cognitive improvements after only 8 weeks! is impressive.
Does anyone have a link to the full paper, please? Interested to know the magnitude of impact.
cognitive improvements after only 8 weeks! is impressive.
Does anyone have a link to the full paper, please? Interested to know the magnitude of impact.
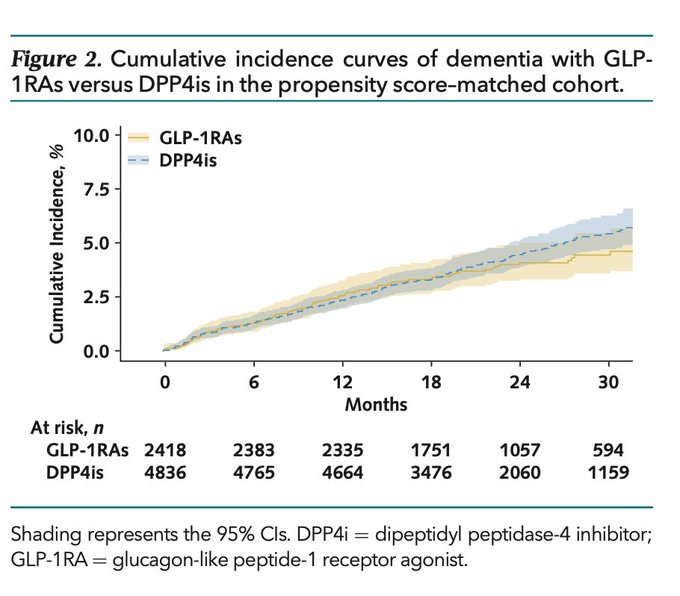
Subgroup analyses showed consistent benefit across age and sex, with the strongest effect among older adults and females.
Hi Steve - I think for both GLP-1’s and SGLT2’s the evidence is growing that these are neuroprotective.
Could anyone link the best papers on SGLT2Is being neuroprotective?
There are dozens of them. Search for dementia, Alzheimer’s, or Parkinson’s in the canagliflozin thread (or on Google Scholar): Canagliflozin - Another Top Longevity Drug
I completely agree. The further question I have though is whether they are independently protective beyond the weight loss/blood glucose etc affect. I suspect there will be lots of factors - weight loss will lead to greater activity levels, less painkiller use. And they may also lead to better average quality of food intake. And there’s all the other downstream affects of GLP-1s like reduction in alcohol, gambling etc
I suspect, after all of those benefits, there may not be a direct pharmacological neuroprotective affect - but I’d love to be wrong.
Well as much as we all hate pasted AI - this is from Vera Health and it documents it reasonably well … so at the risk of scorn … I paste.
Yes, the longevity and neuroprotective effects of GLP-1 agonists and SGLT2 inhibitors are at least partially independent of their glucose-lowering and weight-reducing effects:
Conclusion:
The evidence strongly supports that GLP-1 agonists and SGLT2 inhibitors have longevity and neuroprotective effects that are at least partially independent of their glucose-lowering and weight-reducing actions. This is demonstrated by consistent cardiovascular and renal benefits across different risk profiles, significant reductions in dementia risk, and mechanistic studies showing direct effects on cellular health. However, the degree of independence varies, and more research is needed to fully isolate these effects from metabolic improvements.
Hello Dr. Fraser,
Do you always use regular doses of GLP-1 RA or in some cases micro- doses?
I use standard dosing, most commonly tirzepatide to the degree of tolerability and not causing weight loss to an unacceptable level. There are many patients who are at or near ideal body weight - in those, I’d favor a low dose SGLT2-i as this can usually be tolerated with little change in body weight. For the majority, who have a bit of weight to lose we go with standard doses, with goal of 0.5-1 lbs/week wt loss (no faster) until at IBW, then back off a bit, and usually if financially able an no contraindications, add an SGLT2-i … for individuals at some risk of neurocognitive decline, cardiovascular, metabolic or renal disease … which is most people.
I propose that with most drugs, the benefit looks a bit like how it works with statins (but there we can easily measure the effect) in that a majority of the benefit occurs at lower doses, and pushing higher gets a tiny bit more benefit, but more toxicity.
The microdosing approach makes little sense to me - it is like homeopathy - a minuscule dose is going to have therapeutic effects? Results are dose dependent, as is toxicity. I’d at least like to see a modest dose in order to think it is doing anything. I however don’t have definitive proof of this belief in this context, but it makes the most sense pharmacologically … and I’ll stick with this until proven otherwise.
I’m going to give the 5 year fermented Dr Ohhira’s probiotics a go to see if it helps me recover from recent antibiotic usage. Amoxicillin gave me some gut pain.
Hi… Here is a link to my article titled Postbiotic Metabolites: The New Frontier in Microbiome Science which explains why Dr. Ohhira’s Probiotics is the best product in the world to help reset a healthy gut microbiome. Each dose of Dr. Ohhira’s Probiotics contains over 500 POSTBIOTIC METABOLITES. If you want additional info…send a request to me at: rosspelton70@gmail.com
Thanks I’ll give it a read. I’m excited to try the product. The 60 capsule version of the 5 year fermented product is on sale on iHerb at the moment, it’s cheaper to buy 2 of those than 1x of the 120 pack.
Hi…not sure which will give you best price…usually the #120 count is less expensive than purchasing two of the #60 boxe.
There is a special on the 60 pack. Works out cheaper for the time being. Worth checking out!
Thanks for letting me know.
Hello Dr. Frazer, I understand that many patients on GLP-1agonists develop constipation, especially with a predisposing tendency to the problem. Patients who take SGLT2 inhibitors are prone to worsening of urinary frequency and UTIs. Both problems are common in elderly population. How do you deal with these problems?
I even developed constipation on Pendulum GLP-1 Probiotic.
Thank you!
Good question - this is a multipronged approach and everything is dose dependent.
So for GLP-1’s, first, with a primary plant based whole food diet (feel free to add a little fish, fermented dairy and if desired other little bits of meat) will be a high fiber diet with lots of bulk. Individuals pursuing this get multiple health benefits, but also tend to tolerate GLP-1’s. I recall possible ~2% of my patients having an issue with this - and those individuals have gone down on dose, or switched GLP and have tolerated it to the benefit of their metabolic health.
The SGLT2’s tend to have a long half life - but still, taking them in the AM is smart. I’ve not noted a big issue with urinary frequency for most, but the UTI issue is a real one - and some individuals who get them repetitively, just shouldn’t have these agents. Naturally, the moment you think you have a UTI, cease this medicine until it is treated and better as the bacteria have a feast on all the glucose coming into the urine. I’ve got a handful of people with this issue, and the SGLT2-i’s just aren’t a match for them.
I don’t think Pendulum is comparable to an injectable GLP-1 … I appreciate their view that it might have some action in this space - I’ve not found it to be clinically meaningful.
Have you seen this?
also: