High BP can kill you slowly, Low BP can kill you fast.
For adults over the age of 60, low blood pressure is generally defined as Systolic: Less than 90 mmHg, Diastolic: Less than 60 mmHg
“cardiovascular disease risk doubles for every 20 mmHg systolic or 10 mmHg diastolic
increase in blood pressure, starting at 115/75 mmHg. This means that the risk of death from stroke and ischemic heart disease (IHD) increases linearly and progressively from levels as low as 115 mmHg SBP and 75 mmHg DBP upward. These increased risks are present in individuals ranging from 40 to 89 years of age.”
It looks like 115/75 would probably be close to the sweet spot for most older people.
This would be for healthy people. Low blood pressure is a comorbidity of vascular diseases,
etc., in old people.
Found a few other relevant resources from the senior author and perhaps world leader in AD prevention:
Perfecting a Cocktail of Approaches to Treat Alzheimer Disease: Richard Isaacson, MD
Sep 27, 2023
The director of the Center for Brain Health and Alzheimer Prevention Clinic at Florida Atlantic University provided perspectives on the multimodal, multitargeted approach needed to treat Alzheimer disease. [WATCH TIME: 5 minutes]
An overview of biomarkers and a bit of what the future holds
MASTER CLASS WITH DR. RICHARD ISAACSON
Alzheimer’s Prevention
Get practical, up-to-date information on Alzheimer’s risk reduction from Dr. Isaacson’s Alzheimer’s Prevention Clinic
20 free short videos
Lastly, this might be helpful that he mentioned in his video:
Retain Your Brain is a research study funded by the National Institutes of Health
- Learn about Alzheimer’s disease and how to manage your risk
- Contribute to research, improving future Alzheimer’s treatments
- Participate online, no travel necessary
Thanks, just followed them on Scholar:
I emailed them in Feb to ask about SGLTi, BPV (instead of just mean BP), low-dose lithium, neuromodulation (inc. light therapy), and non-statin lipid-lowering drugs (inc. obicetrapib). No answer so far.
(By the way, the article was shared by “Drlipid”, he posts great content.)
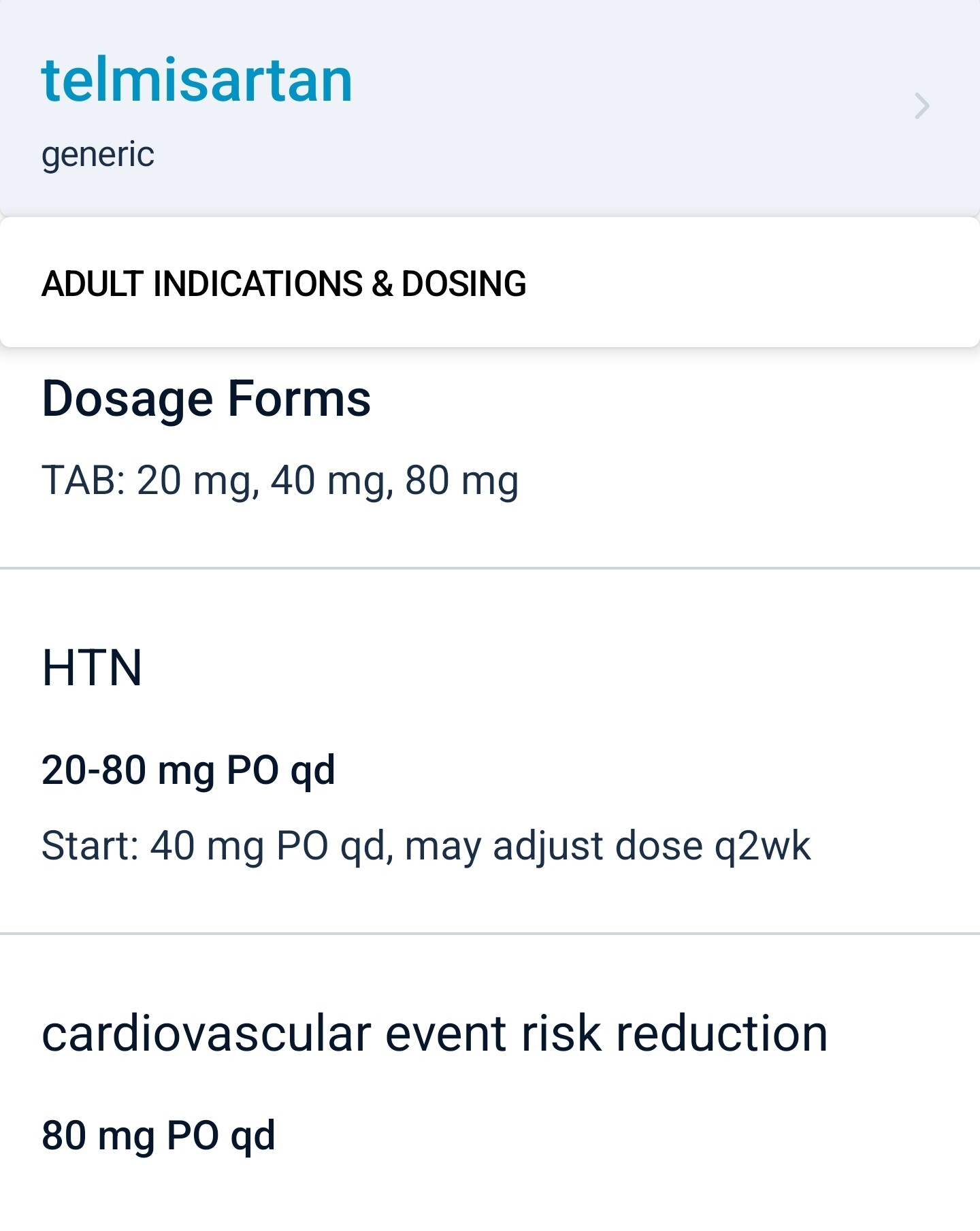
80mg daily is also the only FDA-approved dose for “cardiovascular event risk reduction”, so maybe this is related mechanistically (?)
You wrote: " Also, can you recommend a good blood pressure device that is accurate but does not break the bank?"
Sure, Buy a Littman Stethoscope for $60 on zon and a blood pressure cuff that is the proper size.
There are some good youtube videos on how to read it. It’s a bit intimidating at first but after a dozen tries you’ll get quite accurate.
No batteries, and it never breaks… and you can listen to your lower right lung lobe and tell you are getting pneumonia (it usually starts there) early.
Where do you see this?
It’s in the clinical medicine app I use called epocrates. The free web version is at epocrates.com
“Telmisartan is, therefore, the only ARB with a broad indication for CV risk reduction in patients with atherothrombotic disease or diabetes with end-organ damage.”
I am a fan of Telemsartan, I was previously using Losartin, but I switched.
“Telmisartan has a number of pharmacological properties that distinguish it from other angiotensin II receptor blockers (ARBs) - the longest plasma half-life, highest lipophilicity and strongest receptor binding affinity in class”
“With publication of the ONTARGET
data, telmisartan is alone among the ARBs in providing CV risk reduction in a broad range of patients typically treated in primary care. So far, no other ARB has achieved this indication.
Therefore, telmisartan is likely to remain at the forefront of CV risk management strategies in the future.”
Link to the full article:
https://sci-hub.se/10.1586/ecp.10.141
Maybe if you are taking omega 3, you can take it alongside your 40mg Telmisartan tablet to enhance its ppar gamma effects ?
https://www.cell.com/cell-metabolism/pdf/S1550-4131(20)30237-0.pdf
Thanks a lot. Telmisartan is really a no brainer as the first-line anti hypertensive.
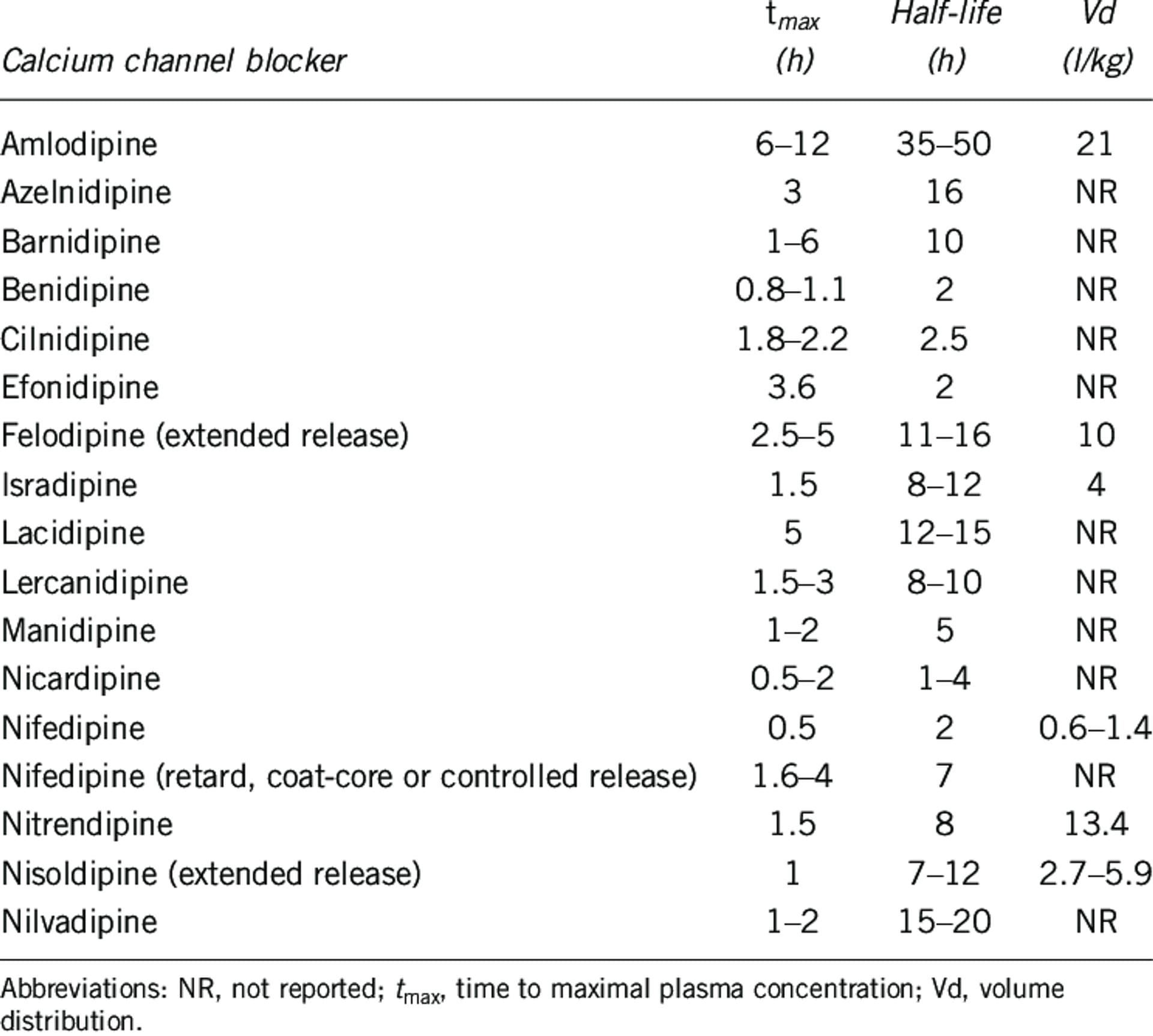
For the second line, amlodipine seems the way to go (long half life [40h] + dihydropyridine + reduced edema risk when combined with telmisartan) but the Ora Biomedical results suggest that two other dihydropyridine CCBs might be even better for longevity: benidipine (half life 2h) and azelnidipine (16h). We need more data in humans but azelnidipine seems interesting:
- Same BP lowering effect as amlodipine but without causing tachycardia: Efficacy and Safety of Azelnidipine as an Antihypertensive Compared to Amlodipine: A Systematic Review and Meta-analysis | High Blood Pressure & Cardiovascular Prevention
- Some neuroprotective properties? Azelnidipine Attenuates the Oxidative and NFκB Pathways in Amyloid-β-Stimulated Cerebral Endothelial Cells - PMC
See also: Benidipine calcium channel blocker promotes the death of cigarette smoke-induced senescent cells and improves lung emphysema 2023
Aside from the well-known senolytic, ABT-263, we identified other potentially new senescence-eliminating compounds, including a new class of molecules, the dihydropyridine family of calcium voltage-gated channel (CaV) blockers. Among these blockers, Benidipine, decreased senescent lung cells and ameliorates lung emphysema in a mouse model. The dihydropyridine family of CaV blockers thus constitutes a new class of senolytics that could improve lung diseases. Hence, our work paves the way for further studies on the senolytic activity of CaV blockers in different senescence contexts and age-related diseases.
Strikingly, 4 different molecules targeting voltage-gated calcium channels (CaV), namely Benidipine, Cilnidipine, Felodipine and Lacidipine, displayed potential senolytic activities on CS-induced senescent cells. To confirm this senolytic activity, we assessed Benidipine, or Cilnidipine, on control and CS-induced senescent cells and observed a clear specific decrease cell number and density of senescent cells without impacting the non-senescent cells (Figure 1C, ,1D1D and Supplementary Figure 2A, 2B). This decreased cell number correlated with senescent cell death as assessed by the quantity of blue trypan positive cells (Figure 1E).
The half-life of felodipine and lacidipine is OK:
Interestingly, lacidipine does not cause edema: Comparative peripheral edema for dihydropyridines calcium channel blockers treatment: A systematic review and network meta-analysis 2022
Nifedipine ranked highest in inducing peripheral edema (SUCRA 81.8%) and lacidipine (SUCRA 12.8%) ranked the least. All DHPCCBs except lacidipine resulted in higher relative risk (RR) of peripheral edema compared with placebo. Nifedipine plus angiotensin receptor blocker (SUCRA: 92.3%) did not mitigate peripheral edema and amlodipine plus angiotensin-converting enzyme inhibitors (SUCRA: 16%) reduced peripheral edema the most. Nifedipine ranked the highest and lacidipine ranked the lowest amongst DHPCCBs for developing peripheral edema when used for cardiovascular indications. The second or higher generation of DHPCCBs combination with ACEIs or ARBs or diuretics lowered the chance of peripheral edema development compared to single DHPCCB treatment.
Lacidipine and lercanidipine might be good alternatives to amlodipine in patients who develop edema, but otherwise, I feel like there’s not enough data to recommend them instead of amlodipine first.
Then, for the third-line treatment, my bet is on indapamide SR, but we don’t have much data…
I dug further into CCBs. It’s complex as there are different generations, dihydropyridine (DHP) vs. non-DHP, L-type, T-type, N-type (and their combinations), BBB-crossing or not, centrally vs. peripherally, lipophilic or not, etc.
Amlodipine is a peripheral-acting third-generation L-type DHP CCB that does not cross the BBB easily.
Some papers suggest that DHP CCBs that cross the BBB easily (e.g. felodipine, isradipine, lacidipine, lercanidipine, nicardipine, nifedipine, nimodipine, nisoldipine, and nitrendipine) are better:
In people with no prior history of psychiatric or neurodegenerative disorder, there was a significantly lower incidence of most disorders with BP-CCBs compared to amlodipine, with risk ratios ranging from 0.64 to 0.88 and an overall risk ratio of 0.88, i.e. a risk reduction of 12%.
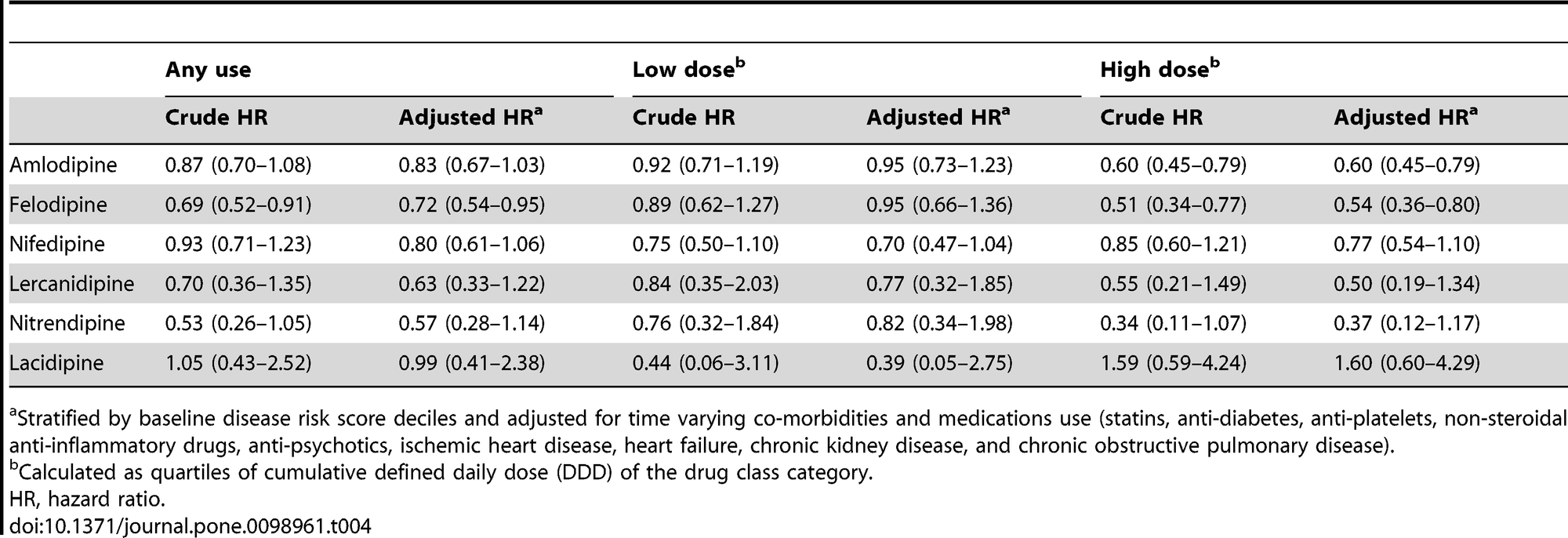
Antihypertensive Agents and Risk of Parkinson’s Disease: A Nationwide Cohort Study 2014
Due to the differences in lipophilic properties, we further distinguished CCBs into the central-acting ones that could cross the blood-brain barrier (felodipine, nifedipine, lercanidipine, nitrendipine and lacidipine) and the peripheral-acting ones that are thought to not cross blood-brain barrier as readily (amlodipine, verapamil, and diltiazem). We found any use of central-acting CCBs, rather than peripheral-acting ones, was associated with a decreased risk of PD (adjusted HR, 0.69; 95% CI, 0.55–0.87, table S4). Among the individual dihydropyridine CCB, the use of felodipine was found to have a reduced association with PD, with a potential dose-response relationship (HR, 0.72; 95% CI, 0.54–0.95 for any use; HR, 0.54; 95% CI, 0.36–0.80 for higher cumulative use). There was also a decreased association between higher cumulative use of amlodipine and risk of PD.
Non-amlodipine CCBs don’t do as well as amlodipine for PD prevention in the above paper, but they’re also used way less often, which might explain the wider CIs.
Felodipine seems interesting: Neuro-modulatory impact of felodipine against experimentally-induced Parkinson’s disease: Possible contribution of PINK1-Parkin mitophagy pathway 2024
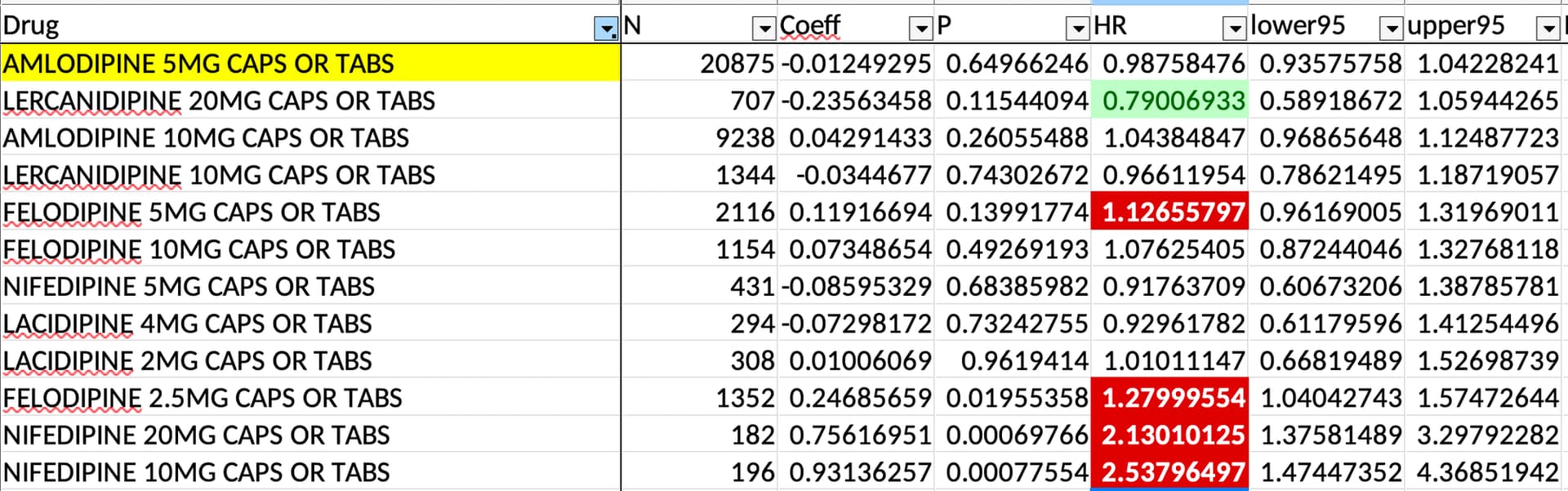
But in the EPITERNA study, only lercanidipine 20 mg might do a bit better than amlodipine 5 mg and felodipine didn’t look especially good:
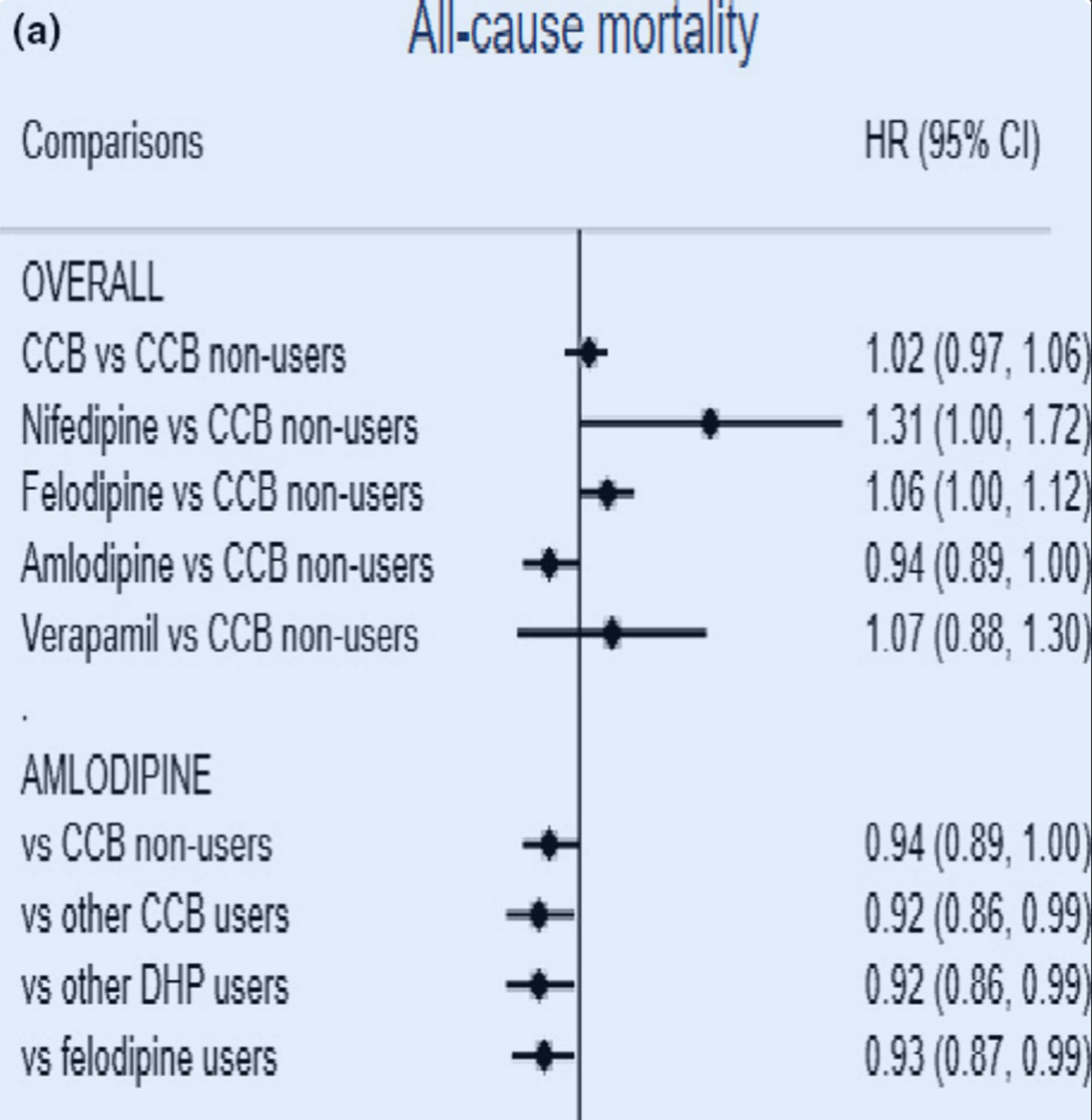
And in this paper, amlodipine reduced ACM more than felodipine and other DHPs (mostly nifedipine and felodipine?): Calcium channel blockers, survival and ischaemic stroke in patients with dementia: a Swedish registry study 2020
The lack of edema with lacidipine and lercanidipine makes them interesting. Lercanidipine apparently “prevents renal damage induced by angiotensin II and demonstrates anti‑inflammatory, antioxidant, and anti‑atherogenic properties through an increasing bioavailability of endothelial nitric oxide.” (Lercanidipine in the Management of Hypertension: An Update 2017) But they’re way less studied (and prescribed) than amlodipine: 14 RCTs ever done for lacidipine (0 ongoing), 13 for lercanidipine (1 ongoing), and… 681 for amlodipine (63 ongoing)!
So, I conclude the same thing as this paper: fourth-generation DHP CCBs lacidipine and lercanidipine look great, but we need more data; in the meantime, amlodipine is still the king: Newer Calcium Channel Blockers 2022
There is plenty of clinical evidence supporting the advantages of newer L-/T- and L-/N-type CCBs over conventional L-type CCBs. However, this evidence may be biased in many ways due to the small sample size, short follow-up and open-label design of several studies. Due to the lack of large and long-term studies, data on cardiovascular outcomes and mortality is scarce for most of the newer agents. Conversely, amlodipine has been studied in several large, long-term trials, such as the antihypertensive lipid-lowering treatment to prevent heart attack trial that enrolled >33,000 patients and had a follow-up of about 5 years. In addition, the safety and efficacy of amlodipine for enhancing patient outcomes are firmly established. Despite the limitations of current clinical evidence, the novel CCBs herald a new era in antihypertensive therapy. More well-designed, large-scale and long-term clinical trials involving these agents are needed to aid clinicians in making a more informed decision about the most appropriate CCB for their patients.
What do you think @DrFraser?
I’m still in a holding pattern with my first drug for most people being telmisartan, then adding amlodipine low-moderate dose then indapamide as my first 3 drugs in progression for most patients.
I try to stay away from the Non-DHP agents due to having more interactions and potentially contributing to symptomatic bradycardia in older individuals. They also limit my ability, if needed to add a beta blocker.
Each case is different - but thinking that each drug one prescribes should have a dual benefit of longevity independent of the condition being treated is a new concept for most patients. If I’m going to Rx an ACE-I or ARB for Hypertension - it makes sense to Rx the one that decreases rate of death and neurocognitive decline - and actually push the dose up to 80 mg … rather than only going low-moderate dose with other agents. However, the table is fascinating above on pushing the dose up on the CCBs with risk of PD. So treating a patient with PD or high risk of developing - if they have enough blood pressure, considering these agents for dual use may be the smart move.
Thanks for the excellent groundwork here @adssx
Tried Lexapro/Escitalopram at various doses. That only made me hungrier, more lethargic, unmotivated and without any libido. Once I went off it, all of those side effects disappeared within days.
Unfortunately, given the HRs in the chart, I’m not even sure the non-amlodipine DHP CCBs do much better than amlodipine for PD. Also, it’s a 2014 paper; since then, other people could have reproduced it. The neuroprotective effect of DHP CCBs for PD has been reproduced in several papers since then, but not the superiority of lercanidipine, felodipine, and co, if I’m correct.
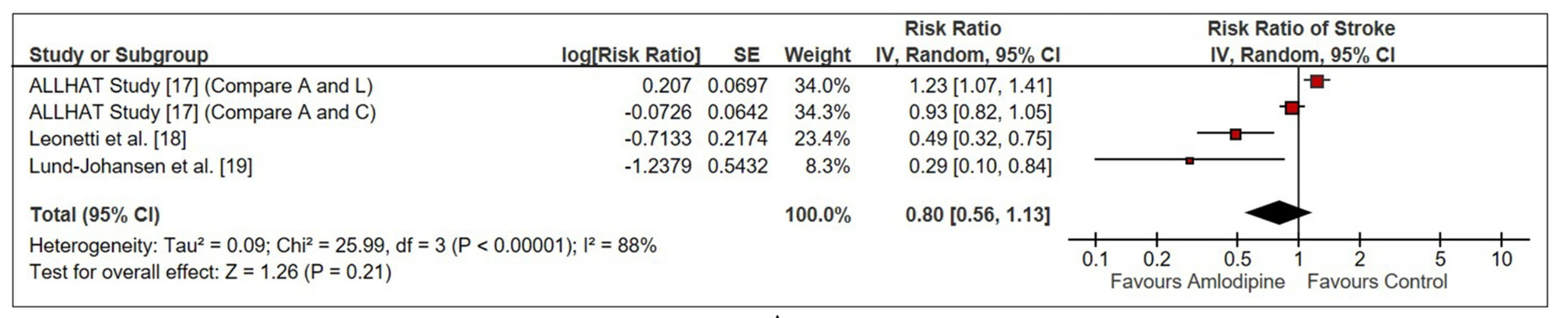
In any case, amlodipine seems the best for CVD. Here’s another paper for stroke, for instance:
- ALLHAT: amlodipine (A) vs lisinopril (L) or chlorthalidone (C)
- Leonetti: vs lercanidipine or lacidipine
- Lund-Johansen: vs lercanidipine
How about Nebivolol as the first addition to Telmisartan? A drop in resting heart rate would seem to be a priority for most.
Nebivolol doesn’t look great @LVareilles:
- Rilmenidine vs Telmisartan or other BP meds for Longevity - #63 by adssx
- Rilmenidine vs Telmisartan or other BP meds for Longevity - #65 by adssx
Amlodipine and indapamide SR look way better for BP lowering, BP variability lowering, and long-term outcomes (CVD, dementia, Parkinson’s, etc.). It’s not even sure that nebivolol is significantly better than other beta-blockers (see the above two links).
It’s unfortunate that blood pressure medication can’t only target systolic (to my knowledge). Most people don’t want to lower their diastolic since it could get too low. I know I’m one of these people who has to watch out for low diastolic.