A new paper:
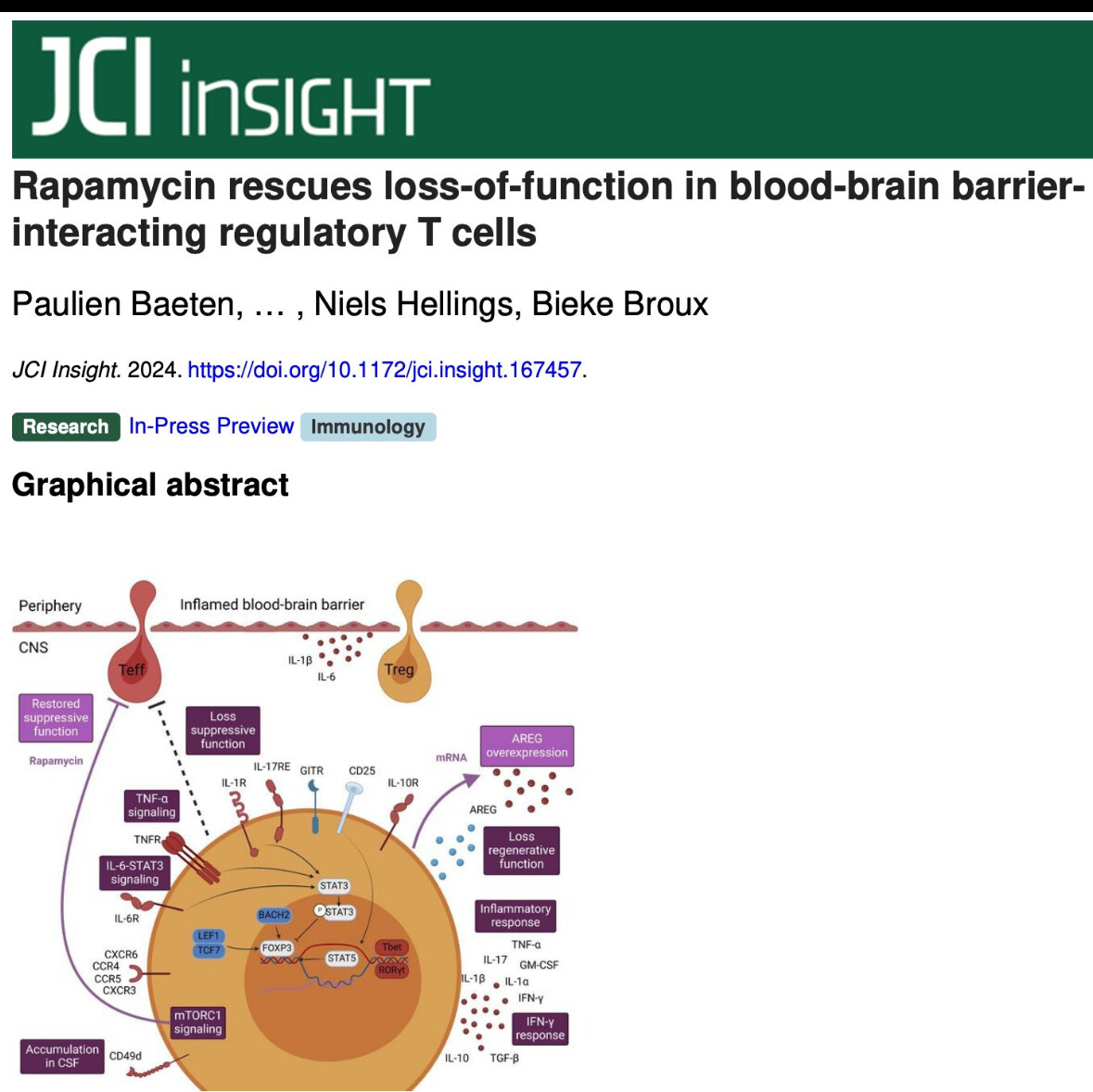
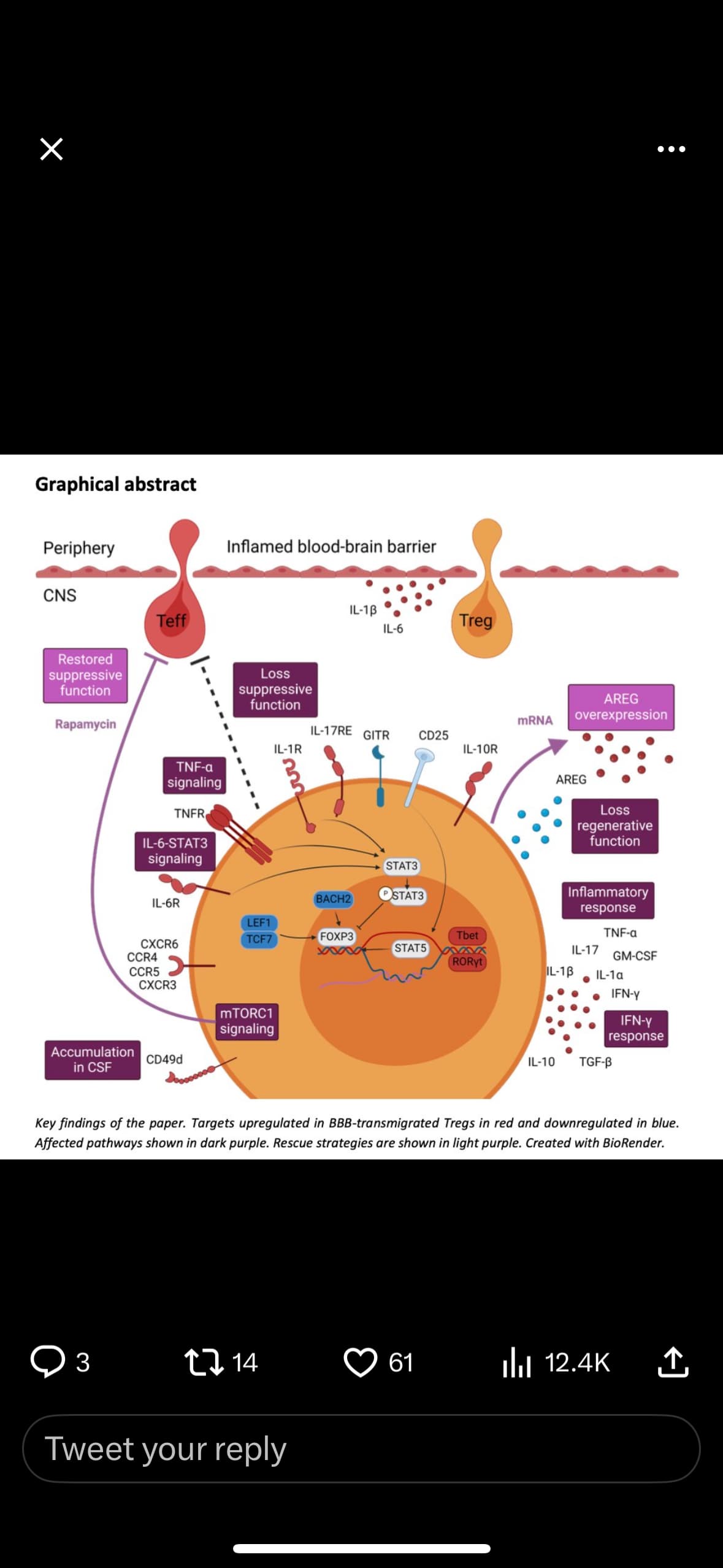
In autoimmunity, FOXP3+ regulatory T cells (Tregs) skew towards a pro-inflammatory, non-suppressive phenotype and are therefore unable to control the exaggerated autoimmune response. This largely impacts the success of autologous Treg therapy which is currently under investigation for autoimmune diseases, including multiple sclerosis (MS). There is a need to ensure in vivo Treg stability before successful application of Treg therapy. Using genetic fate-mapping mice, we demonstrate that inflammatory, cytokine-expressing exFOXP3 T cells accumulate in the central nervous system during experimental autoimmune encephalomyelitis. In a human in vitro model, we discovered that interaction with inflamed blood-brain barrier endothelial cells (BBB-ECs) induces loss-of-function by Tregs. Transcriptome and cytokine analysis revealed that in vitro migrated Tregs have disrupted regenerative potential, a pro-inflammatory Th1/17 signature and upregulate the mTORC1 signaling pathway. In vitro treatment of migrated human Tregs with the clinically-approved mTORC1 inhibitor rapamycin restored suppression. Finally, flow cytometric analysis indicated an enrichment of inflammatory, less suppressive CD49d+ Tregs in the cerebrospinal fluid of people with MS. In sum, interaction with BBB-ECs is sufficient to affect Treg function, and transmigration triggers an additive pro-inflammatory phenotype switch. These insights help improve the efficacy of autologous Treg therapy of MS.
Open Access Paper: