ChatGPT 5.1 Summary
Here is my structured summary, novelty-identification and critique of the paper Preservation of Autophagy May Be a Mechanism Behind Healthy Aging (Bektas et al., Aging Cell, 2025). I will follow your preferred format: executive summary, bullet summary, claims/evidence table, actionable insights, and technical deep dive + critique.
Executive Summary
This study examines autophagic flux in human CD4⁺ T cells from younger (23–35 yrs) vs older (67–93 yrs) healthy donors to test whether autophagy declines with human age (as animal studies often show) or is preserved. Unexpectedly, the authors report that the older-donor T cells show higher autophagy flux (measured via LC3 + compartments and response to lysosomal inhibition) compared to younger donors, while the total clearance of autophagosomes was comparable. They conclude that rather than a generalized decline in autophagy, in healthy older adults there may be a compensatory enhancement of autophagy in CD4⁺ T cells, which could underlie “healthy aging”. The paper suggests that maintenance (or up-regulation) of autophagy in immune cells might be a protective mechanism rather than simply a feature of youthful cells. For longevity/healthspan research this shifts the paradigm from “autophagy declines with age” to “autophagy may be maintained or even elevated in selected healthy older individuals”.
Bullet Summary
- Background: Autophagy is tightly linked to proteostasis, mitochondrial quality control, and longevity. Animal models show autophagy declines with age and that boosting autophagy improves lifespan.
- Knowledge gap: In humans, particularly in immune (CD4⁺ T) cells, it is unclear if autophagy declines with age or remains intact.
- Objective: Compare basal and induced autophagy flux in CD4⁺ T cells from younger vs older healthy donors.
- Methods:
- Donor groups: younger (23-35 yrs) vs older (67-93 yrs) healthy individuals.
- Immunofluorescence for LC3 (autophagosome/autolysosome marker) and LAMP2 (endolysosomal marker).
- Pharmacologic manipulations: bafilomycin A1 (to block lysosomal acidification) and CCCP (mitochondrial uncoupler) to test inducible autophagy and mitophagy.
- Key findings:
- Older donor CD4⁺ T cells had more LC3⁺ compartments per cell than younger donor cells under basal conditions.
- Autophagic flux (e.g., difference with vs without bafilomycin) was higher in older donor cells.
- Despite more LC3 + compartments, the total number of autophagosomes degraded over the measurement period was comparable between young and old groups → suggests older donor cells may have lower autophagosome biogenesis but enhanced flux/clearance efficiency.
- Interpretation: Rather than a decline, in healthy older adults the autophagy system in T cells appears maintained or possibly up-regulated. The authors infer this may support immune function and contribute to healthy aging (i.e., the older donors are “healthy” rather than frail).
- Implications: This challenges the “autophagy declines with age” narrative (at least in humans and at least in CD4⁺ T cells), and suggests therapeutic focus might shift to supporting autophagy in aging immune cells rather than simply assuming it is failing.
- Limitations (acknowledged by authors): Cross-sectional design (not longitudinal), limited to CD4⁺ T cells (not other cell types/tissues), healthy donor selection may bias toward “successful aging” individuals, using surrogate markers (LC3, LAMP2) rather than full multi-omics autophagy pathway read-outs.
- Conclusion: Maintenance (or enhancement) of autophagy in human CD4⁺ T cells is compatible with healthy aging, and may represent a biomarker/target for longevity interventions.
Claims / Evidence Table
| Claim |
Evidence Provided |
Notes / Caveats |
| Autophagy flux is higherin CD4⁺ T cells from older healthy donors vs younger donors |
Immunofluorescence data showing more LC3⁺ puncta, higher response to bafilomycin/CCCP in older donor cells. |
Flux measurement via indirect proxies (LC3, LAMP2) rather than e.g., mass spectrometry of autophagy substrates. Also, sample size & donor variability matter. |
| Autophagosome clearance is comparable between young & old donor T cells |
Authors report that despite more LC3 + puncta in older donor cells, the total amount degraded is similar → implies enhanced flux rather than build-up. |
The time-window and experimental manipulations may miss subtler dynamics. Also, only CD4⁺ T cells studied. |
| Autophagosome biogenesis may be reduced in older donor T cells |
Because older donor cells had more LC3 + compartments but similar clearance, authors infer biogenesis may be lower but balanced by higher flux. |
This is inferential rather than directly measured (e.g., by Atg gene expression or real-time autophagosome formation assays). |
| Preservation/enhancement of autophagy may underlie healthy aging |
Based on older healthy donor cohort showing maintained autophagy, authors propose this mechanism might support immune resilience and longevity. |
Correlation only. The older donors are “healthy” survivors; selection bias. Doesn’t prove causation. |
| The simple assumption that autophagy declines in all aging humans may be incorrect |
The data show a counter-example (CD4⁺ T cells in healthy older donors) to the dogma of decline. |
The result may not generalize to other cell types, to unhealthy older individuals, or to in vivo organismal autophagy. |
Novelty
Here’s what is new / interesting in this paper (given your interest in longevity / immunosenescence).
-
Human primary immune cell data: While much of the autophagy-aging literature is in model organisms (worms, flies, mice) or non-immune tissues, this paper uses human CD4⁺ T cells from actual younger vs older donors. That’s a valuable translational step.
-
Counter-intuitive finding: Rather than autophagy decline, the authors find increased flux in older donor T cells — this flips a commonly assumed narrative and suggests we need to refine the “autophagy declines with age” model in humans.
-
Focus on health‐span rather than disease‐state: The older donor cohort is “healthy” (not frail, not heavily comorbid), so the results may reflect mechanisms of successful aging rather than typical aging/frailty. That aligns with your interest in longevity.
-
Potential biomarker/target angle: If immune cell autophagy maintenance correlates with healthy aging, this suggests a new biomarker domain (T-cell autophagy flux) or intervention target (immune‐autophagy modulators) for longevity tech.
-
Bridges immunology & aging fields: By focusing on CD4⁺ T cells, the paper links autophagy with immunosenescence — the decline in immune function with age — which is a key lever in longevity and health-span research.
Critique (strengths & weaknesses)
Strengths
- The human donor design is a strength: working with human CD4⁺ T cells gives relevance for translational aging research (important given your biotech/health-longevity orientation).
- The combination of basal vs induced autophagy measurements adds depth rather than just snapshot measurements.
- The authors are appropriately cautious in interpretation (they don’t over-claim causality) and discuss limitations.
- The focus on healthy older donors is strategic: studying “successful agers” helps isolate protective mechanisms instead of disease confounders.
Weaknesses / Limitations
-
Cross-sectional design: They compare young vs older individuals at one time point each. Without longitudinal data, you cannot say whether autophagy changed with aging in the same individuals or whether the older healthy group is a selected survivor cohort with inherently higher autophagy.
-
Selection bias / cohort limited: The older donors are healthy; they may represent a subset of older adults with above-average resilience. It’s unclear how generalizable the results are to “typical aging” or those with comorbidities.
-
Cell-type specificity: Only CD4⁺ T cells were studied. While important, we don’t know if other immune subsets (CD8+, B cells, NK cells), or non-immune tissues, behave similarly. For longevity/healthspan interventions, systemic autophagy matters.
-
Proxy measurements: The authors use LC3 and LAMP2 immunofluorescence, and pharmacologic perturbation (bafilomycin/CCCP) to infer autophagic flux. These are standard but indirect; more quantitative measures (e.g., proteomic autophagy substrate turnover, gene expression of autophagy regulators, live-cell imaging of autophagosome formation/clearance) would strengthen conclusions.
-
Mechanism not deeply probed: While the observation is novel, the paper does not deeply investigate why older donor T cells have enhanced flux — which pathways, regulators, upstream triggers are responsible (e.g., nutrient sensing, lysosomal capacity, mTOR/AMPK signaling, mitophagy specificity).
-
Functional outcome unclear: The study shows higher flux, but does it translate into better T-cell function (cytokine production, proliferation, response to pathogens) in older donors? For longevity relevance you’d like to see immune function correlates.
-
May not reflect organismal aging: T-cell autophagy is important but organismal aging involves many tissues, systemic inflammation, metabolic regulation, senescence, stem cell exhaustion, etc. So using this one cell type as a proxy for “healthy aging mechanism” is a bit of a stretch without broader validation.
Actionable Insights (for your health-longevity / biotech agenda)
Given your interest in longevity, immune/biomarker optimization and health-span product development, here are some ideas:
-
Consider T-cell autophagy flux as a biomarker: This paper suggests that measuring autophagic flux in CD4⁺ T cells (or other immune cells) could serve as an indicator of “healthy aging” status (resilience) rather than simple “age”. Developing an assay (flow cytometry based, LC3 puncta count or better) might be a novel lead-gen tool for a longevity diagnostics platform.
-
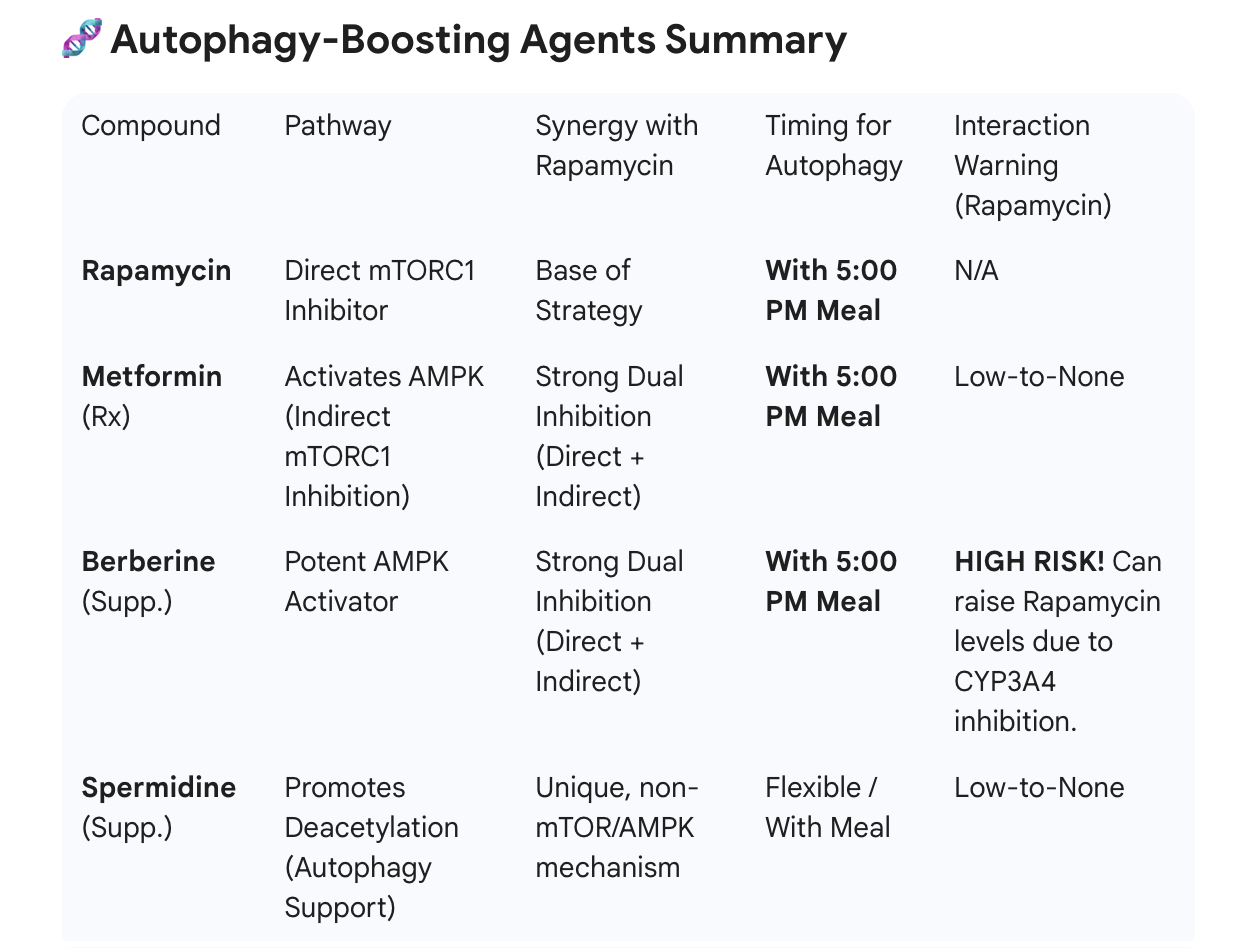
Interventions that support immune/autophagy axis: Since the study supports that immune cell autophagy is maintained in healthy older adults, you might explore whether existing or novel interventions (dietary, pharmacologic, nutraceutical) that enhance autophagy in T cells (e.g., spermidine, rapalogs, intermittent fasting, exercise) can shift immune autophagy flux upward and whether that correlates with improved immune resilience in older clients.
-
Stratify longevity cohorts by autophagy measures: If you are involved in designing digital tools or content for longevity clients, you may incorporate autophagy flux (immune cell) as one stratifier to distinguish “high resilience agers” vs. “low resilience agers” and tailor interventions accordingly.
-
Develop translational studies: If you’re engaged in biotech or product development, this opens a path: design a small trial in older adults measuring CD4⁺ T-cell autophagy flux before/after an intervention (exercise, caloric restriction mimetic, immunomodulator) to test if flux can be modulated and whether that correlates with improved immune biomarkers (e.g., vaccine response, T-cell proliferative capacity, immunosenescence markers). That could feed into a lead-gen narrative for a longevity clinic or product launch.
-
Caveat: Focus on “healthy aging” segment: Recognize that the paper studies healthy older donors. Many older individuals have comorbidities, chronic inflammation, immunosenescence, etc. Any product/diagnostic you design must segment accordingly and not over-generalize.
Technical Deep Dive & Further Critique
Given your STEM/biotech interest, here are deeper technical points worth noting:
- The assay: Use of LC3 (microtubule-associated protein 1 light chain 3) is standard for marking autophagosomes/autolysosomes. LAMP2 marks late endosome/lysosome compartments. The combination plus blockade with bafilomycin A1 (which prevents lysosomal acidification and thus degradation) allows measurement of “flux” (i.e., accumulation when clearance is blocked). The authors also used CCCP to induce mitochondrial damage (mitophagy stimulus). These are sound approaches.
- Interpretation nuance: The finding of more LC3 + puncta in older donor cells could be interpreted as “accumulation due to reduced clearance” (which would indicate dysfunction). But the authors show clearance (decay) is equivalent, hence they infer clearance is intact but production is adjusted (i.e., biogenesis reduced but flux increased). The logic is sound but somewhat inferential: they don’t measure biogenesis rate directly (e.g., via Atg gene expression or live autophagosome formation imaging). They infer from static counts + flux experiments.
- Sample size & donor variability: The older donor age range (67–93 yrs) is broad; there could be substantial heterogeneity. Variation in lifestyle, diet, medications, sub-clinical morbidities could confound. It’s unclear how well matched the younger vs older groups are in terms of other variables (sex, smoking history, BMI, latent disease). Without access to full paper I can’t verify how well controlled these are.
- Functional link: While the flux difference is interesting, the paper stops short of linking the higher autophagy flux to improved immune function (e.g., fewer senescent T cells, better proliferative capacity, improved vaccine response). That is a missed opportunity for mechanistic depth.
- Causality vs correlation: Because this is cross‐sectional, we don’t know whether preserved/high autophagy is a cause of healthy aging or simply a marker of individuals who already aged well. It might be that those older individuals who had inherently higher autophagy survived and are now the “healthy old” pool (survivor bias). Longitudinal work would help.
- Tissue / system generalizability: CD4⁺ T cells are but one component of aging physiology. It remains possible that other cell types/tissues (muscle, liver, brain) still show autophagy decline with age even if immune cells do not. For a biotech/healthspan product you’d need to test across multiple cell/tissue types. The paper should thus be seen as a piece of the puzzle, not the whole.
- Mechanistic pathways: The authors don’t deeply explore upstream regulators of enhanced flux in older donor T cells: for example, changes in mTORC1/AMPK signaling, lysosomal biogenesis (TFEB), mitochondrial quality control (PINK1/Parkin), or nutrient sensing (insulin/IGF). Given your biotech interest, you might want to know those mechanistic nodes to design interventions. The paper leaves open that question.
- Clinical translation: The leap from T-cell autophagy flux to viable interventions is non-trivial. Even if flux is higher, we need to know threshold values, inter-individual variability, reproducibility, and whether manipulation of flux yields meaningful functional/clinical gains (reduced infections, improved vaccine responses, delayed immunosenescence). Those are future steps.
- Statistical/reporting transparency: Without full access I cannot assess whether they adjusted for confounders (sex, comorbidities, medication use) in their comparisons, whether the data are normally distributed, whether multiple comparison corrections were applied, and whether effect sizes are large enough to matter biologically (vs statistically). For product/clinical translation you’d want effect size data (e.g., fold‐change in flux, variation across donors) and reproducibility.
My Final Take
For your longevity/healthspan focus, this paper is meaningful: it provides human-cell data suggesting that autophagy in immune cells may not necessarily decline with age in “healthy agers” and that preserving or boosting immune cell autophagy could be a targetable mechanism. The shift from “decline” to “maintenance/enhancement” is important, because it reframes interventions (you might aim to support autophagy rather than simply restore it). It also suggests the value of immune cell autophagy as a biomarker for resilience.
That said, from a product/biotech standpoint, it’s still early stage: the data is correlative, limited in scope (one cell type), cross-sectional, and mechanistic underpinnings are weak. If you are evaluating building diagnostics or therapeutics around this concept, you will want follow-up studies: longitudinal cohorts; interventions showing modulation of T cell autophagy flux; linking flux changes to improved immune outcomes; expanding to other immune subsets and tissues; exploring upstream modulators (nutrient sensors, lysosomal regulators, mitophagy pathways); and defining normative ranges for “healthy” vs “low resilience” autophagy flux.
In terms of critique, the main risk is over-generalizing: just because CD4⁺ T cell autophagy appears preserved in healthy older adults doesn’t mean systemic autophagy in all tissues is preserved, or that boosting autophagy will necessarily translate into improved healthspan. Also, the “healthy older donor” selection means results may not translate to typical aging populations with comorbidities.