers with ARBs.”
The point was made to exclude those with already preexisiting cancers. Seems like a given assumltion but I guess past ones did not that showed increased risk?
Thanks, I’ll have a look!
For whatever reason, this low-quality paper is often posted on this forum. See:
Whether it’s a good or bad study I don’t know, but it’s getting traction as physicians decrease use or ARB’s.
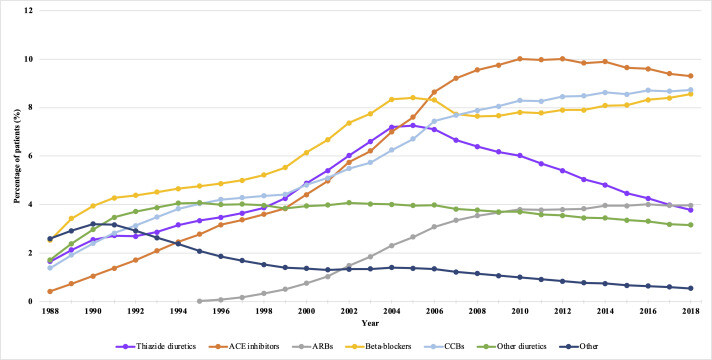
It’s the opposite, as all data and papers point to ARBs being superior to other antihypertensive drugs, they’re increasingly used:
- In the US: The Top 300 of 2021 (lisinopril constant vs losartan +1, benazepril -6 vs valsartan +3, etc.)
- In the UK: Treatment and prescribing trends of antihypertensive drugs in 2.7 million UK primary care patients over 31 years: a population-based cohort study 2022
I’ve just checked nebivolol briefly. It’s interesting as it might have fewer side effects than other beta-blockers, but I don’t think it’s good enough to replace other antihypertensive drugs.
Apparently (Wikipedia, I didn’t double-check the sources), it is only highly cardioselective for β1 at low doses (5 mg), then loses its cardioselectivity and “nebivolol is also not cardioselective when taken by patients with a genetic makeup that makes them “poor metabolizers” of nebivolol (and other drugs) or with CYP2D6 inhibitors” (how can we check that?)
According to the 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: “However, there are no outcome trials with vasodilating BBs in hypertensive patients, and the same applies to bisoprolol. There are also some recent large real-world studies with vasodilator BBs conducted in the USA, with inconsistent results. In one study, there was no statistically significant difference in CV outcomes between 118 133 patients receiving either nebivolol or carvedilol and 267 891 patients receiving atenolol [588]. In other studies, use of nebivolol led to greater CV protection compared with use of atenolol or metoprolol [589,590].”
Also, in the recent EPITERNA paper, nebivolol was not associated with life extension, although not statistically significant, it was more on the side of “lifespan reduction”. In “Association of cardiovascular disease management drugs with Lewy body dementia: a case–control study”, nebivolol didn’t perform better than other antihypertensive (and especially not better than the best in class like sartans and their combinations with CCBs or thiazide).
There’s one ongoing trial comparing nebivolol to telmisartan, with results expected in 2026. Other than that, I couldn’t find interesting trials of nebivolol so I assume that it doesn’t interest researchers that much.
Nebivolol might be interesting in quadruple low‐dose treatment. For instance, the QUARTET USA trial tried candesartan, 2 mg, amlodipine, 1.25 mg, indapamide, 0.625 mg, and bisoprolol, 2.5 mg, once daily. While QUARTET Australia tested irbesartan at 37.5 mg, amlodipine at 1.25 mg, indapamide at 0.625 mg, and bisoprolol at 2.5 mg.
We’ll get the ITP results for nebivolol next year. I understand that when a compound works, the ITP team notices it early on and mentions it informally (on social networks or in podcasts) and/or starts scheduling a second round trial. For instance, Sodium Thiosulfate (STS) is part of the same batch as nebivolol, and as it seems promising, it was selected again last year to be re-tested at a different dose and confirms the findings. Does it mean nebivolol failed?
Beta-blockers are also associated with increased risk of Parkinson’s disease. (see “Our comprehensive study indicated that regular NBB use is associated with an increased risk of PD. In light of the detrimental effects of NBBs on PD, some people should choose alternative antihypertensive treatments.” in Nonselective beta-adrenoceptor blocker use and risk of Parkinson’s disease: from multiple real-world evidence 2023). There might be reverse causation as propranolol is used for mild essential tremors that can be early Parkinson’s symptoms. Still, unless I can find evidence that nebivolol is associated with a significantly lower risk of Parkinson’s and Alzheimer’s and other dementia and NDDs vs telmisartan, amlodipine and indapamide, I see no reason to use it.
Fair enough, thanks for the review! For now, perhaps it’s safe to say IF a person needs/wants a BB, nebivolol is the one to choose due to less side effects (lipids, sexual dysfunction, etc) and greater tolerability, but it doesn’t seem to necessarily have any better outcomes than other BBs.
I’ll probably try transitioning to telmisartan again. Last time it made me drowsy and “brain foggy”, but maybe I just need to take it slower and give myself longer to adjust.
That’s also what I initially thought but for instance nebivolol doesn’t seem to be used for arrhythmias contrary to atenolol, bisoprolol and metoprolol. According to this 2022 paper: “Little evidence exists regarding the role of nebivolol in the treatment of both supraventricular and ventricular arrhythmias. Until further evidence accumulates, nebivolol should not be the first beta blocker chosen when treating arrhythmias.” (Nebivolol for the Treatment of Arrhythmias: a Narrative Review)
So I’m not even sure you can use switch BBs like that.
Interesting! Maybe that’s why my nebivolol seemingly had no effect in protecting against the two episodes of afib I’ve had over the last several years (both happened after chugging a cold fruit smoothie).
Have you come across the topic of psychological stress-induced myocardial ischemia in your hypertension readings? It always seemed like a beta blocker would be most protective against this “fight or flight” response from a stressful event that can trigger a MI, but when last I checked (several years ago), I couldn’t find much data and what I did find never seemed to mention beta blockers.
I’ve never checked this. I assume it’s hard to measure. In clinical trials and medical records, can we distinguish stress-induced MI from other myocardial ischemia? If not: we cannot know which drug works best for this.
Oh it’s definitely a thing and is measurable, and puts people prone to this at much higher risk of cardiac events. I’ll look into the literature later today to see what I can dig up.
Of course, stress-induced MI is real. But can you distinguish on a dead body whether the person died of stress-induced MI or non-stress-induced MI?
A positive for telmisartan seems also to be weight/fat loss. I’m experiencing that with my regimen and think my high dose of telmisartan is helping (though I’m also taking other things like rapa and jardiance that many feel help in the weight/fat as well)
Do other bp medicines have this effect?
I didn’t believe it but a quick research confirms that telmisartan slightly decreases body weight:
- Effects of telmisartan on adiponectin levels and body weight in hypertensive patients with glucose intolerance 2008: “Candesartan did not achieve similar improvements in these patients. Among ARBs, telmisartan may have a larger impact on obesity-related diseases that can lead to cardiovascular disorders.”
- Telmisartan Prevents Weight Gain and Obesity Through Activation of Peroxisome Proliferator-Activated Receptor-δ–Dependent Pathways 2010
- Telmisartan reduced abdominal circumference and body weight with decreasing triglyceride level in patients with type 2 diabetes and metabolic syndrome 2010
It also affects fat distribution: Effects of telmisartan on fat distribution: a meta-analysis of randomized controlled trials 2015
See also: Effects of telmisartan on metabolic syndrome components: a comprehensive review 2024 (![]() Iranian paper
Iranian paper ![]() )
)
I wonder if its affects on body weight/fat are in a dose dependent manner? I’m taking the 80 mg. Will be interesting to observe my body after a few months more on it as ive really just started it recently. (though I’m also taking other substances that could be decreasing the body weight/fat)
I think the idea behind PSIMI is to subject patients to a psychologically stressful stimulus and assess for signs of mild cardiac ischemia. Those who show signs of ischemia from psychological stress (vs those who don’t, while carefully controlling for other risk factors) have a much higher risk of future cardiovascular events. Thus, meds which block this effect should significantly reduce future risk in those who experience PSIMI. I’m curious if they’ve yet done studies with different classes of BP meds to assess which may be best for this use.
Edit: it’s referred to as “Mental Stress Induced Myocardial Ischemia” aka MSIMI. Here’s a recent review, but not a lot of answers yet.
What is written in guidelines whether to start use of anti-coagulants in your case for stroke prevention because of afib?
It’s a tough call. I’ve never had episodes of afib other than those two times after chugging cold smoothies (and I know immediately when I’m in afib, unlike some who can’t tell), so is it worth being on an anticoagulent med for the rest of my life, which also carries its own risks? There aren’t any anticoag outcome studies in the subgroup of patients who only get afib from drinking cold drinks too fast. I do plan to ask my cardiologist next time I see him if it’s worth wearing a portable cardiac monitor for a month to see if I ever have any brief episodes of afib during sleep, for instance. I wore a FitBit for several months with afib detection and never got any notifications.
I don’t know anything about this but you never know whether what the cardiologists etc are saying is medicine 2.0 or 3.0. If it’s the same case as for statins or similar drugs, that is.
If I search for studies on apixaban I found this:
Apixaban for Stroke Prevention in Subclinical Atrial Fibrillation
We included 4012 patients with a mean (±SD) age of 76.8±7.6 years and a mean CHA2DS2-VASc score of 3.9±1.1 (scores range from 0 to 9, with higher scores indicating a higher risk of stroke); 36.1% of the patients were women. After a mean follow-up of 3.5±1.8 years, stroke or systemic embolism occurred in 55 patients in the apixaban group (0.78% per patient-year) and in 86 patients in the aspirin group (1.24% per patient-year) (hazard ratio, 0.63; 95% confidence interval [CI], 0.45 to 0.88; P=0.007). In the on-treatment population, the rate of major bleeding was 1.71% per patient-year in the apixaban group and 0.94% per patient-year in the aspirin group (hazard ratio, 1.80; 95% CI, 1.26 to 2.57; P=0.001). Fatal bleeding occurred in 5 patients in the apixaban group and 8 patients in the aspirin group.
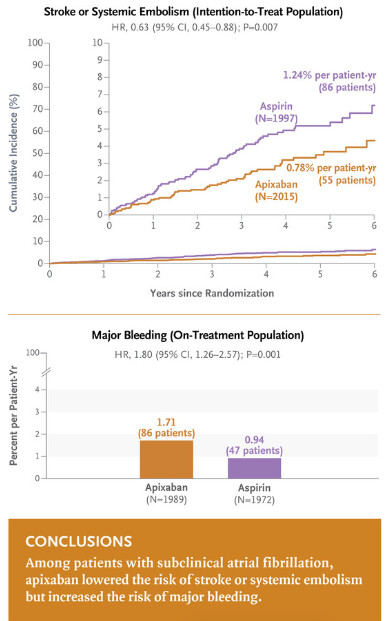
https://www.nejm.org/doi/full/10.1056/NEJMoa2310234
I know almost nothing about this or afib.
Very interesting! That’s a newer paper I hadn’t seen and wasn’t out when last I discussed this with my cardiologist. I’ll make sure to bring it up and revisit it, thanks. I already take clopidogrel (Plavix) for CVD risk reduction (since I can’t tolerate even low dose aspirin), so adding an anticoagulent to Plavix would REALLY heighten bleeding risk, and I doubt swapping the Plavix for Eliquis would be a good idea because then I wouldn’t have the antiplatelet effect for heart attack prevention.