I feel like we don’t discuss thyroid health much on here so I’m hoping to get a discussion going.
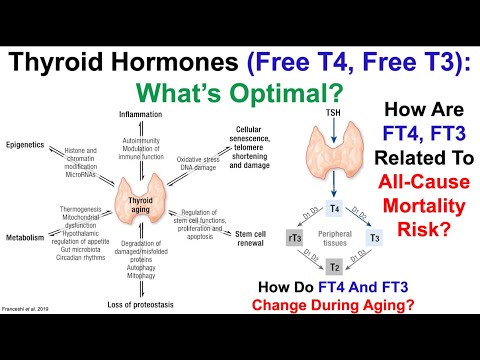
In my personal case, I have an optimal TSH (1.6) and Free T4 (1.4), but my Free T3 runs on the low end of the normal range (2.7).
I have a bunch of links saved in my notes so I’m going to share them here.
The impact of thyroid hormone dysfunction on ischemic heart disease. 2019 study
Thyroid Dysfunction in Heart Failure and other Cardiovascular Outcomes
https://www.ahajournals.org/doi/10.1161/CIRCHEARTFAILURE.118.005266?fbclid=IwAR0UUzJVMK5mcownP4vOEKES1urH5Vjqc-bC0krT2hR5UcPcUKBIcePi57A&
Thyroid Replacement Therapy and Heart Failure
http://circ.ahajournals.org/content/122/4/385.extract
Thyroid Hormone and Cardiac Disease: From Basic Concepts to Clinical Application
The Role of Thyroid Hormone Therapy in Acutely Ill Cardiac Patients
T3 Therapy Lowers the Incidence of Atrial Fibrillation After Cardiac Operations
http://www.annalsthoracicsurgery.org/article/0003-4975(96)00102-6/abstract
T3 Effects on Cardiovascular System in Patients with Heart Failure
Relation Between Free T3/Free T4 Ratio, Echocardiographic Parameters and Mortality in Dilated Cardiomyopathy
http://onlinelibrary.wiley.com/doi/10.1016/j.ejheart.2004.04.016/full
Low-T3 Syndrome: A Strong Prognostic Predictor of Death in Patients with Heart Disease
http://circ.ahajournals.org/content/107/5/708.full
Low Thyroid Hormone Increases Risk of Death from Heart Attack by 70%
Low T3 Syndrome: A Strong Predictor of Low Cardiac Output and Death in Patients Undergoing Coronary Artery Bypass Grafting
http://www.annalsthoracicsurgery.org/article/S0003-4975(14)00328-2/fulltext
Acute Effects of T3 Replacement Therapy in Patients with Chronic Heart Failure and Low-T3 Syndrome
http://press.endocrine.org/doi/full/10.1210/jc.2007-2210
Safety and Hemodynamic Effects of Intravenous T3 in Advanced Congestive Heart Failure
Low T3: A Strong Predictor of Outcome in Acute Stroke Patients
-
Symptomatic Relief is Related to Serum Free Triiodothyronine Concentrations during Follow-up in Levothyroxine-Treated Patients with Differentiated Thyroid Cancer - Larisch, Midgley , Dietrich and Hoermann. See: Thieme E-Journals - Experimental and Clinical Endocrinology & Diabetes / Abstract (This paper clearly proves that FT3 concentrations are the most important in clinical decision making, as they are most closely linked to residual hypothyroid symptoms in T4- Only treated patients. It also shows that in-range TSH is not sufficient for symptom relief.).
-
Homeostatic equilibrium between free thyroid hormones and pituitary thyrotropin are modulated by various influences including age, body mass index and treatment - Hoermann R1, Midgley JE, Giacobino A, Eckl WA, Wahl HG, Dietrich JW, Larisch R. See: Homeostatic equilibria between free thyroid hormones and pituitary thyrotropin are modulated by various influences including age, body mass index and treatment - PubMed ((This is a great paper, although complex. It shows that it is the relationships of the thyroid hormones, and how they adjust during treatment, that counts. It also makes it crystal clear that TSH should only have a supporting role in the assessment process during treatment.)
-
Recent Advances in Thyroid Hormone Regulation: Toward a New Paradigm for Optimal Diagnosis and Treatment - Hoermann, Midgley, Larisch, Dietrich. See: Frontiers | Recent Advances in Thyroid Hormone Regulation: Toward a New Paradigm for Optimal Diagnosis and Treatment
-
Thyroid hormone replacement - a counterblast to guidelines - Dr A.D. Toft. See: http://www.rcpe.ac.uk/sites/default/files/jrcpe_47_4_toft.pdf
-
Consensus statement for good practice and audit measures in the management of hypothyroidism and hyperthyroidism - M P J Vanderpump, J A 0 Ahlquist, J A Franklyn, R N Clayton, on behalf of a working group of the Research Unit of the Royal College of Physicians of London, the Endocrinology and Diabetes Committee of the Royal College of Physicians of London, and the Society for Endocrinology See: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2351923/pdf/bmj00557-0041.pdf
In patients with a left ventricular ejection fraction of greater than 40% (study II), triiodothyronine (T3) administration resulted in significantly improved stroke volume (p less than 0.01) and cardiac output (p less than 0.02) and reduced systemic (p less than 0.01) and pulmonary (p less than 0.05) vascular resistances. There were no adverse reactions to triiodothyronine in the dosages that were used. Triiodothyronine appears to be beneficial to all patients undergoing open heart surgery.