I’ve seen Matt Kaeberlein mention that he doesn’t think that rapamycin is a very strong immune suppressant. I was wondering if anyone has seen any specific data related to the dose/response relationship of rapamycin in terms of immune suppression, especially compared to the most popular immunosupressant cyclosporin: https://en.wikipedia.org/wiki/Ciclosporin
Obviously this is an important issue as the primary theory on why we shouldn’t be dosing at high levels (over a long period of time) is that eventually these high and regular dosing of rapamycin will cause mTORC2 inhibition and then immune suppression. I don’t doubt that this is true at some level, but what I’m wondering is specifically how much immune supression we will actually see, and what that means in the real world.
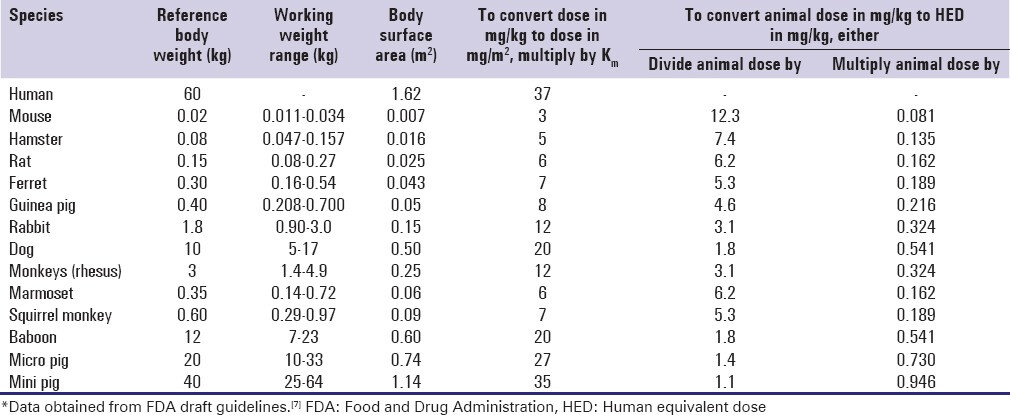
Part of the reason I’m asking this is because I’ve recently communicated with an independent researcher who is doing testing with high dose rapamycin in rat communities at his own home. And by “high dose” I’m talking 100mg/kg to 200mg/kg per day (by IP / SC injection), in very non-sterile environmental conditions, and he’s not seeing any issues with regard to immune system related issues. To put this in perspective, this is the highest ongoing dosing level experiment I’ve ever heard of or seen. I’ve looked in all the literature and the highest dosing ongoing experiment I’ve ever seen is 100mg/kg for a few weeks in mice and rats. So, short of doing LD50 experiments (testing dosing levels to find the point that is lethal for 50% of the population), this is one of the highest dosing levels ever done in rats.
This is a small and low-cost personal project by this individual working with a large number of rats in a garage. This is not a typical lab-like environment with its pathogen free environment (purified air cycled through HEPA filters, autoclaved cages and equipment, purified water, etc.).
This experiment is comprised of rats from a local vivarium purchased for $3 each (vs. $60 per sterile rat from Jackson Labs for true lab rats), no autoclaving of cages and equipment, no masks, no sterile food, etc… The environment these high dose rats are living in are pretty similar to a human environment… a regular garage, plastic crates from Costco, being fed regular dogfood and left over old vegetables, tap water for drinking, etc. And these rats are living in relatively crowded environments; up to 14 rats in a crate. So if there are any immune system issues, you’d expect him to see them in this type of environment.
So - I’m starting to wonder, how truly immunosuppressant is rapamycin? Is there some agreed to classification or measure of immunosupressants? Does anyone have any information on this, before I start doing a deep dive into the issue?
How exactly is risk quantified with regard to immunosuppressants? Are there some general benchmarks that they might use in transplant patients - e.g. T-cell counts, or other mechanism or ranges?