Diabetes mellitus is a well-recognized risk factor for dementia. In prospective studies, diabetes confers a greater than 80% increase in risk for all-cause dementia and Alzheimer’s disease, and greater than 180% increase in risk for vascular dementia.1 One in seven adults in the United States are estimated to have diabetes, and more than 90% of them have type 2 diabetes (T2D).2 With an aging population and increasing obesity, the incidence and prevalence of T2D is expected to continue to increase worldwide.3
Insulin resistance, which is a metabolic hallmark of T2D, has been postulated as a pathophysiologic connection between diabetes and dementia. Hyperinsulinemia, a biomarker of peripheral insulin resistance, is a risk factor for Alzheimer’s disease even in the absence of diabetes.4 At the same time, ex-vivo studies have shown evidence of brain insulin resistance in people with Alzheimer’s disease who did not have diabetes.5 While insulin signaling in the brain has an important role in neuronal and glial metabolism, synaptic neurotransmission, neuroinflammation and neurovascular coupling, it is presently unclear whether the observed associations between T2D and dementia are caused by insulin resistance in the brain or metabolic consequences of peripheral insulin resistance (as reviewed in Reference 6). T2D is also characterized by endothelial dysfunction and microvascular insufficiency, which can lead to vascular dementia even in the absence of macrovascular insults, through mechanisms involving ischemia, blood–brain barrier leakage, and disruptions in white matter integrity.7
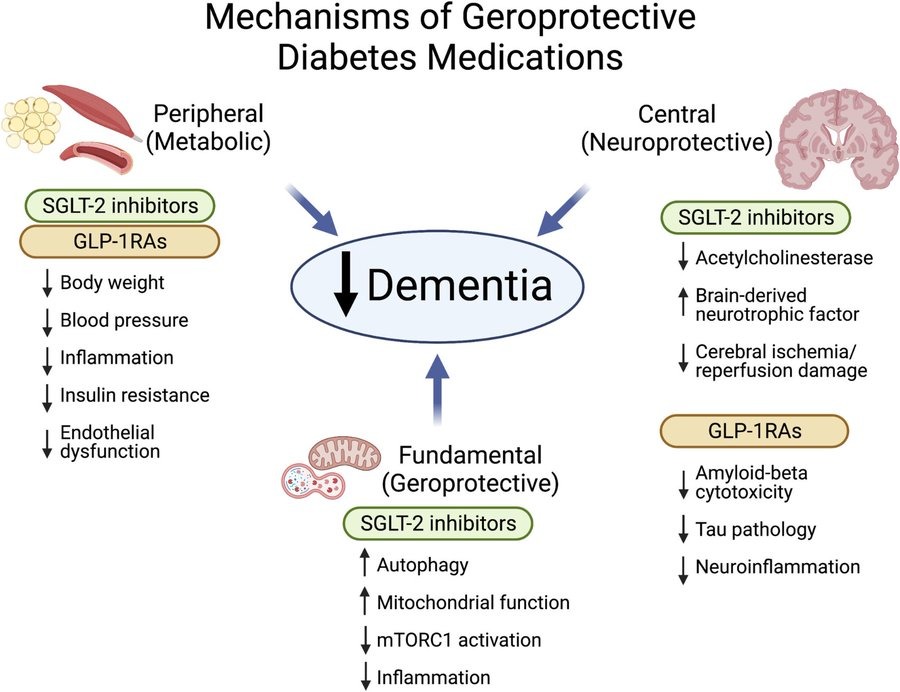
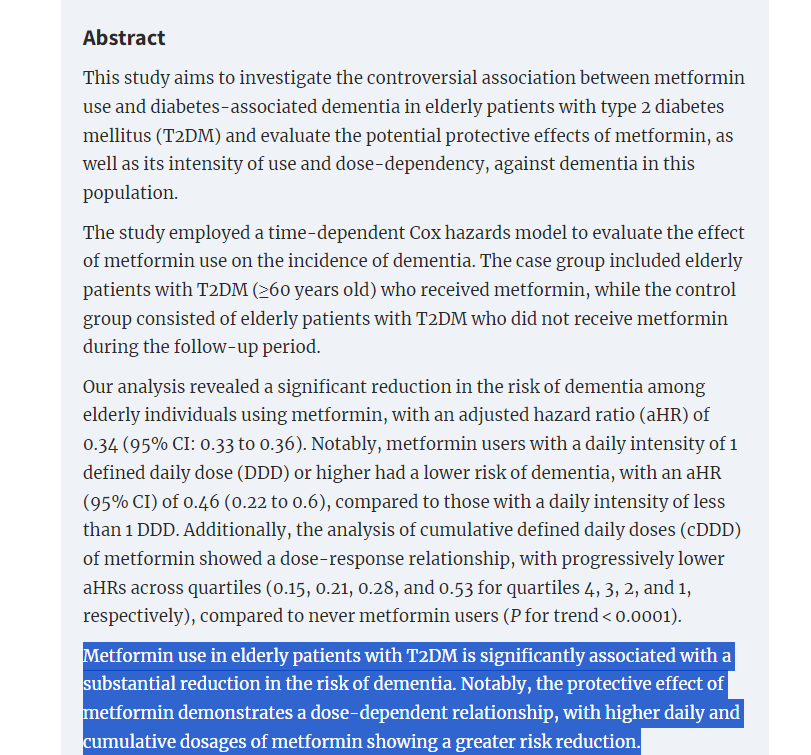
Given the strong epidemiologic and pathophysiologic connections between diabetes and dementia, it is not surprising that glucose-lowering drugs have been of interest for the prevention of dementia. In the current issue of the Journal of the American Geriatrics Society, Tang and co-authors8 aimed to resolve inconsistencies in the existing observational data by performing a systematic review and a meta-analysis to examine the associations between the use of dipeptidyl peptidase-4 (DPP-4) inhibitors, glucagon-like peptide 1 receptor agonists (GLP-1RAs) and sodium-glucose co-transporter 2 (SGLT2) inhibitors in people with T2D and the risk for incident all-cause dementia, Alzheimer’s disease and vascular dementia. Ten observational prospective studies that met the inclusion criteria for meta-analysis encompassed more than 800,000 people with T2D (44% men), with a mean baseline age of 68 years and a median duration of follow-up of 4.5 years. Included studies were predominantly deemed to be of high methodological quality, but with substantial heterogeneity. Seven studies involved DPP-4 inhibitor users who, compared to non-users, had significantly lower relative risk for all-cause dementia by 17% and vascular dementia by 41%, but without significant difference in the risk for Alzheimer’s disease. Compared to non-users, users of GLP-1RAs (five studies) and SGLT2 inhibitors (three studies) had a significantly lower risk for all-cause dementia by 28% and 38%, respectively; meta-analysis by dementia subtype was not performed due to a limited number of studies.
Full Paper:
https://agsjournals.onlinelibrary.wiley.com/doi/10.1111/jgs.18405