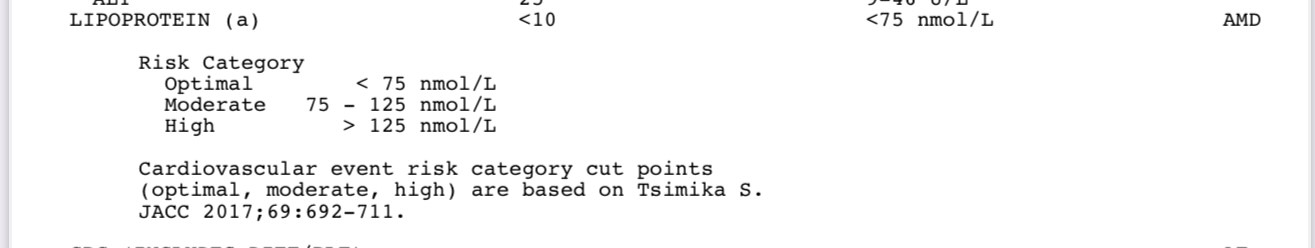
Sadly, yes. That said, there’s some new thinking in some quarters, that the Lp(a) situation is highly complex, and while the particle may be much more atherogenic than plain LDL, there’s some indication that there is some conditionality involved too, where it may end up not being particularly involved in plaque progression under some circumstances. FWIW, I had a CAC done at age 65 1/2, and my score was zero. Now, it’s possible that my arteries are riddled with soft plaque, but it’s still a surprising score to me, as I have had life long high LDL (165-185 mg/dL), and have only been on atorvastatin 10mg/day for about 5 years (and btw. not very effective, last October my LDL was 146 mg/dL, TC 240).
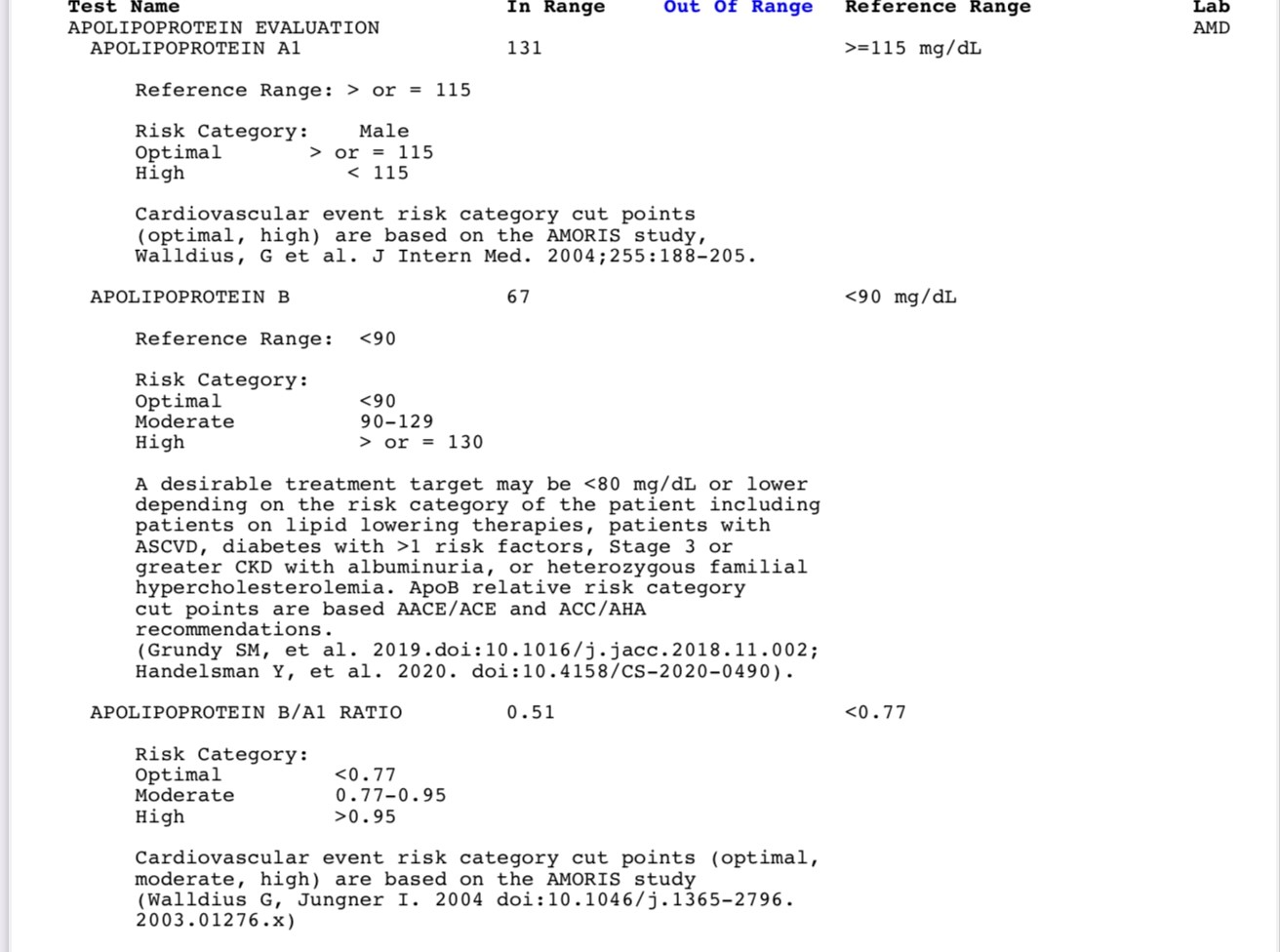
Anyhow, your LDL has been crushed at 32. Lp(a) is nasty, but fortunately it’s not a big component numberwise of your blood lipids, it’s dwarfed by LDL, so if you crush LDL, the Lp(a) is small change. Of course, the danger of Lp(a) is the calcification of the valve leaflets, so yeah, good drugs against it can’t come soon enough.
And your rosuvastatin is not very high intensity, so you don’t need more at 32mg/dL.
I’m awaiting my results. Right now, as of the past 6 months I’m on 4 mg/day of pitavastatin. Depending on what my lipid panel shows, I intend to push my LDL to below 60 mg/dL at least, or lower. For that I’m looking to 180 mg/day of bempedoic acid, and ezetimibe 10 mg/day… hopefully that will be enough.
But lipids lowering is only one CV therapy. I think, depending on the rest of your physiology, metabolic biomarkers, you may want to add a SGLT2i like empagliflozin that’s cardioprotective, perhaps an ARB, like telmisartan to keep your BP firmly below 120 SYS. Maybe additional therapies - rapamycin can be cardioprotective. Point being, you can’t just look at lipids. There is a lot more we should be doing to keep the CV system working, it impacts the brain too. Work in progress.