Yes, undoubtedly. It never occurred to me that it might make a difference what type of vaccine was being administered. Shingles will be more difficult because it’s now being administered with two doses.
Immunity wanes over time. I had a bad case and still have an intermittent chronic cough and decreased lung function. It’s treatable with an inhaled steroid that costs me $180 a month on my high deductible health plan. I’d rather avoid getting it again and the best way for me is to get a booster shot.
I think the vaccines are generally safe. I think Rapamycin is generally safe. I think it’s possible that the vaccine increases the risk that a child will get type 1 diabetes by 72% as on study suggested. But the odds are so vanishingly low that would mean that only 1 in 5000 would be affected. I saw a well documented n=1 account by a Doctor who was not a vaccine denier that suggested that the vaccine might have caused the spread of his lymphoma.
My take away is that it is possible that a few of us will suffer some serious adverse effects from this “safe” drug. It has been in use for a long time but with a low number of patients. The vaccine is new but it has been given to 1 billion patients. None of this alters my risk/reward ratio one iota. But you would hate to be that 1 in 5000.
But there is no evidence the vaccine gives you more protection than you already have but all medical procedures come with a risk of side effects (especially experimental ones). Vaccines are preventive so you are healthy now and might not even ever catch covid, do you are risking your health now for a problem you might never get
I have never had Covid. The vaccine gives me significantly more protection than I would have otherwise. That said, I just have to open Twitter and I can find a lot of support for your position without even scrolling.
My position is not a twitter position, it is what I was taught in med school regarding vaccines…
The vaccine saved me from getting COVID. I got the shot two weeks before all of my family and in laws got COVID. The ones who were vaccinated recently had minor cases. Those who were not vaccinated recently had more severe cases. Fortunately no one was hospitalised. I did not show up positive on PCR tests even though I was living in close quarters to COVID patients. I view that as an effective vaccine. I don’t know how bad it would be if I hadn’t been vaccinated.
After I got my 3rd dose, I did experience flu like symptoms.
My triple vaxxed girlfriend was out for a week whereas unvaxxed me barely noticed anything at all (even though I was on rapamycin )…
It is quite clear that vaccine efficacy rapidly wanes to negative
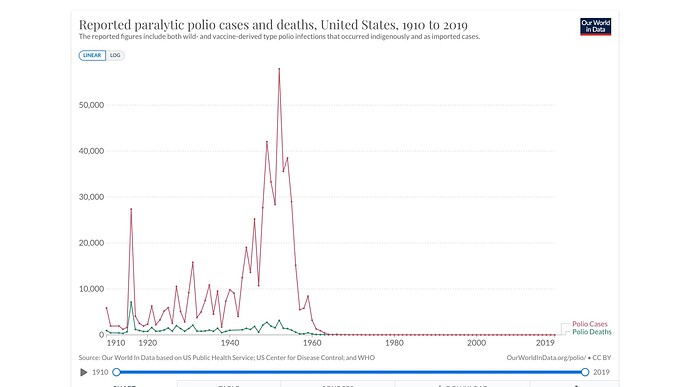
That sounds like a strong argument for not getting the polio vaccine. I am happy you were not leading health policy in the 1960s.
Like I said that’s not me it’s generally accepted medical practice. For polio the risk for getting serious complications from polio and the vaccine were completely different than from these experimental covid vaccines. We don’t even vaccinate the general population against influenza because the risk from vaccination doesn’t outweigh the benefits
You clearly lack the knowledge to asses the risk and benefits for an individual patient, covid doesn’t hit random people but a very certain group: those with metabolic syndrome, the elderly and those deficient in certain nutrients (vit d/k zinc, selenium) if don’t have any of those conditions there is only risk in taking these experimental vaccines
Ok, you have both stated your and given evidence. This is not the place to debate vaccines. Please agree to disagree and move on to new discussions.
Of course I completely forgot to wait a week after my vaccine to restart rapamycin. So I ended up starting five days later. So far so good.
Finally got COVID, and it’s pretty bad. Coughing up a lot of blood. Went to the hospital and am on Paxlovid and other flu meds. The meds seem to help a lot. It seems that all of my supplements couldn’t prevent it in the end. It’s just darn painful when I cough.
Hey Chris - Hang in there. Each of has phenotypes and blood types that respond differently. Some react as if nothing - for some it is life-threatenting.
I am glad you are getting all the bells and whistles to fight this virus. Being on Rapamycin is suppose to keep your immune system from over reacting.
Keep us informed of your progress back to health.
Well I am blood type O which is supposed to be most resistant. And I had 3 vaccine shots, but last one was a year ago. I dose Rapamycin on Saturday and got sick on Thursday so Rapa in my blood was pretty low. All in all, probably on par with a moderately bad flu except it hurts a lot more to cough. With the meds, I am probably on the mend. Going to rest and recover in isolation over the next five days according to the hospital’s guidelines.
Sorry to hear. Have you
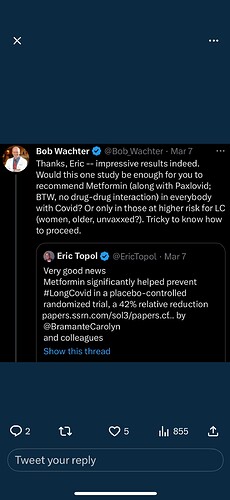
(A) seen that Paxlovid for 7-10 days may be better than 5 days to avoid rebound (and perhaps long covid)
(B) seen the data that Metformin for 14 days also may help decrease long covid
If not and interested I can dig up the stuff I read about either or both of above.
Hope you get well soon.
Unfortunately the doctors here only prescribe Paxlovid for 5 days. I do intend to continue taking Metformin after I am done with the Paxlovid. NMN is also supposed to help. I took some yesterday.
”Findings: Of 1323 randomized trial participants, 1125 consented for long-term follow up, and 95.1% completed >9 months of follow up. The median age was 45 years (IQR, 37 to 54), and 56% were female (7% pregnant). The median BMI was 30 kg/m2 (IQR, 27 to 34). Overall, 8.4% reported a medical provider diagnosed them with Long COVID; cumulative incidence: 6.3% with metformin and 10.6% with matched placebo. The hazard ratio (HR) for metformin preventing Long COVID was 0.58 (95%CI, 0.38 to 0.88; P=0·009) versus placebo. The metformin effect was consistent across subgroups, including viral variants. When metformin was started within <4 days of symptom onset, the HR for Long COVID was 0.37 (95%CI, 0.15 to 0.95). No statistical difference in Long COVID occurred in those randomized to either ivermectin (HR=0.99; 95%CI, 0.59 to 1.64) or fluvoxamine (HR=1.36; 95%CI, 0.78 to 2.34).”