The video explains why measuring lipoprotein particle numbers, especially ApoB, is crucial for assessing cardiovascular risk.
Key Points from Dr. Tom Dayspring’s Grand Rounds on Lipids and Cardiovascular Risk
1. Lipoproteins vs. Lipids
- Atherosclerosis is caused by the accumulation of steroid foam cells in arterial walls, a process driven by lipoproteins, not just cholesterol or lipids.
- Lipoprotein concentrations are dynamic and not routinely measured in clinical practice; lipid concentrations are often used as surrogates, but risk follows lipoprotein numbers more closely.
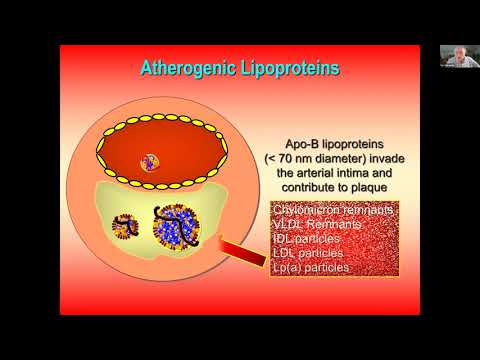
2. Beta Lipoproteins and Atherogenesis
- Beta lipoproteins (ApoB-containing particles) are the key mediators of atherogenesis. Recognizing and modulating these is essential, regardless of cholesterol metrics.
- Only ApoB particles smaller than 70 nanometers (LDL, remnants, and Lp(a)) can penetrate the arterial wall and initiate atherosclerosis.
3. Lipoprotein Particle Measurement
- Measuring ApoB provides a direct count of all atherogenic particles, as each particle contains one ApoB molecule.
- LDL metrics dominate because 90% of ApoB particles are LDLs.
- Advanced tests (NMR, ion mobility) can count LDL particles, but ApoB is a simpler, widely available metric.
4. Cholesterol Synthesis and Transport
- Cholesterol is synthesized in many tissues, not just the liver; the majority is in peripheral tissues and the brain.
- Cholesterol transport involves complex interplay between synthesis, absorption, and excretion, with reverse cholesterol transport (RCT) performed by both LDL and HDL particles.
- Fecal excretion is the only way the body eliminates cholesterol.
5. Lipid Panel Limitations
- Standard lipid panels report lipid concentrations, not lipoprotein numbers. LDL and HDL are lipoproteins, not direct lab tests.
- LDL cholesterol and non-HDL cholesterol are used as therapy goals, but only LDL cholesterol and non-HDL cholesterol are meaningful for tracking therapy efficacy.
- HDL cholesterol should not be used as a goal of therapy; raising it does not improve outcomes.
6. Triglycerides and Lipoprotein Discordance
- Triglycerides are measured in all lipoproteins; high triglycerides often signal insulin resistance and high ApoB particle numbers, even if LDL cholesterol is normal.
- Discordance between LDL cholesterol and ApoB/LDL particle count is common, especially in diabetics and those with insulin resistance.
7. Lipoprotein(a) [Lp(a)]
- Lp(a) is a highly atherogenic LDL particle with an additional apoprotein (Apo(a)), increasing risk for atherosclerosis and calcific aortic stenosis.
- Lp(a) should be checked at least once in life, especially in those with premature heart disease or family history.
- No approved therapies currently lower Lp(a) directly, but trials are underway. Statins, ezetimibe, bempedoic acid, and PCSK9 inhibitors are used to lower ApoB and overall risk.
8. Therapy and Guidelines
- Statins are the primary ApoB-lowering therapy; PCSK9 inhibitors also lower Lp(a).
- Guidelines are moving toward using ApoB as the main metric for risk and therapy monitoring.
- LDL particle size is less important than particle number for risk; size may indicate insulin resistance but is not a primary therapeutic target.
9. Omega-3 Fatty Acids
- Icosapent ethyl (EPA) at 4g/day reduces cardiovascular risk beyond statins, with benefits not solely due to triglyceride lowering.
10. Historical Perspective
- The understanding of lipoproteins and their role in cardiovascular disease has evolved over decades, with key contributions from researchers like Paul Wood and John Gofman. ,