I get the same issues, particularly the fatigue and low motivation when I take it. I just don’t understand why and I have tried both low and high doses
Dude yea. I might try ultra low dose by splitting one of my capsules into 20 capsules and taking it 2-3 times a week in the future but for now I want to get back to how I was before this. I feel just awful on it. Fatigued, low motivation, didn’t exercise anywhere near as much, anxious, grumpy. Ugh.
Did you mention your baseline thyroid labs anywhere?
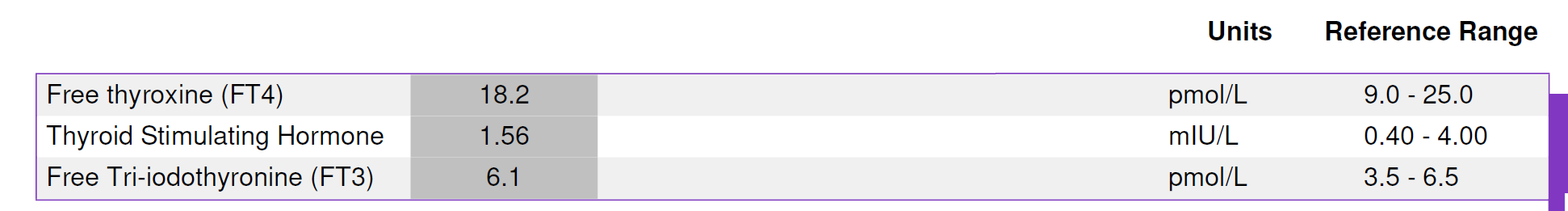
Honestly seemed fine I was just curious what benefit I might get from adding in some thyroid. Also I am using growth hormone at the moment and I did hear that adding in some thyroid (or t4 or t3?) can be beneficial while using that. Note that these labs were done before adding in growth hormone.
Some ideas you could consider -
-high dose t4 only (300mcg/day).
-TRH ( Thyrotropin-releasing hormone) which seems to be more hypothalamus than pituitary.
-You ever tried a dopamine reuptake inhibitor like ritalin, wellbutrin, vyvanse? I recall you tried the modafinil, but these products are a little bit different.
While both overt hyperthyroidism (suppressed TSH, high free T4/T3) and overt hypothyroidism (very high TSH, low free T4) are associated with significantly increased morbidity and mortality in all age groups, those of us nearing 70 or older may want to evaluate their thyroid status differently by considering that borderline low T4 with borderline high TSH may be associated with longevity. The Leiden Longevity Study identified a thyroid phenotype characterized by higher-than-average TSH levels in conjunction with free T4 levels in the low-normal range. This suggests a centrally-mediated reset of the hypothalamic-pituitary-thyroid axis. This state may be a heritable trait associated with a slower metabolic rate and, ultimately, a longer, healthier lifespan but it might also be modifiable, conferring similar benefits.
There are a number of studies and findings on this topic (not mentioned here) that older adults may find interesting. The generalization is that a low normal or even mildly subclinical hypothyroid state is not detrimental in those over 75-80 and, in fact, appears to be a biomarker for, or contributor to, exceptional longevity. Conversely, a high normal or subclinical hyperthyroid state is consistently associated with increased mortality and cardiovascular risk in this population. IMO, the utility of standard TSH reference ranges derived from younger populations is greatly diminished when applied to older adults. Treatment for mild hypothyroidism at these ages may interfere with a potentially adaptive, pro-longevity metabolic state.
T4 only wasn’t good for me either. My reverse T3 is already high but my hope was to take enough that it would still convert to just enough T3 but my lab level was lower than at baseline.
I actually did try injecting TRH years ago when my symptoms were really bad but I didn’t notice any difference at all.
My symptoms are much much better these days anyway. I just wonder if I’m leaving some energy on the table by having a Free T3 just below 3.
No I’ve never tried the amphetamines
Did you copy this from a link or did you type all this yourself? If there’s a link, I’d be interested in checking it out
These are my thoughts @LukeMV based on a synthesis of reading over the years. You will find many sources related to this discussion. Here are a couple of links I have handy. With a little searching, you will find others even more on point.
More broadly, thyroid function is not the only functional component in which one can find counterintuitive evidentiary trends. SHBG levels in the elderly is another that comes to mind.
Ah ok. That’s cool you tried injecting TRH! Good to hear your symptoms are much better.
That’s a tough call about the free t3 levels and energy.
If you have never tried ADHD medication (or other reuptake inhibitors) it’s something to try one day.
As there are 3 popular reuptake classes (dopamine, noradrenaline, serotonin) so some people stack various products. Some products have 2 in 1 etc.
Usually serotonin paird with dopamine or noradrenline. Some people do all 3.
I don’t believe Wellbutrin is an amphetamine. A lot of online pharmacies carry it.
Some people on this forum use it with good reviews. It appears to be a bit similar modafinil but more of a energy/motivation feel. Kinda like a more narrow focus (intense concentration).
Don’t know if you’ve read about Nandrolone use and it’s effect on neurotransmitters, but there are some interesting articles on animals/rodents. I’ve seen articles saying it can increase or decrease certain chemicals. Not sure what to think on it however.
https://www.sciencedirect.com/science/article/abs/pii/S0039128X13002195
Just linking a post on the subject from 2023
From chat GPT
Looking much deeper than this basic prompt, you will see an interesting set of relationships for older adults.
FWIW …
Attia’s podcast on thyroid.{11/17/2025]
Now all trip over themselves,.
My comment;
Wilson was correct over 30 years ago.
“If you wait until you are ready, it is almost certainly too late.”
~Seth Godin
Great interview. The news of a Free T3 LC/MS test existing and being more reliable than the standard one is huge information to me. I wish he discussed what the results of this test could mean.
I thought you’d enjoy that episode. And no doc has ever told me about that test, either. Fyi, I see on Good Labs it’s available from Quest for $27
I also didn’t know it led to worse lipids etc, even if your levels are corrected.
I find the entire topic confusing and will listen to the episode again. Did I miss them talking about the ideal levels?
Oh yes there’s definitely a correlation between low thyroid levels and higher LDL.
Unfortunately, they didn’t discuss optimal results except for TSH really.
I’m going to try and get a Free T3 LC/MS as well
Journal Article
Published 01, Dec 2016(yes almost a decade)
DIAGNOSIS OF ENDOCRINE DISEASE: “How reliable are free thyroid and total T3 hormone assays”
This is behind a pay wall
https://academic.oup.com/ejendo/article-abstract/175/6/R255/6654920
A summary of this Podcast by Peter Attia, etc.
ChatGPT5.1 Summary:
1. Executive Summary (High-Level Takeaways)
Thyroid physiology is far more intricate than routine clinical screening implies. While most clinicians treat thyroid disease as a “TSH and free T4” problem, the reality is that T3 drives biological activity, and intracellular conversion via deiodinases (D1, D2, D3) determines whether individual tissues experience adequate thyroid signaling. A patient can appear “normal” on labs while specific organs are functionally hypothyroid or hyperthyroid.
In hypothyroidism, Hashimoto’s autoimmune thyroiditis dominates, but a variety of less common etiologies exist. Diagnosis is usually made via elevated TSH with low free T4, but there are subtler cases where pituitary dysfunction, assay interference, medication effects, or chronic illness distort interpretation. Symptoms are notoriously nonspecific: fatigue, weight gain, cold intolerance, dry skin, constipation, hair changes, and cognitive slowing.
Treatment revolves around levothyroxine (T4), but dosing, absorption, adherence, drug interactions, and genetic factors (e.g., DIO2 polymorphisms) create wide inter-individual variability. Some patients report persistent symptoms despite normalized labs; the debate over combination therapy (T4+T3) remains unresolved, with limited evidence supporting broad use but possible benefit in select subgroups. Conversely, overtreatment is common and dangerous: excess thyroid hormone increases risk of atrial fibrillation, bone loss, and arrhythmia.
The interview emphasizes that clinicians should think beyond template protocols — recognizing atypical presentations, carefully evaluating persistent symptoms, and individualizing therapy while avoiding dogma on either side of the T3 debate.
2. Bullet Summary (Key Points)
- T3 is the active hormone; tissue-level thyroid status depends on local deiodinase activity, not just serum labs.
- TSH + free T4 is an oversimplification; labs often fail to reflect organ-specific thyroid signaling.
- Hashimoto’s is the most common cause of hypothyroidism in developed countries.
- Symptoms are nonspecific and overlapping with depression, anemia, menopause, and chronic fatigue.
- Subclinical hypothyroidism requires judgment; treatment isn’t automatically indicated.
- Central (pituitary) hypothyroidism breaks the normal TSH–T4 pattern and is often missed.
- Levothyroxine absorption varies with food, supplements, gut issues, and medications.
- Many patients feel unwell despite “normal” labs — but evidence for adding T3 is mixed.
- A minority with DIO2 polymorphisms may respond better to combination therapy.
- Overtreatment is common and raises fracture and atrial fibrillation risk.
- Thyroid nodules are common and usually benign; ultrasound stratification guides biopsy.
- Silent thyroiditis causes transient hyper → hypo → recovery patterns.
- Hyperthyroidism (Graves’, toxic nodules) is less common but clinically dramatic.
- Graves’ disease involves TSH-receptor–stimulating autoantibodies.
- Treatment options include antithyroid medications, radioactive iodine, or surgery.
- Thyroid eye disease can occur independently of thyroid hormone levels.
- Aging shifts TSH upward; mild elevations may be physiologic rather than pathologic.
- Lab interpretation must consider pregnancy, illness, meds, and assay artifacts.
- “Normal range” is not universal — population and lab variations matter.
- Clinical judgment is essential; algorithms alone miss atypical cases.
Full text of response:
And testosterone! A decent % of guys with slight hypogonadism (ie total T in the 300-400 range) would benefit from addressing thyroid issues, which in turn fixes testosterone. Another well-known gym bro fact which turned out to be true!