It’s interesting… perhaps it depends on how you ask the question, also. I tried a slightly different question, trying to be as specific as I can. I believe that Radiesse needs to get at least down to the Mid-dermis for collagen stimulation.
It seems, from your experience, and the Instagram post you cited, Radiesse can at least be delivered sub-dermis. The open issue is how deep it goes, and does it work as a biostimlator at that level that it does get to.
So, Here is one of my attempts on Google (just using the standard google search bar):
Prompt:
can hyperdilute radiesse be delivered successfully to the mid-dermis or deep dermis in people using dermo-electroporation?
Response:
Delivering hyperdilute Radiesse to the mid- or deep dermis using dermo-electroporation (DEP) is not feasible. The calcium hydroxylapatite (CaHA) microspheres in Radiesse are far too large to pass through the temporary micro-channels created by DEP technology.
Here’s a detailed breakdown of why this method is unsuccessful:
- CaHA particle size: The CaHA microspheres in Radiesse range from 25 to 45 microns in diameter. This is a very large size for a particle to be delivered transdermally (across the skin).
- DEP delivery mechanism: DEP works by using electrical pulses to open temporary, microscopic channels in the skin to increase permeability. This allows for the non-invasive delivery of water-soluble molecules.
- DEP delivery limits: Even advanced DEP systems can only deliver substances to a maximum depth of 3 to 5 mm, targeting micro- and macro-molecules up to 800,000 Daltons. The solid, particulate CaHA microspheres in Radiesse are much larger than the molecules that DEP can transport.
- Radiesse injection method: For hyperdilute Radiesse to reach the mid-to-deep dermal layers, it must be injected using a cannula or needle, which physically places the substance into the desired depth. This is how the treatment is performed in clinical practice.
Conclusion
While dermo-electroporation is an effective, non-invasive method for delivering certain active ingredients like hyaluronic acid or peptides into the dermis, it is completely unsuitable for delivering a particle-based product like hyperdilute Radiesse. For Radiesse to be successfully administered to the dermis, a medical professional must use a needle or cannula injection.
Another Question Approach with Google Search AI results:
Prompt: can hyperdilute radiesse be delivered successfully using dermo-electroporation?
Response:
Yes, hyperdilute Radiesse can be delivered successfully using dermo-electroporation
(DEP). DEP is a needle-free system that is used as an alternative delivery method for substances like hyperdilute Radiesse, which is known for its ability to stimulate collagen production.
How dermo-electroporation (DEP) works
- Dermo-electroporation is a non-invasive, powered drug-delivery system that increases the permeability of the skin.
- It works by applying a controlled current to the patient’s skin, which temporarily opens water-based channels in the skin.
- This allows both micro- and macromolecules to be absorbed into the deeper layers of the skin, including the hypodermis and muscle membranes, without the use of needles.
Another Question Approach with Google Gemini:
Prompt:
can hyperdilute radiesse be delivered successfully to the mid-dermis or deep dermis in people using dermo-electroporation?
Response:
Based on the available information, the use of dermo-electroporation (DEP) to successfully deliver hyperdilute Radiesse (a Calcium Hydroxylapatite or CaHA product) specifically into the mid-dermis or deep dermis is a complex question with some conflicting or limited data.
Here’s a breakdown of the key points:
-
Hyperdilute Radiesse:
- It is a formulation of the Radiesse dermal filler diluted with saline and often lidocaine, resulting in a thinner, more spreadable solution.
- It is typically used as a biostimulator to promote collagen and elastin production, often targeting larger areas and improving overall skin texture and laxity.
- The standard, current clinical practice for delivery is injection (usually with a cannula) into the dermal layer or different depths within the dermis depending on the treatment area, not via a non-invasive device like electroporation.
-
Dermo-Electroporation (DEP) Technology:
- DEP systems are FDA-cleared for the local administration of ionic drug solutions into the body as an alternative to injections.
- It uses controlled electrical pulses to create temporary micro-channels in the skin, enhancing permeability and facilitating the transdermal delivery of substances.
- Some DEP device manufacturers claim they can infuse high-weight molecules, including certain dermal fillers (like RHA Redensity), neurotoxins, or Sculptra (another biostimulator), to depths of 3.0 to 5.0 mm into the dermis.
- A depth of 3.0 to 5.0 mm would generally be considered within the range of the deep dermis or extending into the subcutaneous tissue.
-
The Conflict/Uncertainty:
- While some DEP manufacturers claim the capability to deliver high molecular weight components (like fillers or biostimulators), and even specifically mention delivering dermal fillers, there is a lack of widespread, independent, peer-reviewed clinical studies specifically confirming the successful, effective, and uniform delivery of the calcium hydroxyapatite microspheres in hyperdilute Radiesse to the intended mid-dermis or deep dermis layer using DEP.
- One source reviewing the use of electroporation for another injectable moisturizer (a hyaluronic acid complex) noted that most studies show increased uptake in the epidermis, not the deep dermis, which is the correct layer for the product’s maximum benefit. This highlights a potential limitation of transdermal delivery devices compared to direct injection.
Conclusion:
While DEP technology is marketed as capable of delivering various high-weight molecules into the dermis up to $5.0 \text{ mm}$, direct, definitive evidence confirming the clinical success and efficacy of delivering hyperdilute Radiesse’s CaHA microspheres to the deep dermis using dermo-electroporation is not readily available in standard clinical literature. The primary and widely accepted method for delivering hyperdilute Radiesse remains injection with a needle or cannula.
Another Question Approach with Google Gemini:
Prompt:
can hyperdilute radiesse be delivered successfully using dermo-electroporation?
Response:
The short answer is: Probably not effectively, based on the current scientific understanding and clinical practice.
Here is the detailed explanation:
The Challenge of Particle Size
Hyperdilute Radiesse works because of its active ingredient: Calcium Hydroxylapatite (CaHA) microspheres . These are microscopic particles suspended in a gel.
- CaHA Microsphere Size: Radiesse microspheres typically have a diameter of 25 µm to 45 µm (micrometers) .This is a relatively large particle size.
- Dermo-Electroporation (DEP) Mechanism: DEP works by using controlled electrical pulses to create transient, aqueous pores (nanopores) in the stratum corneum (the skin’s outermost layer) and lipid bilayers. This enhances the delivery of substances through the skin.
- The Barrier: While DEP is highly effective for delivering small molecules (like certain peptides or vitamins) and some macromolecules (like hyaluronic acid, which can be broken down to smaller fragments), delivering solid microspheres in the 25-45 μm range is likely beyond the capability of the temporary pores created by DEP. The pores created by electroporation are typically on the nanometer scale.
Clinical Practice vs. DEP Claims
- Standard Clinical Protocol: The universally accepted and evidence-based method for delivering hyperdilute Radiesse is injection (using a needle or cannula) directly into the desired layer of the skin (subdermal or deep dermis). This method physically places the CaHA microspheres where they can contact fibroblasts and stimulate collagen.
- DEP Device Claims: Some DEP device manufacturers claim they can deliver a wide variety of macromolecules, even mentioning fillers or biostimulators, to the deep dermis (up to 3-5 mm). However, there is a significant lack of independent, peer-reviewed clinical studies specifically demonstrating the successful delivery of solid, large CaHA microspheres with DEP to a depth that would produce the collagen-stimulating effects seen with injection.
- Depth Limitation: Studies on similar large-molecule delivery via electroporation sometimes suggest that most of the uptake concentrates in the epidermis , failing to reach the crucial deep dermis where the fibroblasts need to be activated by the CaHA particles. The collagen-building effect requires direct contact between the CaHA microspheres and the dermal fibroblasts.
In summary, the sheer size of the CaHA microspheres makes their successful transport through the microscopic, temporary channels created by dermo-electroporation highly improbable, and this approach is not supported by established clinical guidelines for Radiesse.
Another Question Approach with Anthropic Claude:
Prompt:
can hyperdilute radiesse be delivered successfully to the mid-dermis or deep dermis in people using dermo-electroporation?
Response
Based on my search, I cannot find any published evidence or established protocols for delivering hyperdilute Radiesse (calcium hydroxylapatite) using dermo-electroporation. Here’s why this appears to be problematic:
Standard Delivery Methods for Hyperdilute Radiesse
Hyperdilute Radiesse is traditionally delivered using needles or blunt-tipped cannulas through injection techniques AAFEPubMed Central. The standard approach involves superficial injection using microboluses, tunneling, and/or fanning techniques to place the diluted material in the dermis PubMed Central.
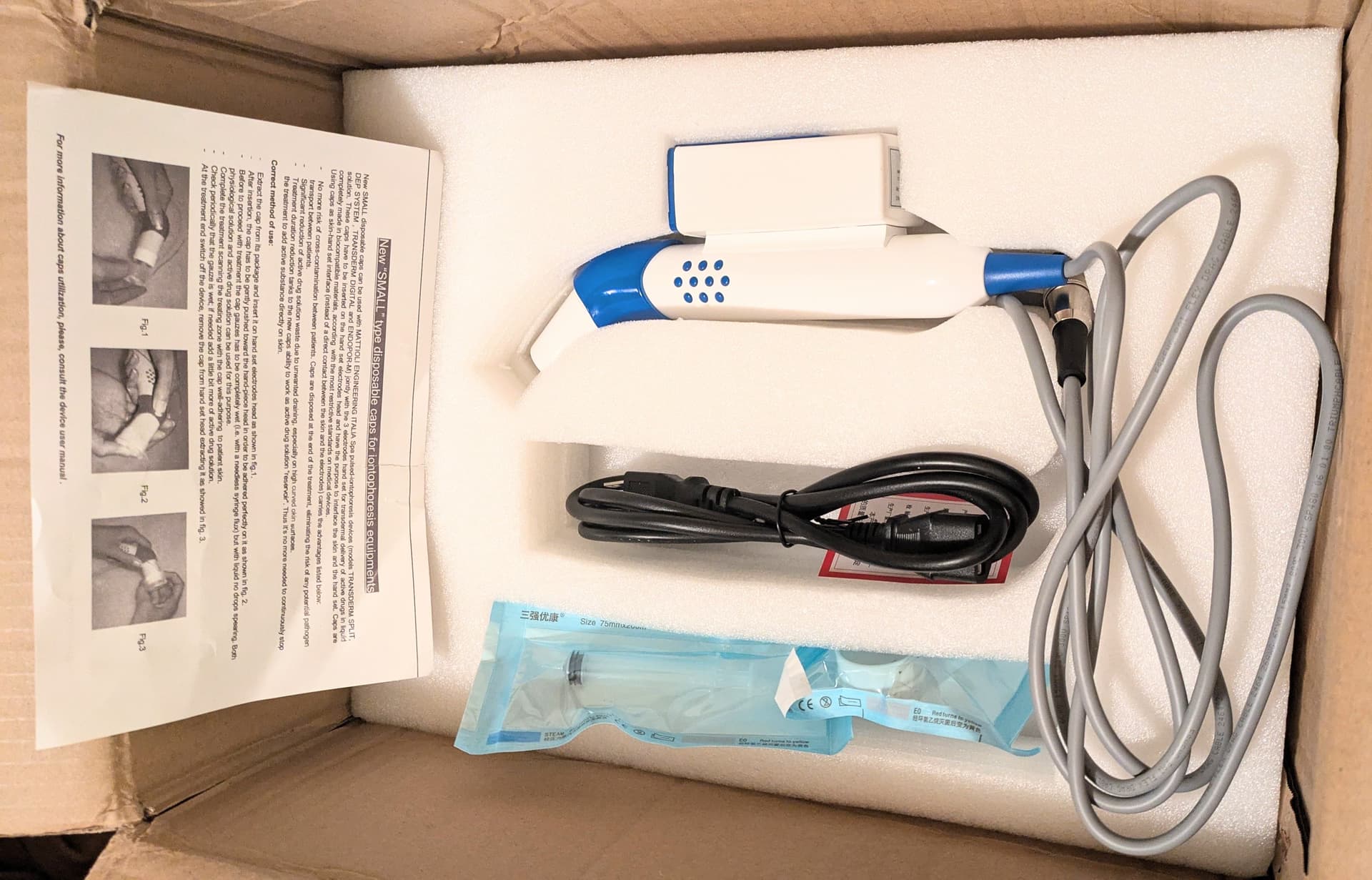
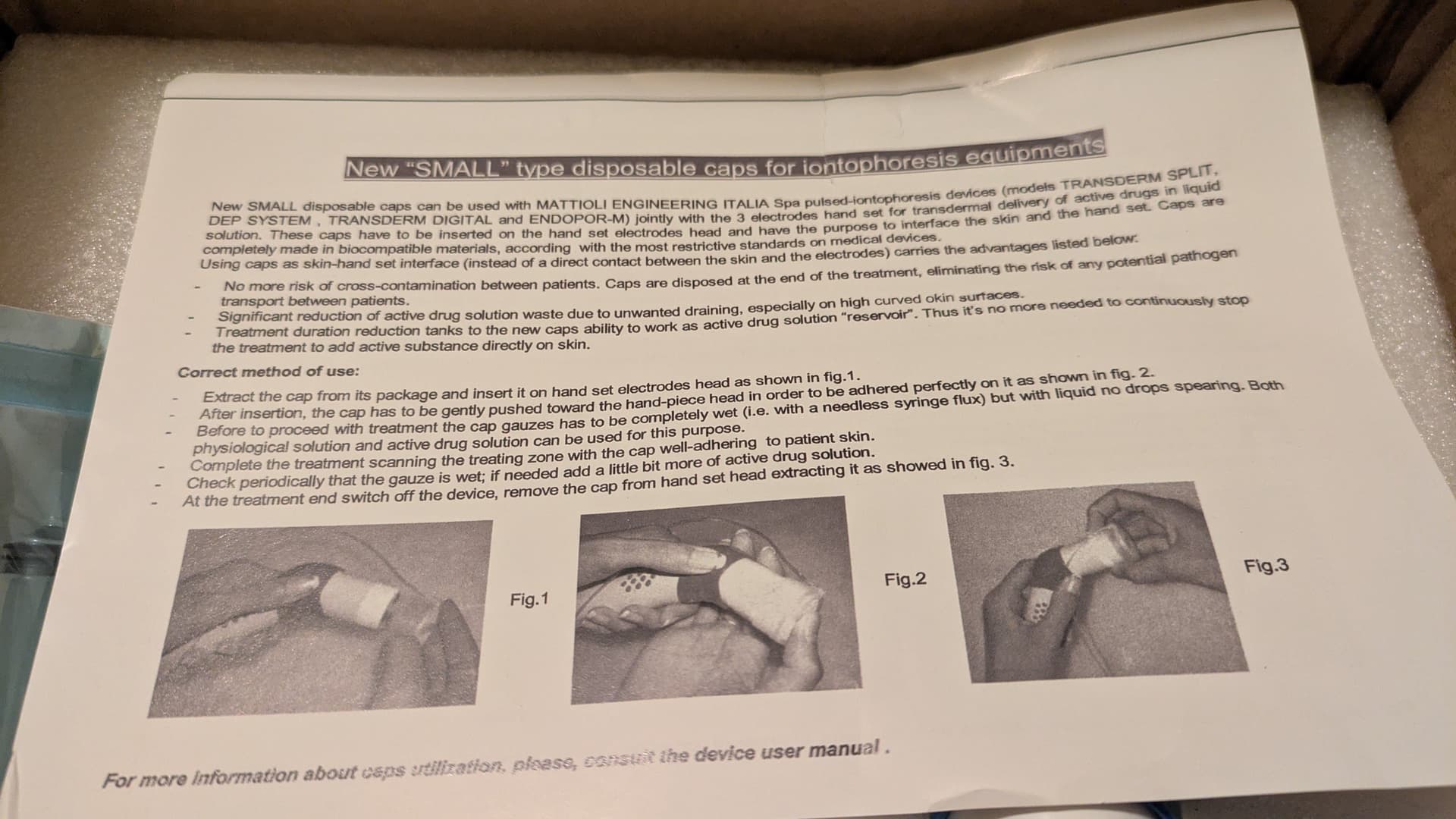
Dermo-Electroporation Technology
Dermo-electroporation uses controlled electrical pulses to create temporary channels in the skin, allowing transdermal delivery of ionic drug solutions at depths of 3-5mm RegenomedixDEP Medical. The technology can deliver molecules greater than 800,000 Daltons Regenomedix.
Key Compatibility Issues
There are several fundamental problems with combining these technologies:
- Physical Properties: Radiesse contains calcium hydroxylapatite microspheres that are 25-45 microns in diameter suspended in a gel carrier Medscape ReferencePubMed Central. These are physical particles, not ionic solutions that dermo-electroporation is designed to deliver.
- Mechanism Mismatch: Dermo-electroporation is designed for water-soluble ionic drug solutions RegenomedixDEP Medical, whereas Radiesse is a particulate suspension that requires mechanical placement.
- Lack of Evidence: I found no published studies, clinical protocols, or manufacturer guidance supporting this combination approach.
Clinical Recommendation: Given the lack of evidence and the incompatibility between the particulate nature of Radiesse and the ionic solution requirements of dermo-electroporation, this combination should not be attempted. Hyperdilute Radiesse should be delivered using established injection techniques with needles or cannulas as supported by clinical evidence.
Another Question Approach with Grok:
Prompt:
can hyperdilute radiesse be delivered successfully using dermo-electroporation?
Response
Overview of Hyperdilute Radiesse and Dermo-Electroporation
Hyperdilute Radiesse refers to calcium hydroxylapatite (CaHA) filler (the active ingredient in Radiesse®) mixed with saline and/or lidocaine at a ratio of 1:2 or higher, transforming it from a volumizing agent into a biostimulatory treatment. This dilution reduces viscosity, allowing superficial injection to promote neocollagenesis (new collagen production), elastogenesis, and improved skin quality, elasticity, and firmness without significant volume addition. It is commonly used for skin laxity, fine lines, crepiness, and cellulite on areas like the face, neck, décolletage, arms, and thighs.
Dermo-electroporation (also known as dermoelectroporation or DEP) is a non-invasive transdermal delivery technology that uses controlled electrical pulses to create temporary micro-channels in the skin’s lipid bilayers. This enhances permeability, enabling the delivery of macromolecules (up to 800,000 Daltons) into the dermis and hypodermis (up to 5 mm depth) without needles. Unlike traditional iontophoresis, it avoids pH adjustments or electrolysis and is FDA-cleared for medical drug delivery. It is often paired with serums, hyaluronic acid, or peptides for rejuvenation.
Can Hyperdilute Radiesse Be Delivered Successfully via Dermo-Electroporation?
Based on available evidence, there is no documented clinical use, study, or guideline supporting the successful delivery of hyperdilute Radiesse via dermo-electroporation. Radiesse, even in hyperdiluted form, is explicitly designed and approved as an injectable subdermal implant (FDA-cleared for injection via needle or cannula). Its CaHA microspheres (25–45 microns in diameter) are suspended in a carboxymethylcellulose gel carrier, which requires mechanical deposition into the subcutaneous or dermal layers to achieve therapeutic concentrations and stimulate fibroblast activity.
Key reasons this combination is unlikely to be successful or standard practice:
- Delivery Mechanism Mismatch: Dermo-electroporation excels at transdermal diffusion of ionic solutions, water-soluble actives, or low-viscosity fluids (e.g., hyaluronic acid serums, vitamins, or peptides). However, hyperdilute Radiesse remains a semi-viscous suspension of microspheres. The electrical pulses may not effectively “transport” these particles through the stratum corneum without risking uneven distribution, aggregation, or skin irritation. Studies on electroporation focus on small molecules or soluble macromolecules, not particulate fillers like CaHA.
- Safety and Efficacy Concerns: Injecting Radiesse ensures precise placement (e.g., supraperiosteal or subdermal for volumization; subcutaneous for biostimulation). Transdermal electroporation could lead to superficial deposition only, reducing biostimulatory effects and potentially causing transient pore disruption without lasting benefit. No adverse event data exists for this pairing, but electroporation’s reversible barrier disruption (restoring in hours) may not suffice for CaHA’s gradual neocollagenesis (peaking at 3–7 months).
- Regulatory and Clinical Standards: All peer-reviewed guidelines (e.g., global consensus from Dermatologic Surgery, 2018; Plastic and Reconstructive Surgery Global Open, 2019) emphasize needle/cannula injection for diluted/hyperdiluted CaHA, with dilution ratios tailored to cannulas of specific gauges (e.g., 25–27G for 1:2 ratios). Electroporation is not mentioned in Radiesse’s instructions for use or biostimulation protocols.
| Aspect | Standard Hyperdilute Radiesse Delivery (Injection) | Dermo-Electroporation (Theoretical for Fillers) |
|---|---|---|
| Primary Method | Needle or cannula (e.g., 22–27G) | Electrical pulses creating micro-channels |
| Depth Achieved | Subcutaneous/dermal (up to 5–10 mm) | Dermal/hypodermal (up to 5 mm) |
| Suitable Substances | Viscous CaHA suspensions (diluted 1:1 to 1:6) | Ionic solutions, low-viscosity serums |
| Efficacy Evidence | High (e.g., 70–90% improvement in laxity after 2–3 sessions) | None for CaHA; effective for HA/peptides |
| Risks | Bruising, swelling (resolves 1–3 days); rare nodules | Skin tingling, temporary redness; potential uneven particle spread |
| Duration of Results | 12–24 months | N/A for this combo |
Recommendations
- Stick to Proven Methods: For hyperdilute Radiesse, opt for professional injection by a qualified dermatologist or aesthetic provider. Typical protocols involve 2–3 sessions spaced 4–8 weeks apart, with results visible in 1–3 months and lasting up to 2 years.
- Alternatives via Electroporation: If seeking needle-free biostimulation, dermo-electroporation pairs well with hyperdiluted hyaluronic acid (HA) or collagen-boosting serums for similar (but milder) skin tightening effects.
- Consult a Professional: Individual factors like skin type, age, and treatment area influence outcomes. Always discuss with a board-certified provider to avoid off-label risks.
If new research emerges (post-2025), this could change, but current data supports injection as the gold standard for hyperdilute Radiesse.