I almost exclusively use olive oil, but technically isn’t an olive a seed?
No it is a fruit. The seed is thrown out.
you can eat what you like.
but i will try to keep my omega6 fats at zero if I can.
Nobody ever proved saturated fat is bad. And it’s lookin’ like it’s FAR more healthy than linoleic acid which breaks down into all kinds of toxins.
Your body makes sat fat and monounsat. It does NOT make omega6. That means it only needs a small amount of it that has always been supplied in our diet (for the 2+ million years we’ve been homo erectus and after).
Now, if you’re a processed food manufacturer, sure you’ll say that. That’s how you make money. You take cheap toxic omega6 fats and you convert them into something meatlike - and profit.
As for me - I’m stayin’ away from as much omega6 as I can (and even omega3 and monounsat - I get enough of those from meat).
All depends on context, if you don’t have context, any purported “data-driven” approach to make some random overarching health claim is meaningless. Pure omega 6 linoleic acid is generally not “inflammatory”…until it isn’t. Anyone without deep knowledge making broad new positive or negative health claims for everyone should be heavily scrutinized. The problem is most people are not realizing acquiring quality nutrition knowledge is more difficult than figuring out astrophysics. It’s one of those subjects that feel deceptively simple, so illusory knowledge is common.
If you have a lot of biochem knowledge as you have previously claimed before Alex, you would probably have understood exactly where to quickly look downstream of linoleic acid metabolism. This isn’t even particularly esoteric, AA/EPA pathways is basic Biochem 101 in college.
Cardiometabolic diseases i.e. insulin resistance, atherosclerosis, and steatohepatitis all share tissue-specific features of chronic unresolved inflammation. The typical view is blood biomarker levels of AA are not associated with higher risk of cardiovascular outcomes for the average person and that’s partly why I mentioned pure linoleic acid in isolation is not “inflammatory” in general - production and breakdown of inflammatory metabolites is highly, highly regulated in the average person who is “healthy”. We also know FADS is a regulator of inflammation resolution can impact cardiometabolic issues in certain contexts.
Some people with asthma may wish to severely limit omega 6 linoleic acid to under 4g/day, according to the Brigham & Women AERD Center.
This is 7% of asthma folks and 14% of those with severe asthma.
https://www.jaci-inpractice.org/article/S2213-2198(17)30794-8/fulltext
It may also be beneficial to severely limit linoleic acid in psoriasis:
If you are a huge biochemistry nerd, you’ll probably quickly realize perhaps those who are “healthy” with FADS variability should also consider limiting intake and test to see if any positive effects can happen compared to baseline.
“With few exceptions, n-6 HUFA are precursors of pro-inflammatory/pro-thrombotic signaling lipids, and n-3 HUFA are generally anti-inflammatory/anti-thrombotic.”
Higher than normal hs-CRP levels with significant linoleic acid intake can be seen here with this genotype:
If you have a persistent higher than normal hs-CRP that is a risk-enhancing factor for atherosclerosis according to the newest 2022 ACC guidelines. So are autoimmune disorders - hence if severely limiting linoleic acid intake clearly helps with inflammation resolution based on well-recognized risk-enhancing factors - you may have a much lower chance of mortality with moderating or limiting “plant oils” and hitting harder on “fatty fish oils”, which is generally recommended as >=2 servings of fatty fish per week based on AHA scientific consensus recommendations, not veganism.
I’d also mention the processing of canola oil can transform some of the natural polyunsaturated fatty acids to trans-fat during the deodorization step of the manufacturing and prolonged commercial deep-fat frying can form oxidation products from polyunsaturated fatty acids which can also be harmful. So when you see “zero trans fat” on canola oil - it’s somewhat misleading. There is in fact trans fat in canola oil, just “below 0.5 g per serving”. One serving is usually one teaspoon. So it can add up to significant amounts of bad “trans fats” if you use a lot of highly processed oils like typical canola oil, rather than let’s say (since the discussion refers to the Mediterranean diet) the fats we see in a typical “true” Mediterranean diet - aka eating fish, avocadoes, raw nuts/seeds, etc with real EVOO (that isn’t highly processed oil) and minimizing highly processed foods. Don’t forget - trans fatty acids may interfere with the desaturation and elongation of omega-3 fatty acids - trans fats should be minimized as much as possible (the exception being trans-palmitoleic acid found in ruminant animals not found in your vegan diet - which may decrease insulin resistance based on several cohort studies cross country)
So relative to fats obtained from a traditional “true” Mediterranean diet, typical canola oil use is a mixed bag and may be relatively “unhealthy” by a marginal amount on average for the average person. Trans fats don’t show up in those calculations that are done in your cited CR discussion.
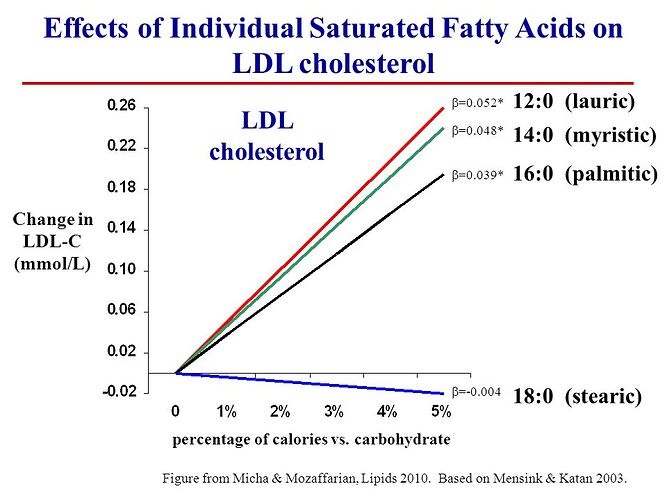
You may say that trans fats are marginal as if you’re only using one teaspoon a day you won’t have significant trans fat intake. But even quite low levels of trans isomers of omega-3 linolenic acid can have adverse effects on LDL and atherosclerosis - so canola oil is probably not that healthy - it may be “healthier” relative to specific saturated fatty acids in general (keep in mind canola oil contains significant amounts of phytosterols as well which boosts the “heart-healthy” part up a bit for the average person - which generally is “good” but can be “bad” in some situations), particularly myristic acid and palmitic acid - so that’s why official guidelines make an overly broad recommendation to replace saturated fats with “heart-healthy” oils such as canola oil - this is heavily dumbed down for the layman aimed at maximizing dietary adherence, not optimization. Note they do not make the recommendation to add gobs of highly processed canola oil in isolation to your diet.
Omega 6 and 3 are essential fatty acids, I wouldn’t avoid either completely. That seems dangerous for health. Here are “adequate intake” recommendations:
It’s likely too much saturated fat is causing millions of deaths each year via its effects on atherogenic lipoprotein concentrations and mass.
It’s proven bad via its effects on LDL and LDL effects on ASCVD (heart attacks).
Seed oils oxidize in the body very quickly. You can track the introduction of seed/vegetable oils into our food system with the onset of heart disease and diabetes. They are poisons.
Read Preston Estep’s Mindspan. He recommends cold-pressed canola oil as the 2nd oil to EVOO. Also mentions that Japanese use canola oil as their primary oil.
Hypoglycemic episodes (especially repeated) are likely harmful to “mindspan”. Yet you seem to ignore this apparently.
As for Estep’s premature claim of higher dietary iron intake having a causative role for a range of neurodegenerative diseases based on pretty much weak and circumstantial evidence that does not establish casuality - an iron chelator recently in larger follow up human trials has failed based on his predictions at least for newly diagnosed Parkinson’s not on levodopa:
https://www.nejm.org/doi/full/10.1056/NEJMoa2209254
In fact, contrary to his predictions, which seem to be partly based on the first small sample size iteration of this trial and a few others, this iron chelator made things worse by accelerating the progression of neurodegenerative disease for these newly diagnosed PD patients and caused harm beyond the typical expected adverse effects, despite decreasing nigrostriatal iron content. Kind of throws a wrench at the hypothesis, but I can’t say it completely rules it out yet.
But one should accept it could be possible that he is just plain wrong and dysregulated iron leading to accumulation is merely an epiphenomenon because all the trials with very modest positive effects as suggestive evidence were pretty tiny in the first place. There really wasn’t much evidence in the first place and at best even if it was true - it would be a modest effect with some tradeoffs.
Have you considered that you’re actually potentially increasing the risk of dementia and accelerating the progression of neurodegenerative disease with some of your claims and interventions?
BTW, I actually take in ~8-9 mg iron personally - even before his claims - and rarely eat red meat in the first place. It’s not because I believe dietary iron has any definitive casual role, as it is quite premature, it’s much more I don’t see any particular reason to take many times the RDA in iron or pretty much almost any other micronutrient either in principle from most fortified foods or any supplement - unless the evidence is particularly compelling.
It also seems you are ignoring high calcium fortification/supplementation common particularly in certain vegan products as well, despite evidence for potentially increased risk. So do you focus at people touting risks particularly regarding meat (which in this case specifically applies to high intakes of red meat) as opposed to risks in veganism?
I’ll also mention a few points regarding Estep and his recommendation on canola oil and a few of his “Mindspan Elite” diet claims.
He claims that it is important to avoid trans fat including not being fooled by <0.5g of trans fat on the label, but touts canola oil. High quality cold pressed canola oil is difficult to find and impractically expensive for most people. You might as well just go with carefully selected true EVOO, so the canola oil recommendation seems largely not particularly applicable for most people.
He also describes a moderate to high intake of fish in the diet of his proclaimed “Mindspan Elite” diet, not veganism. He seems to differentiate meat and fish as inherently different categories (although one can actually selectively breed animals for way more oleic acid and stearic acid as a large majority of the fat content - both of which are LDL-lowering, so there’s a lot more caveats than often assumed to get close to vegetable oils on top of a potential benefit of several specific fatty acids found either only in animals or impractical in plant only, such as CLA), but note he doesn’t recommend specifically eliminating meat, but replacing most “meat” with fish. A bit of a weird category split since it’s not that clear cur, but okay fine I suppose for communication and typical situation purposes that’s acceptable.
He seems to be touting that whole grains and avoidance of refined grains is not the answer and “some” refined grains are good, partly because Asian countries and specifically Okinawa was a big reference. But that’s actually not as true he makes it. The traditional Okinawan staple was the purple sweet potato, not refined grains such as white rice. He claims that Okinawans shifted post WW2 to white rice - but not everyone actually did this. The ones that made shifts (he does mention Westenization and Western diets) eventually ended up closer to the Japanese average life expectancy. He doesn’t seem to have caught this or he might be subtly overlooking data in favor of his conclusion on dietary iron without enough evidence.
I do get his concern on the oxidation of oils. There is a simpler answer - consider avoiding canola oil and eat mixed nuts and fish with some real EVOO for cooking (don’t buy bulk, only small batch) if you wish, and put nuts and fish in the fridge, preferably sealed to slow oxidative processes. Nuts and fish are convenient to put in the fridge, but vegetable oils aren’t if you ever tried his recommendations you’ll see it takes a fairly long time to become liquid again (fat oxidation isn’t particularly a new issue either even before his claims). The canola oil recommendation just seems pretty impractical when you actually try it with all the factors considered. He also seems to be pretty broad in the negatives towards saturated fat recommendations due to LDL, but he isn’t precise and appears to be overgeneralizing - i.e. stearic acid isn’t significantly LDL increasing and potentially slightly LDL lowering, but coconut oil, which he says is a healthful fat without any supportive evidence isn’t necessary the case with much, much more palmitic acid, lauric acid, and myrisitic acid that constitute near 90% that goes against at least his stated reasoning which is firmly based on the LDL hypothesis. He doesn’t seem to be particularly exceptional at rigor in some of his dietary conclusions based on the reasoning presented. That’s below my expectations for any book that is literally a diet book
The calcium supplementation fortification is alleviating a deficiency, there is no difference between calcium in food and supplements. I think those supplements studies are in people with already high or RDA intakes of calcium. I take a 500 mg Calcium Sandoz supplement everyday. I think I get around 600 or 700 mg in total then. I don’t drink milk or calcium fortified foods.
See why calcium supplements may increase the risk of heart disease even if it’s to relieve a deficiency, which will likely apply to fortified foods depending on the situation.
You claim no difference, but did you actually check? It might seem trivial…until it isn’t.
I don’t see the difference between calcium from a supplement or from food. Calcium in a supplement might have been shown to cause an increase risk of heart disease, but I don’t see why it wouldn’t be the same for calcium in food as well. The results seem mixed:
Based on an updated review of the literature that included four randomized controlled trials, one nested case-control study, and 26 prospective cohort studies (170), the National Osteoporosis Foundation (NOF) and the American Society for Preventive Cardiology (ASPC) concluded that the use of supplemental calcium for generally healthy individuals was safe from a cardiovascular health standpoint when total calcium intakes did not exceed the UL (171). NOF and ASPC support the use of calcium supplements to correct shortfalls in dietary calcium intake and meet current recommendations (171).
Please read the cited study - it cites multiple human trials. It also goes in detail the limitations of what you’re citing, reanalyses, and why there is likely a real effect.
I’m not saying there isn’t a real effect. I doubt the claim that dietary calcium somehow doesn’t have the same effect, that is not proven, and it seems very likely to be the same to me. There are trade offs with everything. I don’t want broken bones, and limitations of the studies along with mixed results doesn’t make the picture super clear. Supplemental calcium can easily be studied in a proper way, dietary calcium not so much.
It explains the leading theory - supplementary calcium may be too rapidly absorbed and dietary calcium in a standard food matrix isn’t.
That’s a stretch from an already shaky hypothesis. It isn’t surprising since they work for the diary industry.
I don’t have a horse in this race. If you don’t see the issues and don’t want to read, alternatively I also suggest you actually talk to another independent doc familiar with the research and allay any concern of having a horse in the race so to speak for the following at the very least:
The cardiovascular risk of calcium supplements is not fully settled and it would be wise to avoid excess supplementation, particularly with doses over 500 mg at one time, while encouraging dietary intake over tablets.
I can agree to disagree with select forms of food fortification but I’m fairly certain about the above statement. I’m not part of the dairy industry nor do I even recommend milk.
I’m not saying you have a horse in this race. One of the authors you linked works for the diary industry.
I don’t really care about conflicts of interest, the methodology is what’s important. It has not been proven that dietary calcium does not have the same effect as supplemental calcium. That’s all I am trying to say. Absence of evidence does not mean evidence of absence.
I’m having a hard time seeing the difference of a large glass of milk and calcium in water, especially taken with food.
If you read the citations you are looking at - the limitations actually reveal the exact same issues with methodologies, so it’s not without a point bias or not. The only reason I cited it is that it details the arguments better in one place rather than me compiling a bunch of references. It’s literally not a resolved issue.
I suggest you read the physical properties and how absorption works from a standardized food matrix. It is precisely more concerning in supplement or liquid forms, and likely at 500 mg or above. It doesn’t seem like you read the mechanistics here.
Again, I haven’t ever recommended milk once, I also avoid things like fortified soy milk out of an abundance of caution. But if you have a higher risk tolerance, I suspect a small cup with food would be an option if one really, really enjoys milk.
I generally mention a mix of fish such as sardines, beans, nuts, and leafy greens to get to recommended calcium intakes.
I don’t think getting calcium from sardines is going to spare anyone from the risks of calcium, I think it is pretty much exactly the same. Also taking with food seems like it can slow absorption by a lot.
Bonemeal (sardines are high in calcium because of bones):
And these types of studies are very low on the evidence hiearchy, and just a hypothesis that is not proven at all.
Sardines automatically come with a contribution to a food matrix. I’m assuming one doesn’t simply only eat fish bones all day.