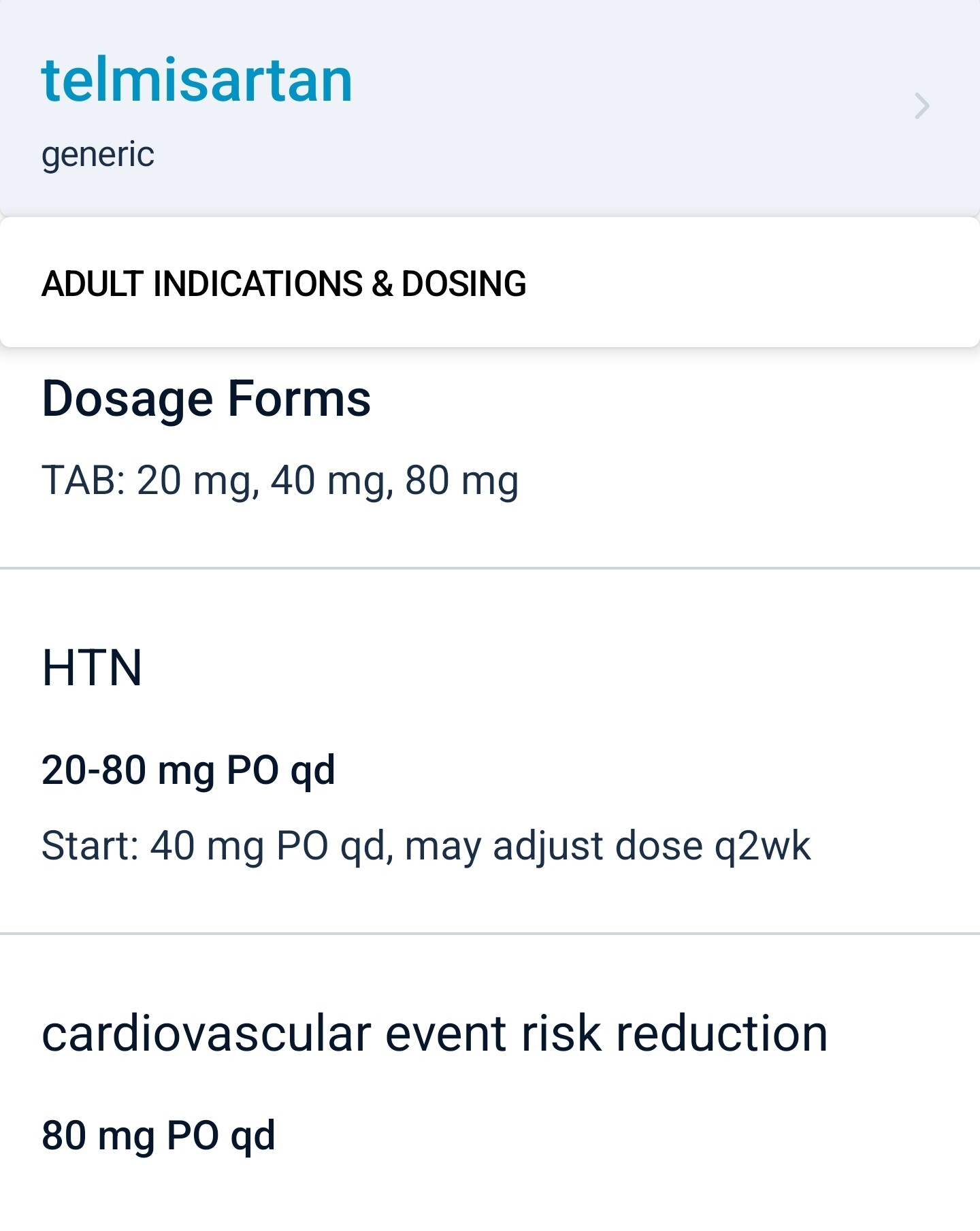
It’s in the clinical medicine app I use called epocrates. The free web version is at epocrates.com
“Telmisartan is, therefore, the only ARB with a broad indication for CV risk reduction in patients with atherothrombotic disease or diabetes with end-organ damage.”
I am a fan of Telemsartan, I was previously using Losartin, but I switched.
“Telmisartan has a number of pharmacological properties that distinguish it from other angiotensin II receptor blockers (ARBs) - the longest plasma half-life, highest lipophilicity and strongest receptor binding affinity in class”
“With publication of the ONTARGET
data, telmisartan is alone among the ARBs in providing CV risk reduction in a broad range of patients typically treated in primary care. So far, no other ARB has achieved this indication.
Therefore, telmisartan is likely to remain at the forefront of CV risk management strategies in the future.”
Link to the full article:
https://sci-hub.se/10.1586/ecp.10.141
Maybe if you are taking omega 3, you can take it alongside your 40mg Telmisartan tablet to enhance its ppar gamma effects ?
https://www.cell.com/cell-metabolism/pdf/S1550-4131(20)30237-0.pdf
Thanks a lot. Telmisartan is really a no brainer as the first-line anti hypertensive.
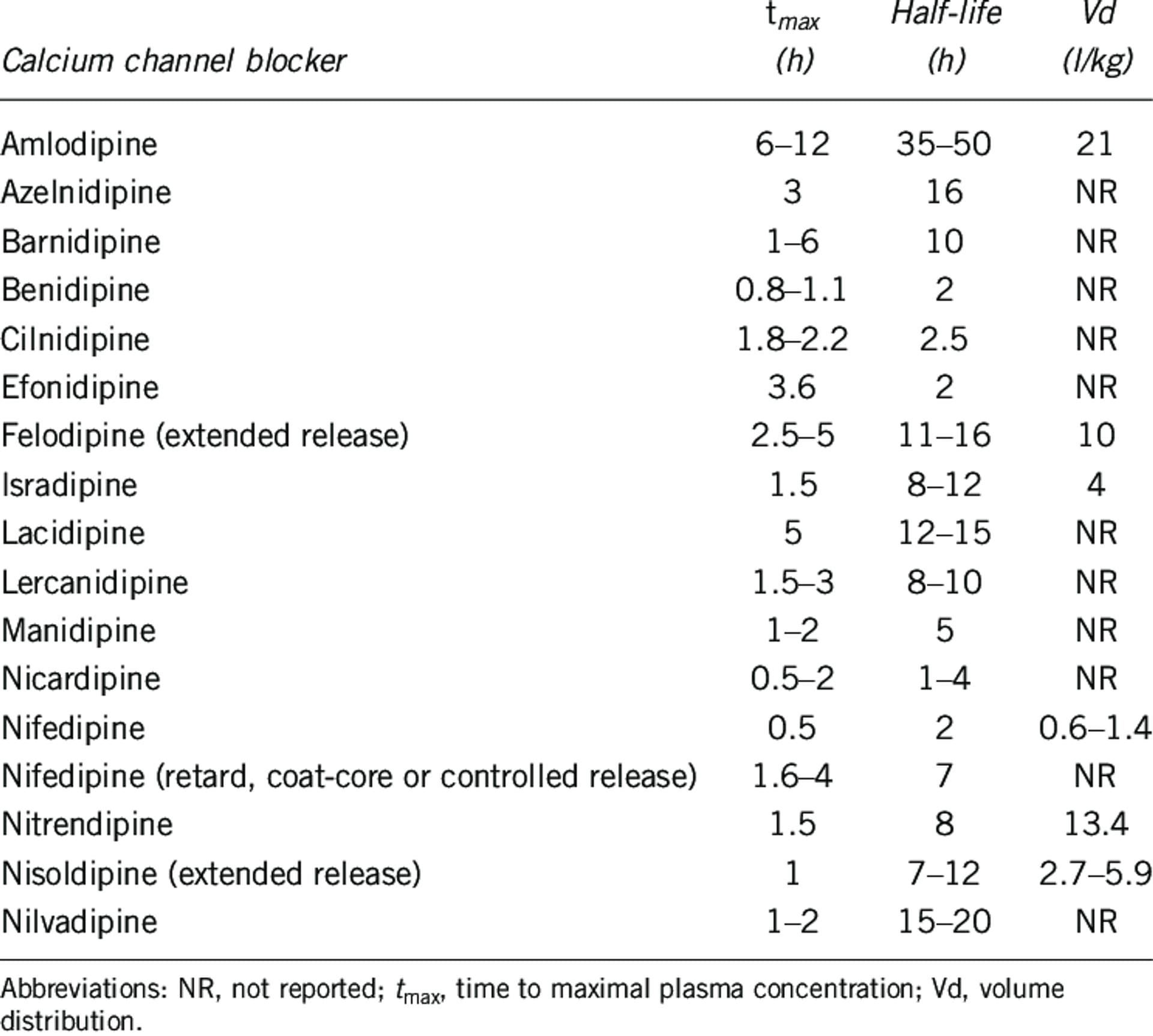
For the second line, amlodipine seems the way to go (long half life [40h] + dihydropyridine + reduced edema risk when combined with telmisartan) but the Ora Biomedical results suggest that two other dihydropyridine CCBs might be even better for longevity: benidipine (half life 2h) and azelnidipine (16h). We need more data in humans but azelnidipine seems interesting:
- Same BP lowering effect as amlodipine but without causing tachycardia: Efficacy and Safety of Azelnidipine as an Antihypertensive Compared to Amlodipine: A Systematic Review and Meta-analysis | High Blood Pressure & Cardiovascular Prevention
- Some neuroprotective properties? Azelnidipine Attenuates the Oxidative and NFκB Pathways in Amyloid-β-Stimulated Cerebral Endothelial Cells - PMC
See also: Benidipine calcium channel blocker promotes the death of cigarette smoke-induced senescent cells and improves lung emphysema 2023
Aside from the well-known senolytic, ABT-263, we identified other potentially new senescence-eliminating compounds, including a new class of molecules, the dihydropyridine family of calcium voltage-gated channel (CaV) blockers. Among these blockers, Benidipine, decreased senescent lung cells and ameliorates lung emphysema in a mouse model. The dihydropyridine family of CaV blockers thus constitutes a new class of senolytics that could improve lung diseases. Hence, our work paves the way for further studies on the senolytic activity of CaV blockers in different senescence contexts and age-related diseases.
Strikingly, 4 different molecules targeting voltage-gated calcium channels (CaV), namely Benidipine, Cilnidipine, Felodipine and Lacidipine, displayed potential senolytic activities on CS-induced senescent cells. To confirm this senolytic activity, we assessed Benidipine, or Cilnidipine, on control and CS-induced senescent cells and observed a clear specific decrease cell number and density of senescent cells without impacting the non-senescent cells (Figure 1C, ,1D1D and Supplementary Figure 2A, 2B). This decreased cell number correlated with senescent cell death as assessed by the quantity of blue trypan positive cells (Figure 1E).
The half-life of felodipine and lacidipine is OK:
Interestingly, lacidipine does not cause edema: Comparative peripheral edema for dihydropyridines calcium channel blockers treatment: A systematic review and network meta-analysis 2022
Nifedipine ranked highest in inducing peripheral edema (SUCRA 81.8%) and lacidipine (SUCRA 12.8%) ranked the least. All DHPCCBs except lacidipine resulted in higher relative risk (RR) of peripheral edema compared with placebo. Nifedipine plus angiotensin receptor blocker (SUCRA: 92.3%) did not mitigate peripheral edema and amlodipine plus angiotensin-converting enzyme inhibitors (SUCRA: 16%) reduced peripheral edema the most. Nifedipine ranked the highest and lacidipine ranked the lowest amongst DHPCCBs for developing peripheral edema when used for cardiovascular indications. The second or higher generation of DHPCCBs combination with ACEIs or ARBs or diuretics lowered the chance of peripheral edema development compared to single DHPCCB treatment.
Lacidipine and lercanidipine might be good alternatives to amlodipine in patients who develop edema, but otherwise, I feel like there’s not enough data to recommend them instead of amlodipine first.
Then, for the third-line treatment, my bet is on indapamide SR, but we don’t have much data…
I dug further into CCBs. It’s complex as there are different generations, dihydropyridine (DHP) vs. non-DHP, L-type, T-type, N-type (and their combinations), BBB-crossing or not, centrally vs. peripherally, lipophilic or not, etc.
Amlodipine is a peripheral-acting third-generation L-type DHP CCB that does not cross the BBB easily.
Some papers suggest that DHP CCBs that cross the BBB easily (e.g. felodipine, isradipine, lacidipine, lercanidipine, nicardipine, nifedipine, nimodipine, nisoldipine, and nitrendipine) are better:
In people with no prior history of psychiatric or neurodegenerative disorder, there was a significantly lower incidence of most disorders with BP-CCBs compared to amlodipine, with risk ratios ranging from 0.64 to 0.88 and an overall risk ratio of 0.88, i.e. a risk reduction of 12%.
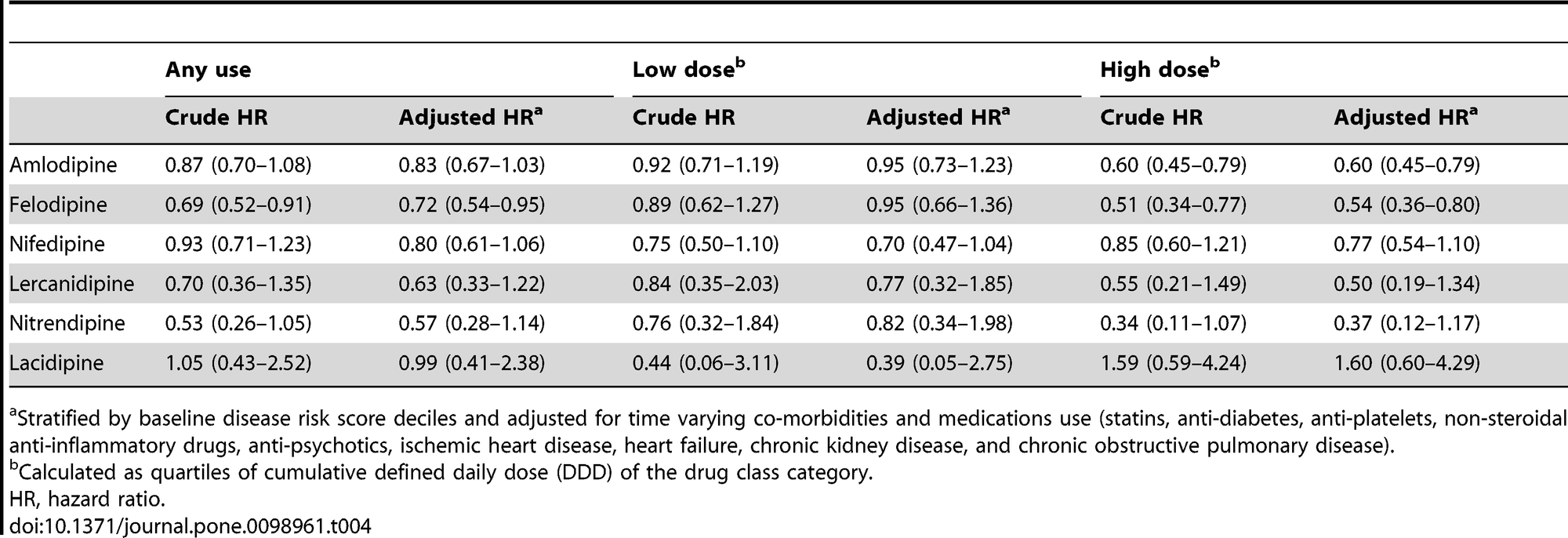
Antihypertensive Agents and Risk of Parkinson’s Disease: A Nationwide Cohort Study 2014
Due to the differences in lipophilic properties, we further distinguished CCBs into the central-acting ones that could cross the blood-brain barrier (felodipine, nifedipine, lercanidipine, nitrendipine and lacidipine) and the peripheral-acting ones that are thought to not cross blood-brain barrier as readily (amlodipine, verapamil, and diltiazem). We found any use of central-acting CCBs, rather than peripheral-acting ones, was associated with a decreased risk of PD (adjusted HR, 0.69; 95% CI, 0.55–0.87, table S4). Among the individual dihydropyridine CCB, the use of felodipine was found to have a reduced association with PD, with a potential dose-response relationship (HR, 0.72; 95% CI, 0.54–0.95 for any use; HR, 0.54; 95% CI, 0.36–0.80 for higher cumulative use). There was also a decreased association between higher cumulative use of amlodipine and risk of PD.
Non-amlodipine CCBs don’t do as well as amlodipine for PD prevention in the above paper, but they’re also used way less often, which might explain the wider CIs.
Felodipine seems interesting: Neuro-modulatory impact of felodipine against experimentally-induced Parkinson’s disease: Possible contribution of PINK1-Parkin mitophagy pathway 2024
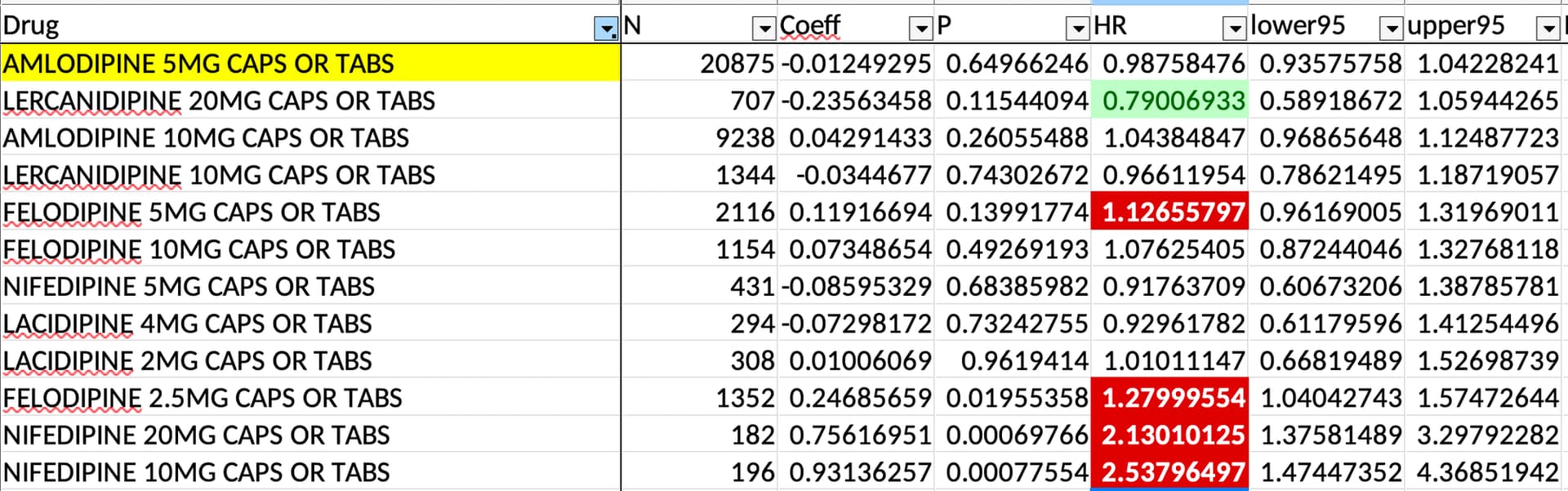
But in the EPITERNA study, only lercanidipine 20 mg might do a bit better than amlodipine 5 mg and felodipine didn’t look especially good:
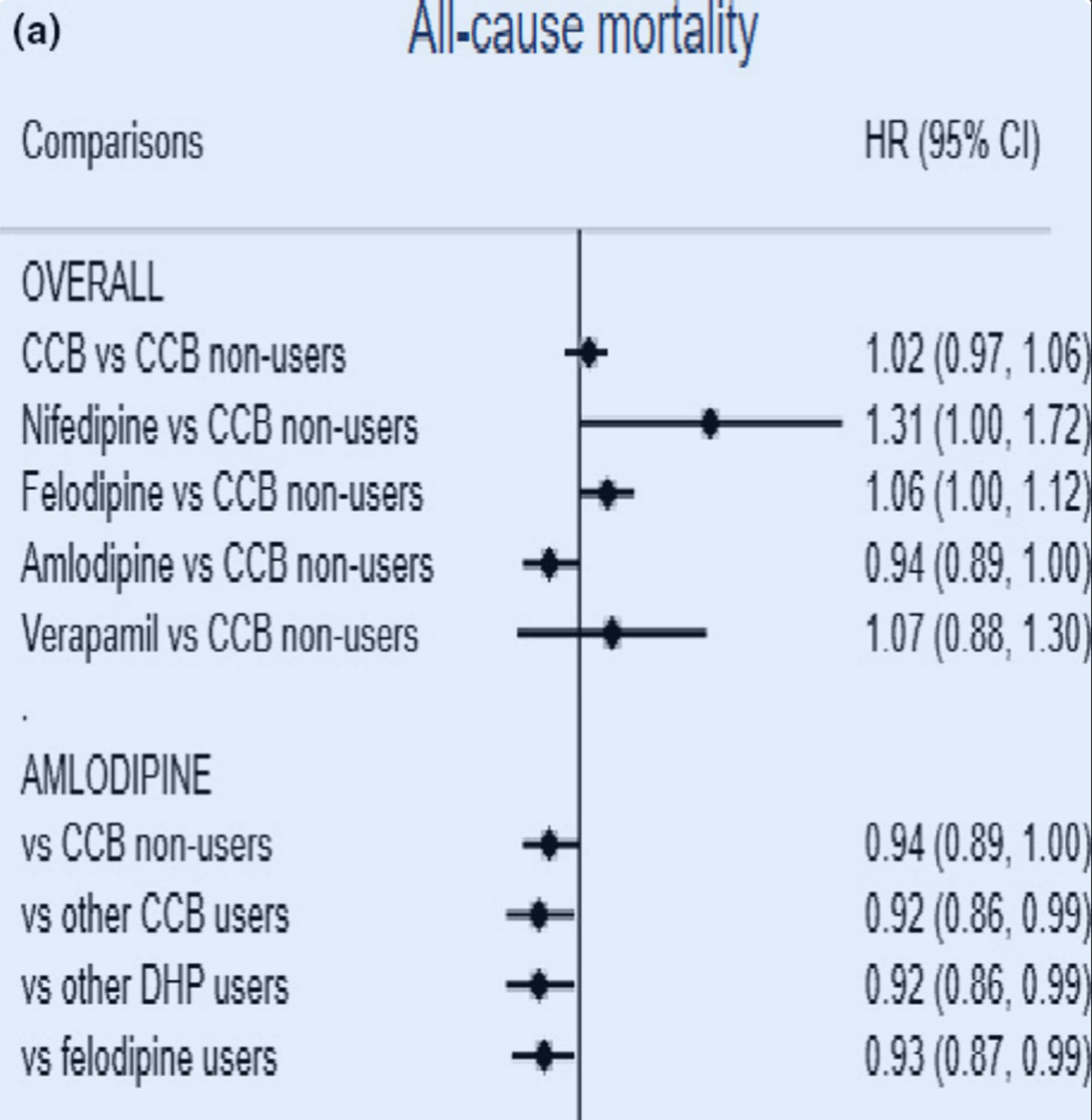
And in this paper, amlodipine reduced ACM more than felodipine and other DHPs (mostly nifedipine and felodipine?): Calcium channel blockers, survival and ischaemic stroke in patients with dementia: a Swedish registry study 2020
The lack of edema with lacidipine and lercanidipine makes them interesting. Lercanidipine apparently “prevents renal damage induced by angiotensin II and demonstrates anti‑inflammatory, antioxidant, and anti‑atherogenic properties through an increasing bioavailability of endothelial nitric oxide.” (Lercanidipine in the Management of Hypertension: An Update 2017) But they’re way less studied (and prescribed) than amlodipine: 14 RCTs ever done for lacidipine (0 ongoing), 13 for lercanidipine (1 ongoing), and… 681 for amlodipine (63 ongoing)!
So, I conclude the same thing as this paper: fourth-generation DHP CCBs lacidipine and lercanidipine look great, but we need more data; in the meantime, amlodipine is still the king: Newer Calcium Channel Blockers 2022
There is plenty of clinical evidence supporting the advantages of newer L-/T- and L-/N-type CCBs over conventional L-type CCBs. However, this evidence may be biased in many ways due to the small sample size, short follow-up and open-label design of several studies. Due to the lack of large and long-term studies, data on cardiovascular outcomes and mortality is scarce for most of the newer agents. Conversely, amlodipine has been studied in several large, long-term trials, such as the antihypertensive lipid-lowering treatment to prevent heart attack trial that enrolled >33,000 patients and had a follow-up of about 5 years. In addition, the safety and efficacy of amlodipine for enhancing patient outcomes are firmly established. Despite the limitations of current clinical evidence, the novel CCBs herald a new era in antihypertensive therapy. More well-designed, large-scale and long-term clinical trials involving these agents are needed to aid clinicians in making a more informed decision about the most appropriate CCB for their patients.
What do you think @DrFraser?
I’m still in a holding pattern with my first drug for most people being telmisartan, then adding amlodipine low-moderate dose then indapamide as my first 3 drugs in progression for most patients.
I try to stay away from the Non-DHP agents due to having more interactions and potentially contributing to symptomatic bradycardia in older individuals. They also limit my ability, if needed to add a beta blocker.
Each case is different - but thinking that each drug one prescribes should have a dual benefit of longevity independent of the condition being treated is a new concept for most patients. If I’m going to Rx an ACE-I or ARB for Hypertension - it makes sense to Rx the one that decreases rate of death and neurocognitive decline - and actually push the dose up to 80 mg … rather than only going low-moderate dose with other agents. However, the table is fascinating above on pushing the dose up on the CCBs with risk of PD. So treating a patient with PD or high risk of developing - if they have enough blood pressure, considering these agents for dual use may be the smart move.
Thanks for the excellent groundwork here @adssx
Tried Lexapro/Escitalopram at various doses. That only made me hungrier, more lethargic, unmotivated and without any libido. Once I went off it, all of those side effects disappeared within days.
Unfortunately, given the HRs in the chart, I’m not even sure the non-amlodipine DHP CCBs do much better than amlodipine for PD. Also, it’s a 2014 paper; since then, other people could have reproduced it. The neuroprotective effect of DHP CCBs for PD has been reproduced in several papers since then, but not the superiority of lercanidipine, felodipine, and co, if I’m correct.
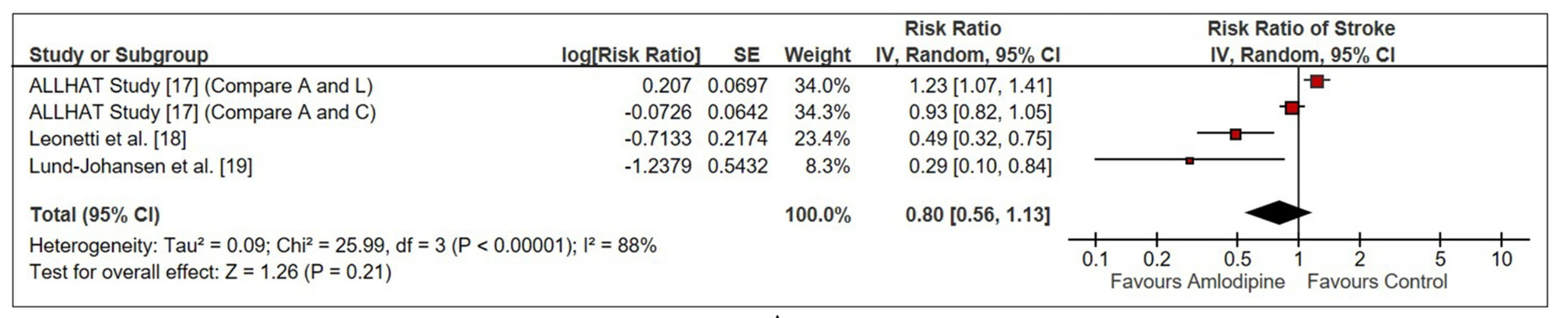
In any case, amlodipine seems the best for CVD. Here’s another paper for stroke, for instance:
- ALLHAT: amlodipine (A) vs lisinopril (L) or chlorthalidone (C)
- Leonetti: vs lercanidipine or lacidipine
- Lund-Johansen: vs lercanidipine
How about Nebivolol as the first addition to Telmisartan? A drop in resting heart rate would seem to be a priority for most.
Nebivolol doesn’t look great @LVareilles:
- Rilmenidine vs Telmisartan or other BP meds for Longevity - #63 by adssx
- Rilmenidine vs Telmisartan or other BP meds for Longevity - #65 by adssx
Amlodipine and indapamide SR look way better for BP lowering, BP variability lowering, and long-term outcomes (CVD, dementia, Parkinson’s, etc.). It’s not even sure that nebivolol is significantly better than other beta-blockers (see the above two links).
It’s unfortunate that blood pressure medication can’t only target systolic (to my knowledge). Most people don’t want to lower their diastolic since it could get too low. I know I’m one of these people who has to watch out for low diastolic.
Yes, isolated systolic hypertension (ISH) can be harder to treat: Unsolved Problem: (Isolated) Systolic Hypertension with Diastolic Blood Pressure below the Safety Margin 2020
The general recommendations for (I)SH treatment mostly agree in various international and national guidelines. They differ in terms of a class of recommendations and level of evidence, but most guidelines recommend thiazide(-like) diuretics and dihydropyridine calcium-channel blockers (CCBs). The Korean Society also recommends angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers as first-line drugs for (I)SH. Experts in Canada do not recommend α-/β-blockers as the first choice of antihypertensive drug for (I)SH unless there is a compelling indication. The authors of The National Institute for Health and Care Excellence (NICE) guidelines from Great Britain recommend the same therapy as for other patients with HTN.
The 2023 European guidelines say:
Based on the data in aggregate, CCBs and Thiazide-like diuretics emerged as the drugs of choice for the management of ISH, whereas ACEis/ARBs showed less efficacy, suggesting that they should be used as first-line agents when there are compelling indications such as HF, coronary artery disease, CKD, metabolic syndrome and diabetes.
See also: Isolated Systolic Hypertension: An Update After SPRINT 2016
Drugs to Avoid: Beta-Blockers
Evidence has shown that beta-blockers have little, if any, efficacy in management of hypertension.As noted in the isolated systolic hypertension substudy of the Losartan Intervention For Endpoint reduction (LIFE-ISH) trial, atenolol was inferior to losartan for cardiovascular risk reduction.In the second Swedish Trial in Old patients with Hypertension (STOP-2) trial subgroup, the combination of diuretics and beta-blockers had the highest events for stroke, compared with ACEi and CCBs.
It’s hard to get good data on how much each antihypertensive reduces SBP and DBP as it depends on the dose but also on the individual (men and women might respond differently, there might be differences between ethnic groups as well). For thiazide-like diuretics, this paper claims that indapamide 1.5 mg SR is better than amlodipine and candesartan: Indapamide SR Versus Candesartan and Amlodipine in Hypertension: The X-CELLENT Study 2006
For the patients with isolated systolic hypertension (n = 388), the three treatments significantly reduced systolic BP, but only indapamide SR did not change diastolic BP and thus reduced pulse pressure significantly relative to placebo (P = .005). […] In patients with isolated systolic hypertension (n = 106), indapamide SR reduced 24-h systolic BP significantly more than amlodipine (P = .037), and only indapamide SR reduced 24-h pulse pressure significantly relative to placebo (P = .03).
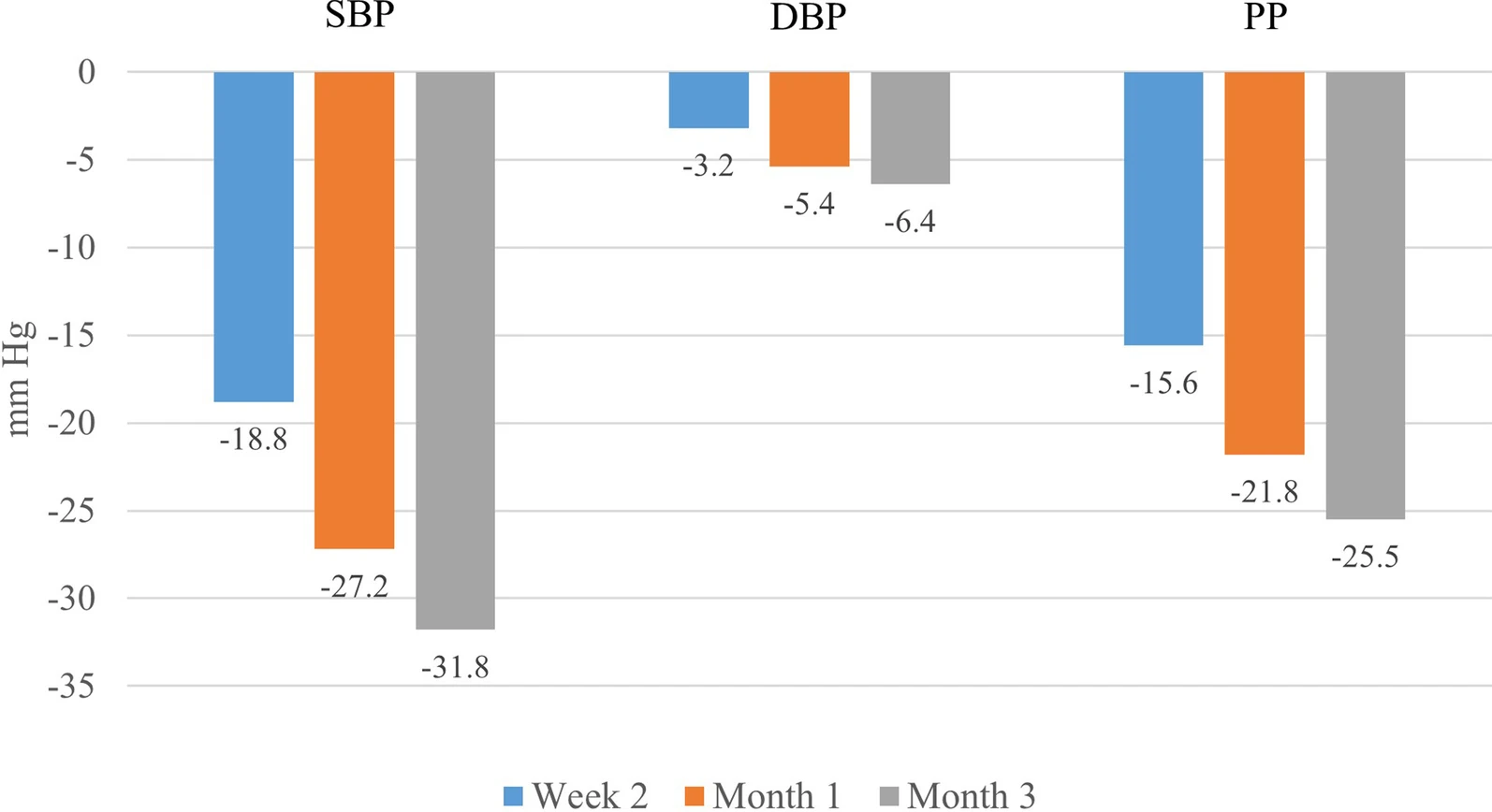
If you need even more BP lowering, another study looked at indapamide 1.5 mg SR (the sustained release version seems better than the normal indapamide 2.5 mg) + amlodipine (5 mg or 10 mg) and you can see that this combo is clearly the best at massively lowering SBP while keeping DBP in range: Effectiveness of indapamide/amlodipine single-pill combination in patients with isolated systolic hypertension: post-hoc analysis of the ARBALET study 2022
At study entry, 68.5% were prescribed indapamide/amlodipine SPC at a dose of 1.5/5 mg and 31.5% were prescribed a dose of 1.5/10 mg.
At 3 months, 60.7% of patients were receiving a dose of 1.5/5 mg, and 39.3% were receiving 1.5/10 mg
Unfortunately, they don’t give the results by dose, but I assume that 1.5/5 mg reduced DBP less than 1.5/10 mg and if that’s still too much you can use 2.5 mg amlodipine instead.
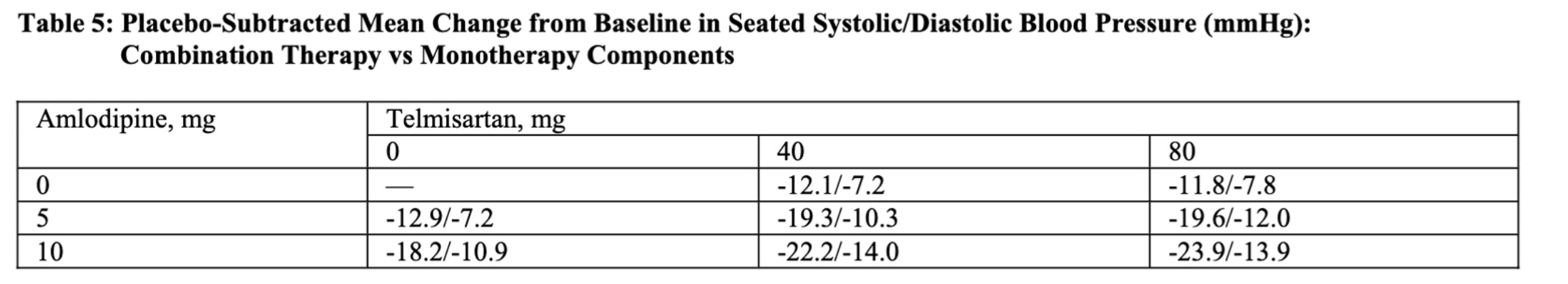
On a personal note, I’m actually considering adding indapamide 1.5 mg SR. Telmisartan 40 mg + amlodipine 2.5 mg reduced my BP only by -7/-6 mmHg to reach 127/75 (24h Aktiia), so although I’m not hypertensive anymore per Europe guidelines (<130/80), I’m still a bit higher than the US guidelines (<125/75) and I’m definitely not “optimal” (<115/75). Although it could have other benefits, pushing telmisartan to 80 mg won’t bring more SBP reduction. Increasing amlodipine to 5 mg is another option (FDA):
For most patients - and there are exceptions, beta blockers come later once we’ve not had adequate success with the stepwise progression. I don’t like the blocking of maximal heart rate and potential effects in ability to exert oneself - if an elite athlete. There is a fair bit of controversy in that space.
Overall, seeing more patients get into symptomatic bradycardia with age must also be monitored.
There are situations such as heart failure where there are likely benefits - but for dual use for longevity and hypertension - I think there are probably better choices.
If I look at the NICE recommendations they seem all over the place, has someone showed that telmisartan for example is recommended by medical societies over other treatments? It’s not as clear as is the case for atorvastatin within cholesterol lowering medications.
For me, the case for telmisartan is way clearer and stronger than for atorvastatin.
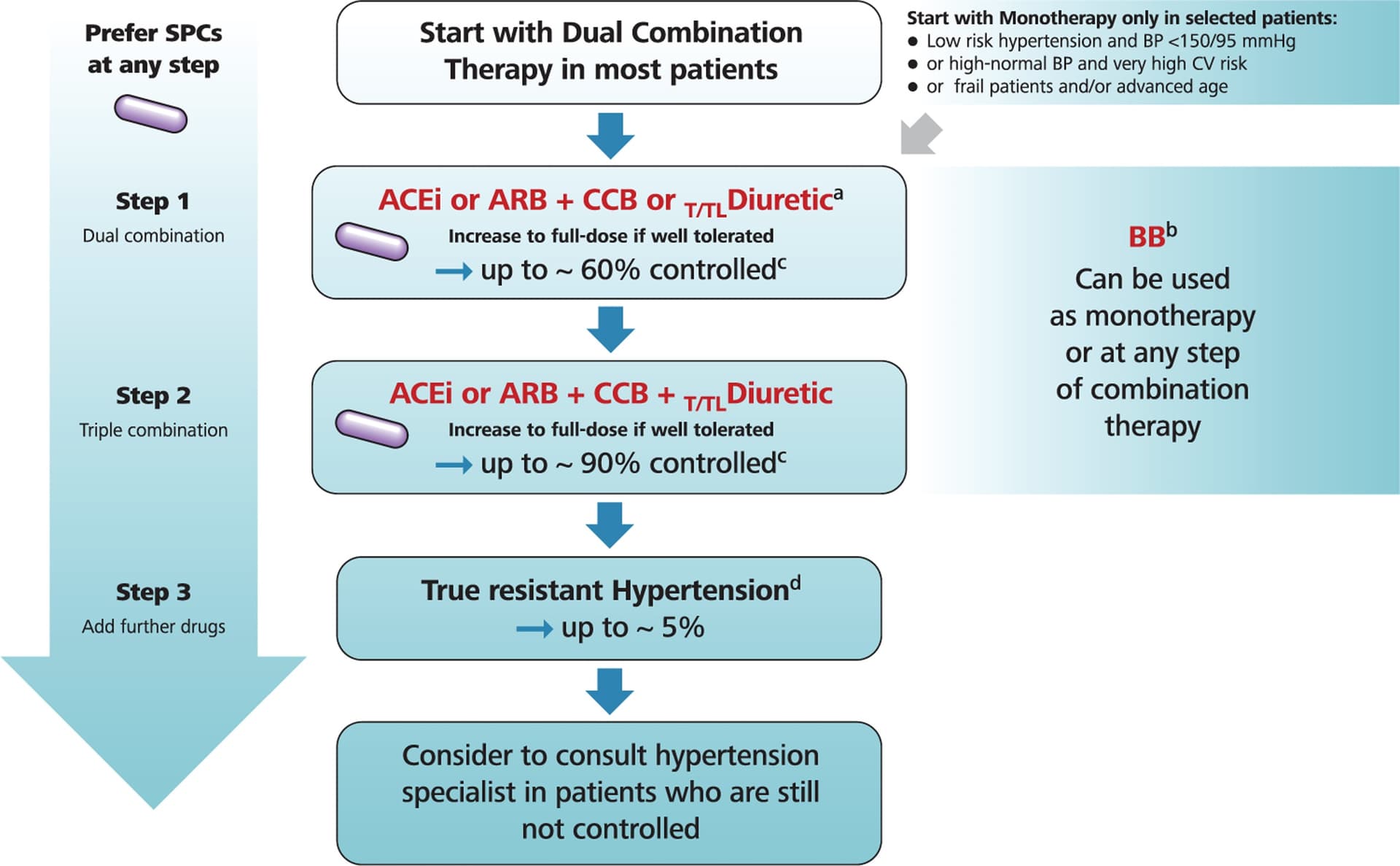
But yeah, the hypertension guidelines really rarely recommend specific drugs and mostly deal with class (although if you read the whole document, they might address some intra-class differences). Here are the latest European guidelines; other countries are almost identical (in terms of overall strategy and choice of classes):
I meant as a drug-specific recommendation for hypertension as atorvastatin is for primary prevention of heart disease. I see so it’s up to us to figure out the best drug within each class.
Exactly. Still, most guidelines (and I think everyone) agree that long-acting agents should be preferred to maintain BP control over a long period of time and decrease BP variability as much as possible. The longest acting ACEi is ramipril, ARB is telmisartan, CCB is amlodipine, and thiazide/thiazide-like is chlorthalidone (or maybe indapamide SR?). For beta blockers I think it’s nadolol. Then for dementia prevention (and potentially longevity?) the best seems to be ARB (over ACEi), DHP CCB (over non DHP CCB), and thiazide (over non thiazide diuretic and beta blockers). Which gives us telmisartan + amlodipine + indapamide SR (chlorthalidone did not outperform HCTZ in a recent trial).
Check potential counter indications (if any, I don’t know) before switching.
Yup, Beta blocker is a rev limiter