A simple method is just track a fixed power/heart rate curve. For example what is your HR at steady state 125w. Then reduce to 50W and see how long it takes for HR to reduce to 80%,
Could this pricing{$49.00 per draw] be available/made available to member’s/users on this forum?
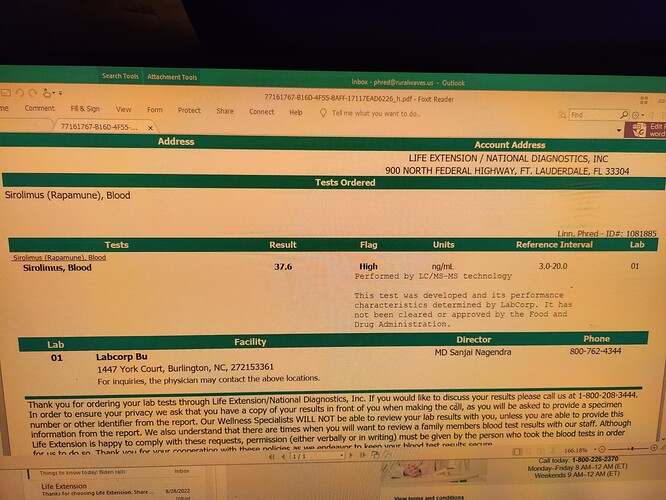
Just to confirm that is 37.6 ng/ml? Not PPM. Is so that is a very good level.
Did you take GFJ prior to or with the sirolimus?
What concentration? 1 or 2 mg.
What formulation did you use? Pfizer Rapamune or Generic. If so know the brand?
Dr. Reddys is triangular with number 53 or 54.
All these details make a difference.
One of our members found this test for $56 (a total of $64 for the total service): Inexpensive Serum Blood Test for Rapamycin
I did drink GFJ, probably 24 oz. Otherwise I think I was fasting that day and it was first thing in the morning.
It was for sure Generic and almost certainly Biocon. Rapacon. Just a line across the top of the tablet. 1mg. I had some other generics at the time from Wal Mart, and it’s been awhile, but I’m pretty sure. I think I wrote about it on here and probably said.
I don’t think there is any difference in these tablets and I’ve used several kinds. They all give me clues that tell me I’m getting the real thing. I just tested because I like numbers.
Saliva won’t work for sirolimus. But I would be happy with an at-home microtube draw and stoked for bloodspot. These are doable but need more people checking levels so we can go to a lab and offer at least a few hundred or more samples a month to make it worth their while to update systems.
Yes both purity and efficacy need to be confirmed. I am working with a vetted supplier of nanoparticle sirolimus in Asia that has 3rd party testing and we will be sending the final ingredients to a lab in Israel to do pharmacokinetics. Price should be less than $2 mg. This would be available without an RX.
For labs or the meds? We want to run 4 more people comparing levels to generic and then send the samples to Israel for full analysis. It will be a few months. I’ll let people know.
Low doses of rapamycin in the range of 4-6 mg/week, or 1 mg every other day, can also induce an inflammatory syndrome. Unfortunately it did with me, starting with transient pruritis and joint pains, and ending with the exacerbation of an immune-related myocarditis condition that I was taking it to prevent.
I had new and more frequent heart pain - once after a weekly dose of 4 mg and once after a 6 mg dose. Then after switching to 1 mg every other day, I had new mild, but continual heart discomfort with new left shoulder pain on and off for 2.5 weeks. Toward the end of that episode, I ran some blood tests and found by CRP had shot up from 0.8 to 25.4. I also had low hemoglobin and hematocrit, and a high neutrophils/Lymphocytes ratio of 3.1. So that’s the end of that experiment, for now.
It’s possible that this happened because I have an autoimmune condition and/or my immune system is dysfunctional in some other way. It could be that that I need to take it more slowly, that the rapamycin can still have a beneficial effect on my immune system and help in the long run, for example, by increasing Tregs per this study involving people with rheumatoid arthritis: Low-Dose Sirolimus Immunoregulation Therapy in Patients with Active Rheumatoid Arthritis: A 24-Week Follow-Up of the Randomized, Open-Label, Parallel-Controlled Trial - PMC. Then again, I found this study in mice showing that low dose, but not high dose, rapamycin can exacerbate and prolong autoimmune disease: Low dose rapamycin exacerbates autoimmune experimental uveitis - PubMed Then there is the paper you cited about sirolimus-induced inflammatory syndrome.
I am not ready to give up so will take a break for a couple of months and may try again, possibly with lower dosing and longer intervals, while monitoring my inflammatory markers more frequently.