![]()
![]()
Yes, it is disconcerting. Chat GPT 5 (paid) quoted me from some thread on Rapamycin news as if I were some authority.
There seems to be some fundamental flaws in AI.
If you have access to OpenEvidence, it only uses the published literature as its sources, and gives full references (clickable that takes you directly to the abstract on PubMed).
I’m not very invested in this argument, but the biology seems pretty much identical (HG and chimps and modern humans) so at least its an indication that low is not harmful…
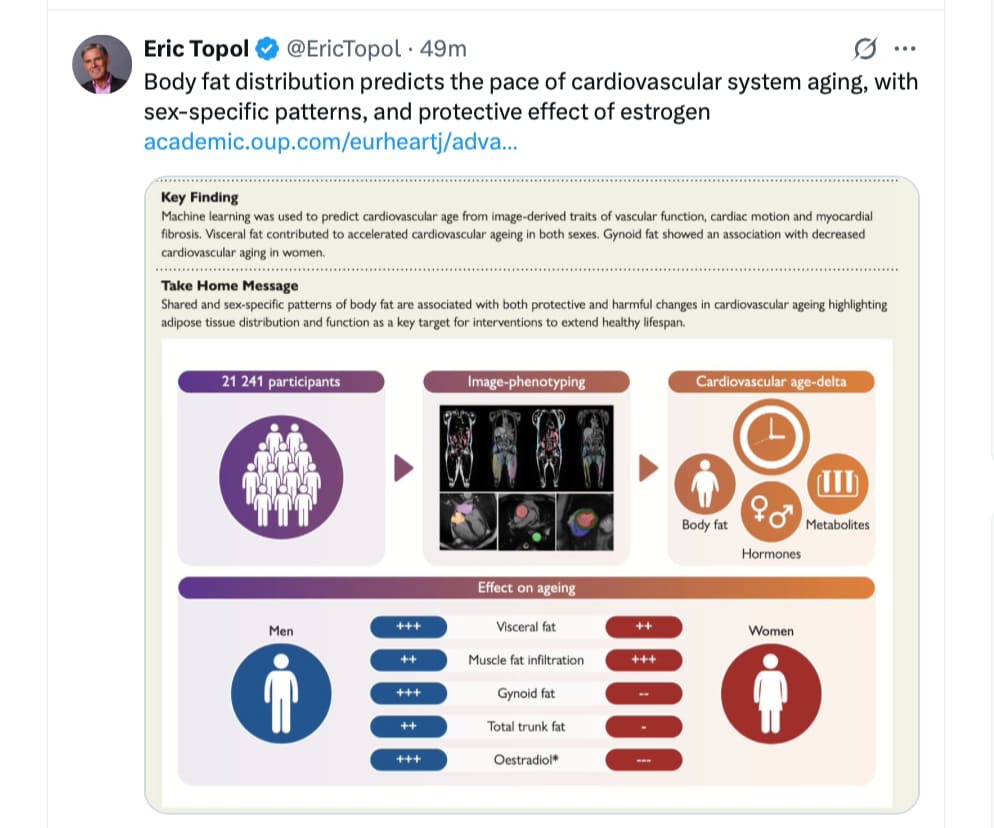
Open Access paper:
https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehaf553/8237967?login=false
a new paper:
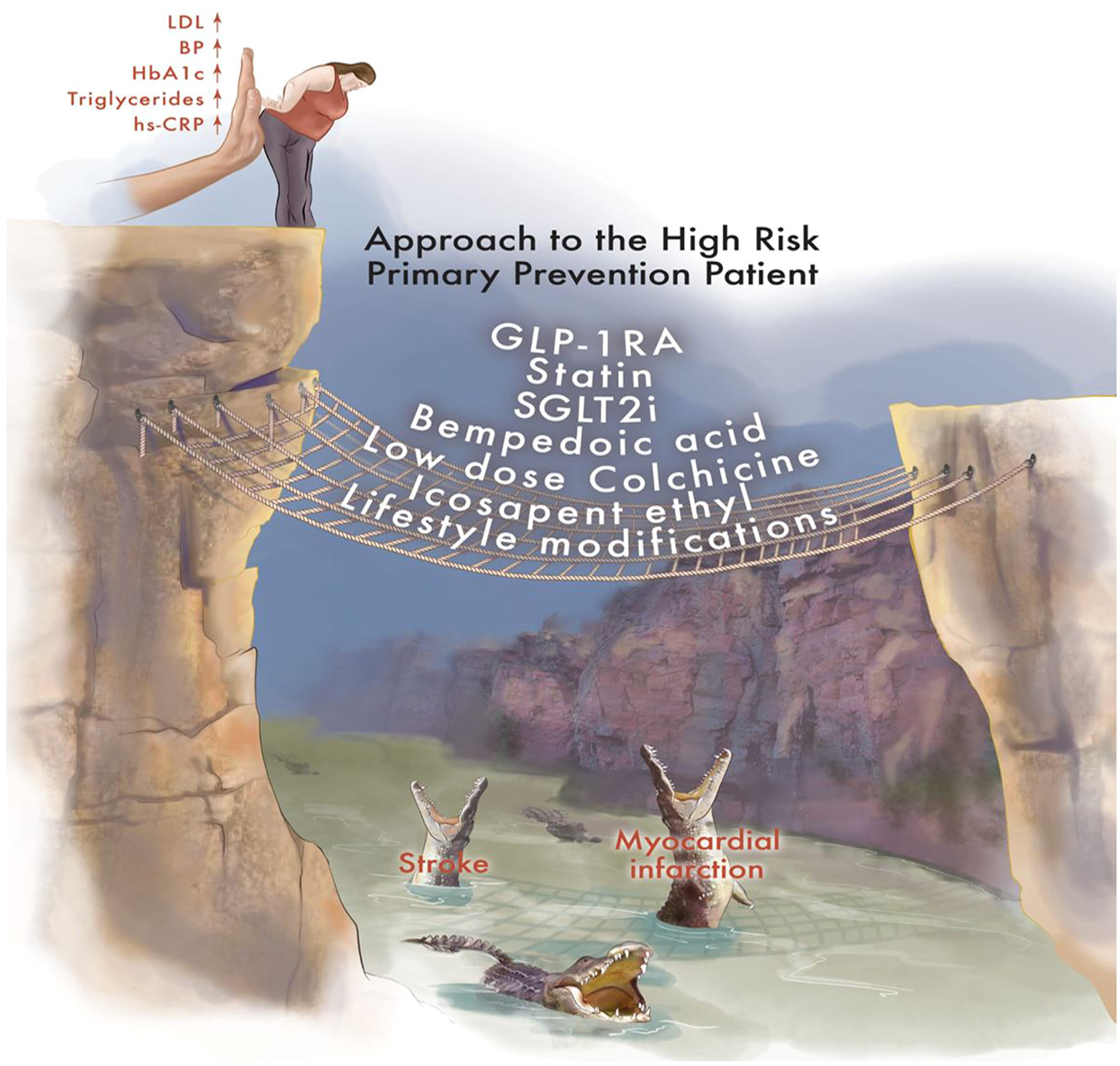
Identification and Management of Patients at High-Risk for Cardiovascular Disease in Primary Prevention
The medical community has traditionally dichotomized patients into primary and secondary prevention, which may be too simplistic. Recent biomarker, imaging, and pharmacotherapy trials have highlighted the importance of recognizing and treating subclinical atherosclerosis to mitigate the progression of subclinical disease and reduce the risk for highly morbid or lethal ASCVD events. Here, we describe the patient with subclinical atherosclerosis and risk factors as a “high-risk primary prevention” patient. Employing an optimal therapeutic strategy over the lifetime of a high-risk primary prevention patient can mitigate ASCVD progression and prevent ASCVD events. This review highlights biomarkers for identifying high-risk primary prevention patients and reviews clinical trials in this population. We then describe current data that guide the management of these patients and discuss future directions for management.
https://www.sciencedirect.com/science/article/pii/S266666772500340X
“Go ahead and JUMP!” - and guitar riff ![]()
![]()
I disagree, quoting you as an authority is a clear sign of intelligence!
I agree that the hunter gatherer argument is thin, but I do think it has some, albeit minor, interest/weight in the absence of long term, all cause mortality RCTs for Ldl-c lowering drugs in primary prevention.
The data is clear that lowering typical western ldl-c is beneficial but my main interest on this as a longevity issue is seeking to understand the optimum range for ldl-c.
The evidence points to anywhere between 10 to 80 which is pretty broad. And the data supporting a target below 50 is very thin. Which is why I’m always interested in academics who misrepresent the data to go lower.
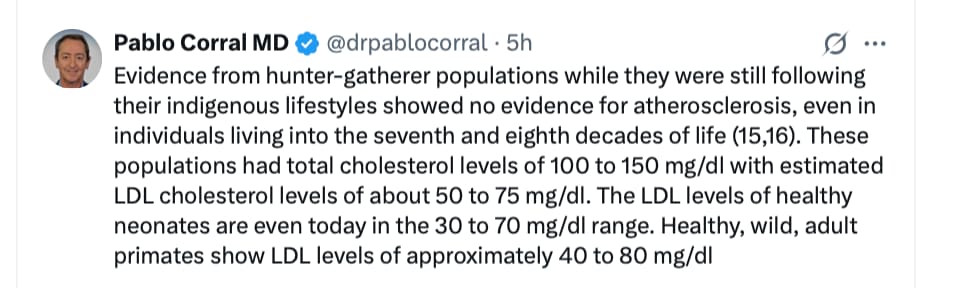
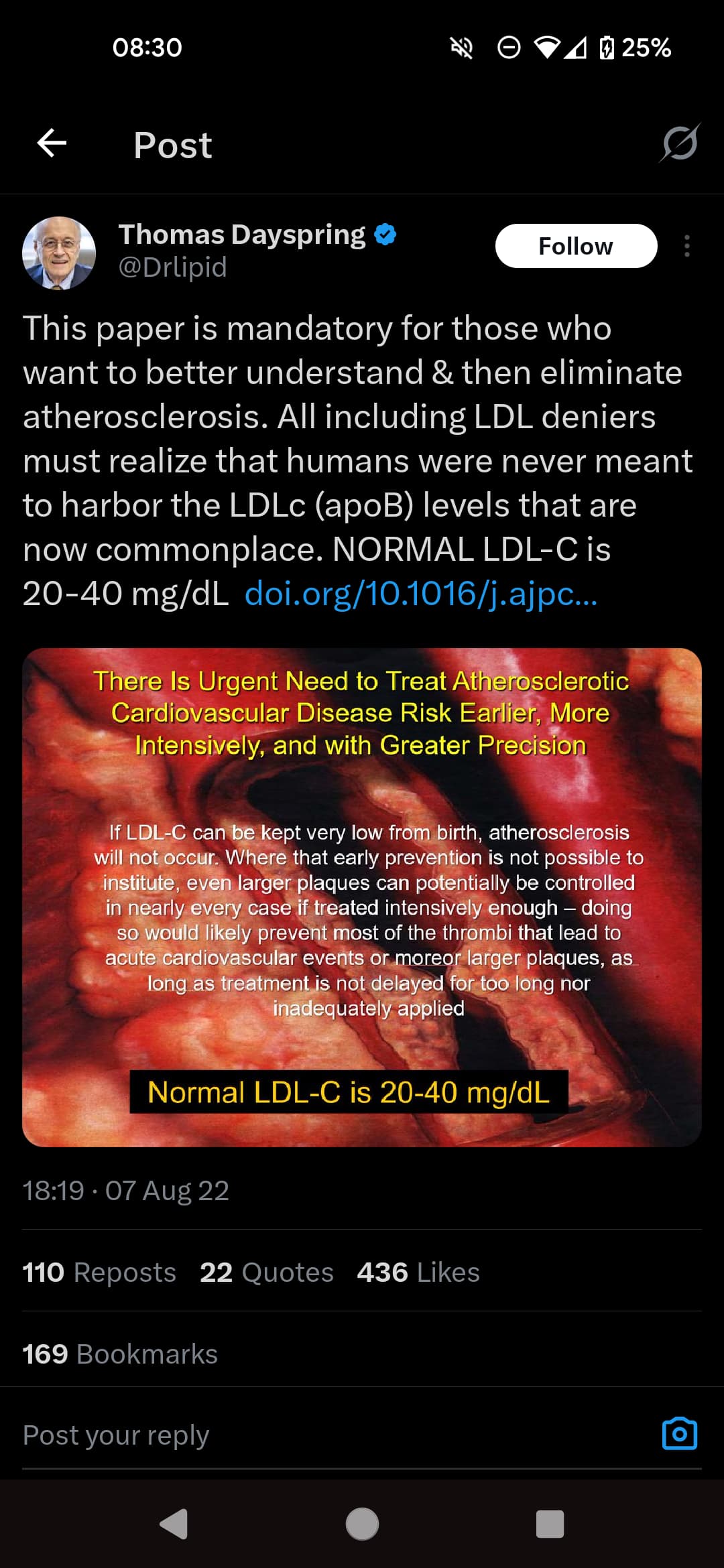
Thomas Dayspring also tweeted in favour of very low (20 to 40) quoting a paper which also misrepresented the hunter gatherer data. I think it’s notable that the data has been misquoted twice by two eminent academics.
Do you have a link to the paper? What is the mis-quote?
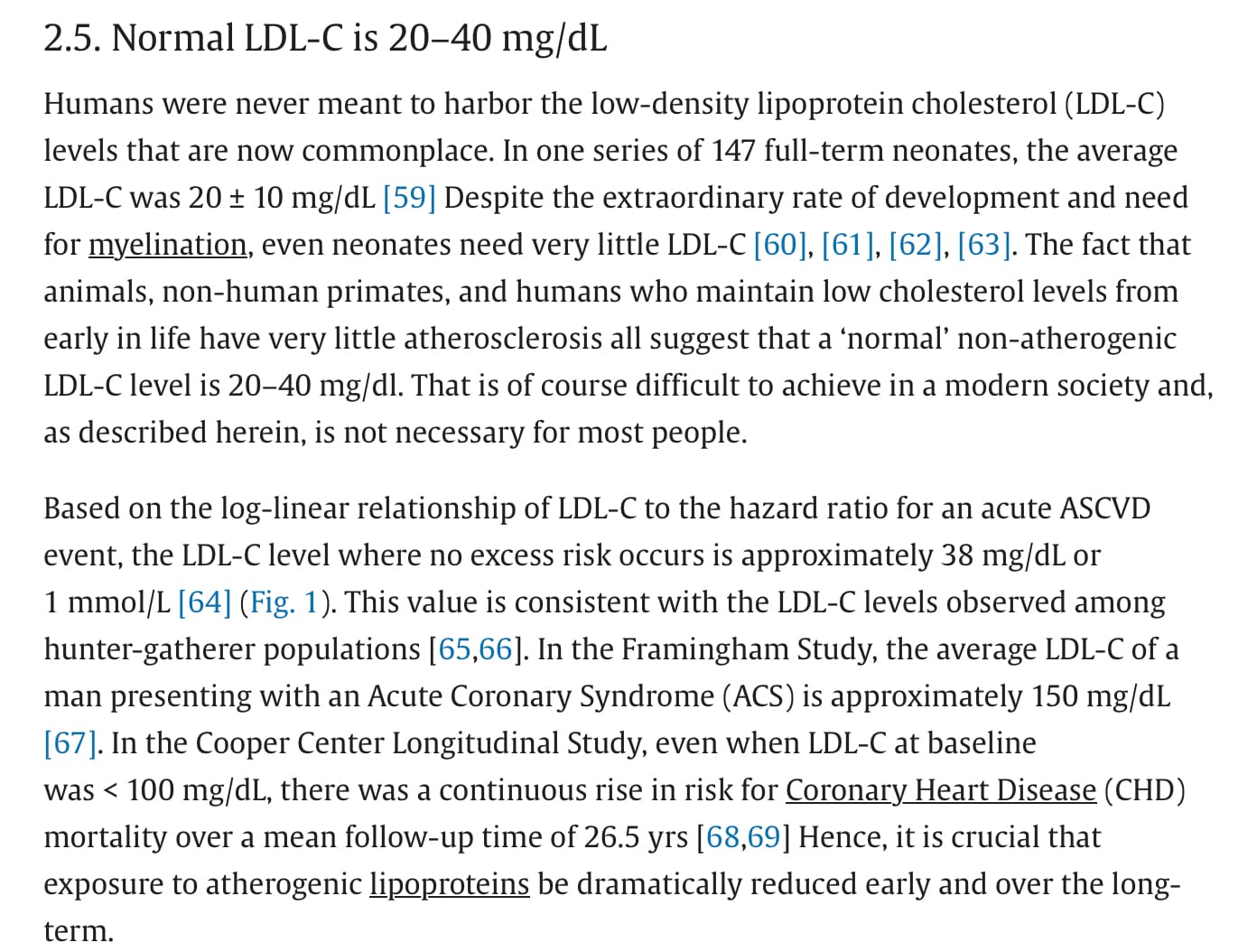
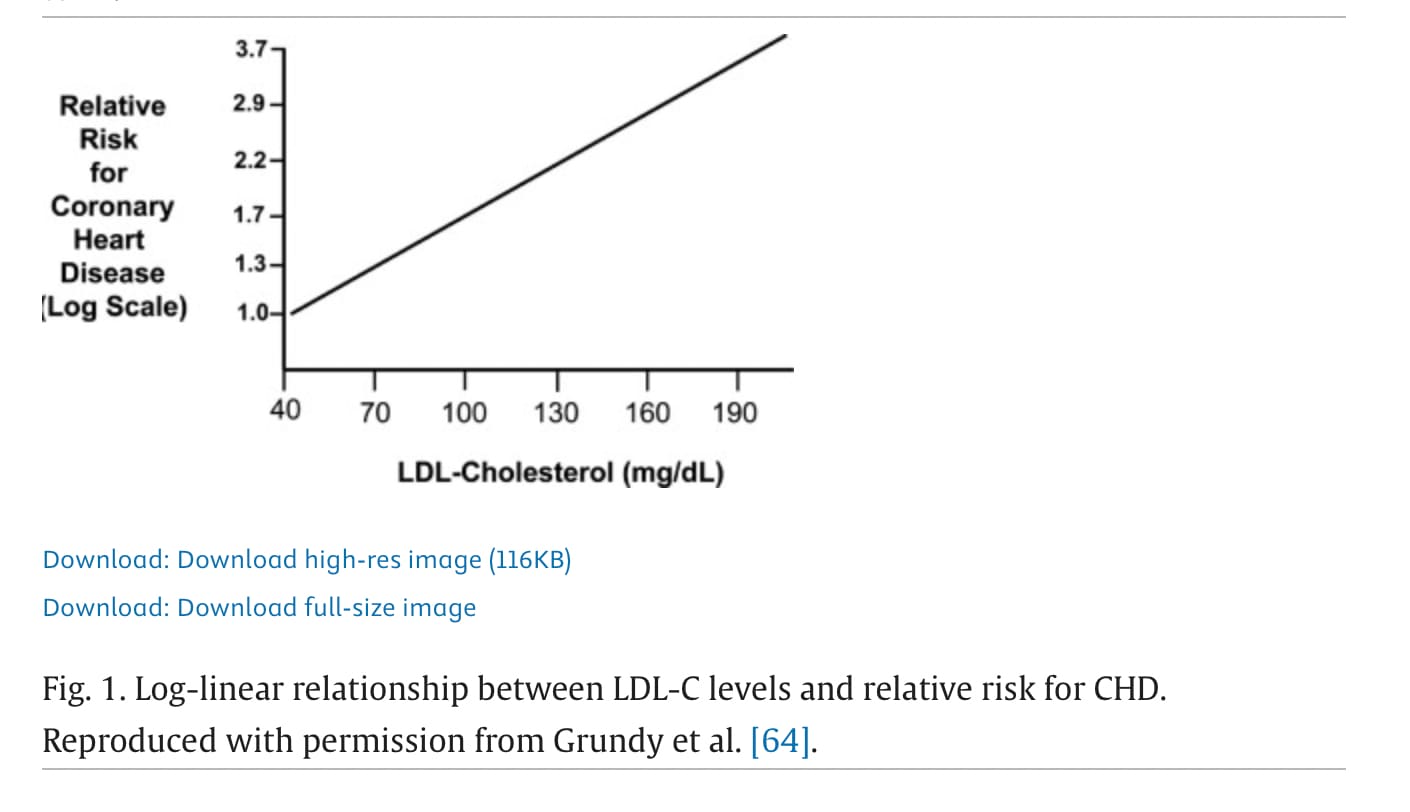
The paper stated:
“Based on the log-linear relationship of LDL-C to the hazard ratio for an acute ASCVD event, the LDL-C level where no excess risk occurs is approximately 38 mg/dL or 1 mmol/L [64] (Fig. 1). This value is consistent with the LDL-C levels observed among hunter-gatherer populations [65,66”
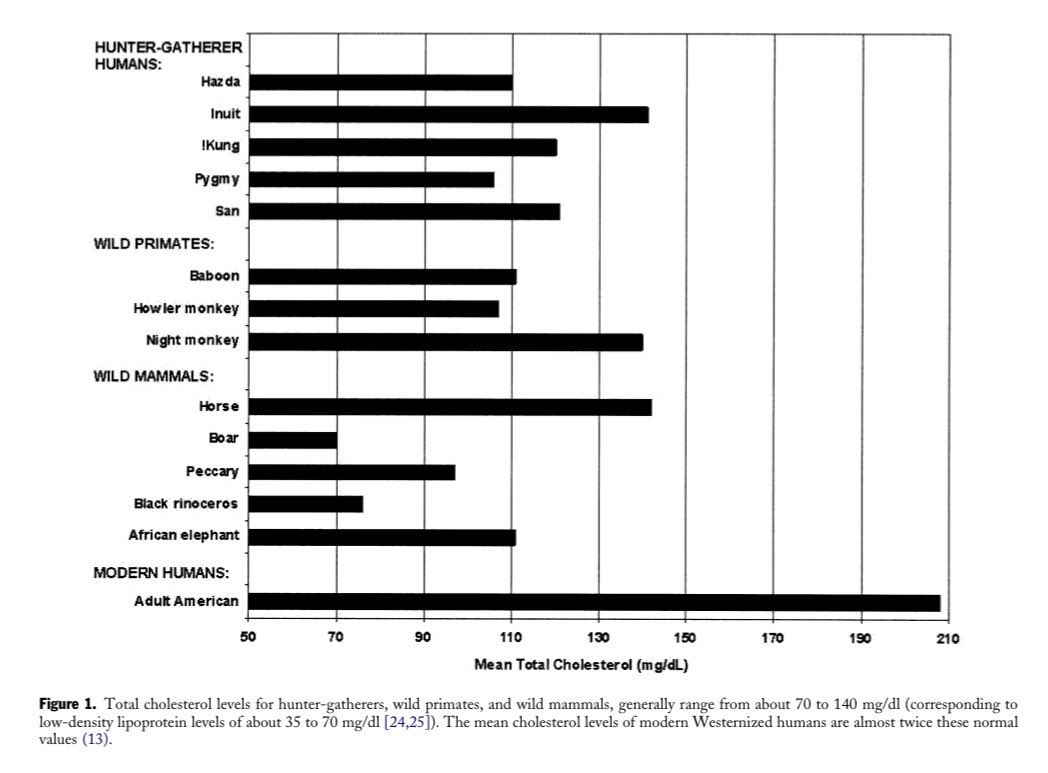
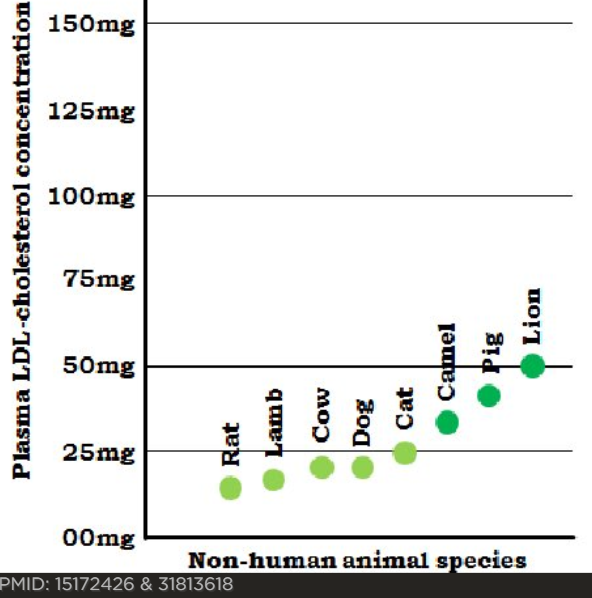
The hunter-gatherer data referenced was the graph I quoted above showing total cholesterol of 100 to 150 and interpreted by the authors as consistent “with estimated LDL cholesterol levels of about 50 to 75 mg/dl”
https://www.sciencedirect.com/science/article/pii/S2666667722000551?via%3Dihub
The temptation to misquote (fairly poor) hunter gatherer LDL data to support LDL below 50 is obviously quite strong
The Paper:
There is urgent need to treat atherosclerotic cardiovascular disease risk earlier, more intensively, and with greater precision: A review of current practice and recommendations for improved effectiveness
The full section:
In case anyone is interested in the underlying source of this graph, it’s from the paper linked below.
The data is from multiple studies which looked at cholesterol lowering interventions in elderly high risk or existing cvd subjects. So it suggests 38 LDL-C would eliminate cvd risk for secondary prevention or high risk elderly groups.
Implications of Recent Clinical Trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines
https://www.jacc.org/doi/full/10.1016/j.jacc.2004.07.001
In terms of primary prevention with no risk factors, the original paper (linked above) concludes:
“If LDL-C in blood is kept very low routinely – under 85 mg/dL for life, … atherosclerosis seems unlikely to occur to any clinically meaningful degree”
But I can’t find the data supporting such a relatively high level either🙂.
As with all these things I tend to reach for a tin of sardines when the data is inconclusive…
This is a very nice yt video of a doctor who experimented with a bunch of statins and dosages, combo with ezetimibe and he showed his bloodwork, lipids including Lp(a), glucose measures, insulin, inflammation and so on.
Doctor Reveals: My FULL Bloodworkon statins (+side effects etc) via Nutrition Made Simple!
Good and enjoyable. Gil probably confused pitavastatin with pravastatin at the end, it’s really not that much less potent – moderate intensity at max 4 mg dose, which should be more potent than his current 5 mg rosuvastatin. It’s actually the most potent statin, just that 4 mg is the maximum dose.
A disturbing must-see video for statin users such as myself.
# Statins Slash GLP-1 Levels: Human Controlled Trial
The same people who take this guy seriously also believe that cancer has been cured every time a popsci article says that X cures cancer because it worked in a petri dish.
It’s a real issue. Obicetrapib + ezetimibe will solve that problem.
Please - if anyone is posting a video now, include an AI summary (from here or other… Krisp | Free Youtube Video Summarizer with AI
Introduction to Statins and GLP-1 Levels
- The discussion begins with the speaker expressing a mix of excitement and annoyance regarding a recent scientific paper on statins, which are the most profitable drugs globally, generating over 20 billion dollars in annual sales.
- This paper highlights the role of statins in contributing to insulin resistance, increasing the risk of type 2 diabetes, and significantly lowering GLP-1 levels in humans.
- While the link between statins and insulin resistance is known, the impact on GLP-1 levels was previously unrecognized, raising concerns about the implications for current popular GLP-1 receptor agonists used for weight loss.
Lack of Awareness in the Medical Community
- The speaker expresses frustration that the findings of this important study, published in Cell Metabolism, did not gain the attention they deserved within the medical community or among the general public.
- During clinical rotations at Harvard Medical School, the speaker found that even among physicians, there was a significant lack of knowledge about the effects of statins on GLP-1 levels.
- In an informal poll of 12 physicians, including cardiologists, seven were unaware of the effects of statins on GLP-1 levels, highlighting a concerning gap in medical education and awareness.
Study Overview and Key Findings
- The study involved 30 patients starting treatment with Torvastatin, a common statin, alongside 10 control patients not on statins, followed for 16 weeks.
- Results indicated a significant increase in HbA1c levels, insulin levels, and insulin resistance in patients taking statins, along with a nearly 50% reduction in GLP-1 levels by the end of the trial.
- The speaker emphasizes that these findings should have been widely publicized, given the potential health implications for patients on statins.
Mechanism of Action: Statins and Gut Microbiome
- The research further explored how statins affect the gut microbiome, discovering that statin treatment altered the microbiome in a way that reduced the production of beneficial bile acids.
- A specific bile acid, ursodeoxycholic acid (UDCA), was found to be significantly reduced in patients taking statins due to the depletion of certain gut bacteria, notably Clostridium species.
- This depletion disrupted bile acid metabolism, leading to downstream effects including insulin resistance and decreased GLP-1 production.
Animal Model Confirmation
- To confirm the causative relationship, researchers conducted experiments on mice, which also exhibited insulin resistance and reduced GLP-1 levels when given statins.
- Transplanting microbiomes from statin-treated humans to non-statin-treated mice resulted in worsened insulin resistance, demonstrating the impact of the altered microbiome.
- Reintroducing the depleted Clostridium species or supplementing with UDCA reversed the metabolic damage, improving glucose metabolism and restoring GLP-1 levels.
Human Pilot Trial with UDCA
- A small pilot trial was conducted with five patients on statins for at least six months, who were given daily doses of UDCA at 500 milligrams.
- The results mirrored those observed in the mouse studies, showing significant improvements in blood sugar levels, insulin levels, insulin resistance, and restoration of GLP-1 levels.
- These findings suggest a potential simple and inexpensive solution to mitigate the negative effects of statins on metabolic health.
Broader Implications and Call to Action
- The speaker reflects on the deeper implications of the research, expressing concern about how the healthcare system often prioritizes profit over patient well-being, leading to gaps in patient care.
- The lack of discussion around simple and effective solutions, such as the use of UDCA, raises questions about the incentives driving medical practices and education.
- The speaker urges patients and clinicians to engage in conversations about these findings, share information, and advocate for better patient care and education in medical settings.
Conclusion and Recommendations
- The speaker concludes with a call to action for patients to share the information from the study and for clinicians to read the research and discuss its implications within their practices.
- The emphasis is placed on the importance of staying informed and questioning existing medical practices to better serve patient health.
- The overall message stresses the need for improvement in healthcare systems to prioritize patient outcomes over profit-driven motives.
He has credentials: a PhD in Human Metabolism at Oxford and an MD from Harvard.
I will take his opinion any day over yours. What are your credentials?
At no point did he suggest that people should stop taking statins.
Your main contribution seems to be trolling.
I take statins and rapamycin, both of which raise my A1C, and I can’t tolerate metformin.
So, yes, I am going to take TUDCA for at least 30 days and monitor what it does to my fasting glucose levels and A1C.
Can we move these discussions somewhere else than the flozin thread? We have a UDCA & TUDCA thread by the way: UDCA (ursodiol) / TUDCA for healthspan and lifespan?