Nature doesn’t want for anything, death being a thing simply evolved by accident and turned out to be a good thing for a species as a whole but bad for the individual.
If you care about the species, don’t do anything and simply accept death.
That is a good question.
“In the ASPREE trial, which included 12,334 healthy older adults (mean age 75.2 years) not taking lipid-lowering medications, the mean LDL-C levels were 3.2 mmol/L (~124 mg/dL) for men and 3.4 mmol/L (~131 mg/dL) for women1. This suggests that naturally low LDL-C (<70 mg/dL or <1.8 mmol/L) is uncommon in this group without disease.”
While very low LDL-C (<40 mg/dL) is rare in healthy older adults, studies like NHANES found that such levels were associated with higher mortality, possibly due to undiagnosed conditions (e.g., cancer, infections)
Are there arguments against “lower is better” other than association studies? Mendelian randomizations, RCTs, mechanistic understanding and neonatal analogy all points towards “lower is better”. By the way, association studies always look at LDL, not ApoB.
There is an argument in terms of Homo Sapiens that the species is not procreating to maintain a constant population (at least in some countries)
There is, however, a debate to be had as to what extent evolution actually selects for a mean lifespan. I think the evidence that it does in some species is very clear. I hence conclude that it does in all species.
Additionally I am of the view that the mechanism of the aging and development clock are essentially the same.
Some species like naked mole rats never seem to age at all and the only reason they die is because they all kill each other.
I did a post looking at these sort of things.
I really hate to disagree with Antoine here, but having done a ton of reading (and never ending!) on this topic, I think the story of statins, LDL and PD is very complicated, and should not be simply seen as “low LDL is a risk factor for PD”. I’m still researching this, but there are so many factors that it’s truly a murky picture. There is the timing issue - usage and dosage of statins before onset of PD symptoms, early stage, late stage, the variety of presentations of PD (it is a very heterogenous condition), the complication of other conditions like blood pressure and the reasons for it interacting, and finally - I hate to say it again - but the particular statin, beyond just lipophilic or hydrophilic, including pitavastatin, the role of statins in the integrity of BBB and possible impact of LPS crossing it, and so on. I have to say, I do a lot of reading about human physiology and pathology, but PD has really humbled me - it is the most difficult condition I have come across in trying to understand and so I am very, very, very, careful in reaching firm conclusions like “low LDL risk for PD”. I say this because people should be careful in making decisions about lowering LDL in particular with statins because they are concerned with PD - in my opinion it’s too complicated a situation to just reject statins based on that factor alone. YMMV.
PD is too complex to be discussed here but we have Mendelian randomization, association studies, RCT and mechanistic understanding against statins in PD. On the other hand for Lewy body dementia (and therefore PD dementia?), lower seems to be better. That’s why I chose to lower my LDL/ApoB with ezetimibe only. Let’s continue the PD discussion in the PD thread if needed.
And I forgot to mention that even though I think that statins are bad for PD… They still reduce mortality among people with Parkinson’s disease! See: https://www.neurology.org/doi/10.1212/WNL.0000000000213783
Because if you have PD, you don’t die from PD but from a heart attach like everyone else so statins will still save your life, even though they might worsen your PD symptoms.
A point about C is that in the cell it comes mainly from acetyl-CoA. Hence if the cell needs c then it will call on cytosolic levels of acetyl-CoA. That obviously can be problematic.
That’s true for all cholesterol and not just ApoB? So if you use something like obicetrapib that essentially keeps total cholesterol constant by lowering LDL and increasing HDL then you’re neutral?
It’s about cholesterol in the cell. I have not tried to find out how the different transports compare.
I wouldn’t be so quick to assume moderate/high LDL and ApoB are fine. This is simply a bit of evidence to the contrary. Most evidence points to getting LDL and ApoB low being good.
The fact is these numbers raise as you get older. Getting them low when you’re younger is a good thing.
It’s the same with body fat. Yes being too lean is a problem, but as you get older it becomes harder and harder to lose that stubborn fat.
Same with muscle. Too much muscle can be bad, but the odds that you build too much without steroids is unlikely and as you get older you’ll almost certainly not have too much.
This is the first I’ve ever heard of this outside of the carnivore/keto community. These people are justifying the results they get to fit the results their diets give them.
Also if you’re worried about statins try some other things like citrus bergamot, d-limonene, berberine, psyllium husk. Simple cheap OTC supplements. Try for 3-6 months and retest.
I take these, and also tirzepatide. I have insanely low ApoB and LDL. No cholesterol meds. To the point where I feel comfortable eating a bit more animal fat and total calories in my diet, what a luxury!
“Tirzepatide induced clinically meaningful reductions in the levels of systolic and diastolic blood pressure, total cholesterol, LDL cholesterol and triglycerides, along with increases in the level of HDL cholesterol.” - Effect of tirzepatide on blood pressure and lipids: A meta-analysis of randomized controlled trials https://pubmed.ncbi.nlm.nih.gov/37700437/
Its not conclusive, hence my “may” but:
“High levels of total cholesterol (TC) and LDL (low-density lipoprotein) cholesterol (LDL-C) are both associated with an increased risk of ischemic stroke, whereas low levels are associated with an increased risk of intracerebral hemorrhage.”
https://www.ahajournals.org/doi/10.1161/STROKEAHA.118.023167#:~:text=High%20levels%20of%20total%20cholesterol,increased%20risk%20of%20intracerebral%20hemorrhage.
"One long-term study found a link between very low LDL cholesterol and a higher risk of hemorrhagic stroke. More long-term data is needed to know about safety.
Many studies have shown that having lower than average total and LDL cholesterol is healthy."
Cholesterol level: Can it be too low? - Mayo Clinic.
I agree the PD risk/impact is low. My take, fwiw is that 50 to 70 apoB is a reasonable zone to be in if you have no other risk factors and inflammation is essentially under control but still want a long healthspan. The mendelian randomization studies have inherent limitations not least they can’t really provide full evidence on favour of a pharmaceutical intervention. But from memory the weight of evidence was they point towards psk9i as a better way to reduce apoB below 50 (vs statins) if that’s one’s objective.
In this uncut conversation, I sit down with Dr. Thomas Dayspring and Dr. Dan Soffer, two of the most respected voices in preventive cardiology, to break down the results of my own CT angiogram and CACS score. This is the full, uninterrupted version of the conversation featured in a recent episode. We unpack what my scan revealed, why cardiovascular disease can develop even in people with great bloodwork, and how to truly assess and manage risk beyond just a basic lipid panel. This is a practical, science-rich discussion that could change the way you think about heart health. What we cover:
- What my scan results actually mean
- The science of plaque development and risk thresholds
- Why good cholesterol numbers don’t tell the full story
- Advanced lipid testing: ApoB, Lp(a), and other biomarkers
- Statins, safety, and when to consider medication
- Misconceptions about diet and cholesterol
- The power of lifestyle change and early intervention
If you’ve ever wondered what’s really going on inside your arteries or how to protect your long-term cardiovascular health, this is an essential listen.
- Intro and Why This Episode Matters (00:00:00)
- Simon’s CT Angiogram: Early Heart Disease at 39 (00:02:03)
- What the Calcium Score Misses (00:04:47)
- Understanding Soft Plaque and ApoB Risk (00:09:05)
- Why LDL-C Isn’t the Full Story (00:12:30)
- Discordance Between Lipid Markers (00:17:42)
- Statin Decisions and Individual Risk Factors (00:23:20)
- How Much Plaque Is Concerning? (00:26:15)
- Lifestyle Changes That Make a Difference (00:32:11)
- Imaging vs Blood Markers: Which to Trust? (00:36:24)
- Preventive Screening: Who Should Get a CT Angiogram? (00:42:01)
- Why Younger Adults Should Take Action (00:47:18)
- Final Reflections and Long-Term Prevention (00:52:09)
This is a 2019 paper citing a 2007 study. However it seems confirmed by more recent studies: https://www.sciencedirect.com/science/article/abs/pii/S0014299925001979
This paper suggests that LDL < 70 mg/dL is the threshold: https://www.neurology.org/doi/abs/10.1212/WNL.0000000000007853
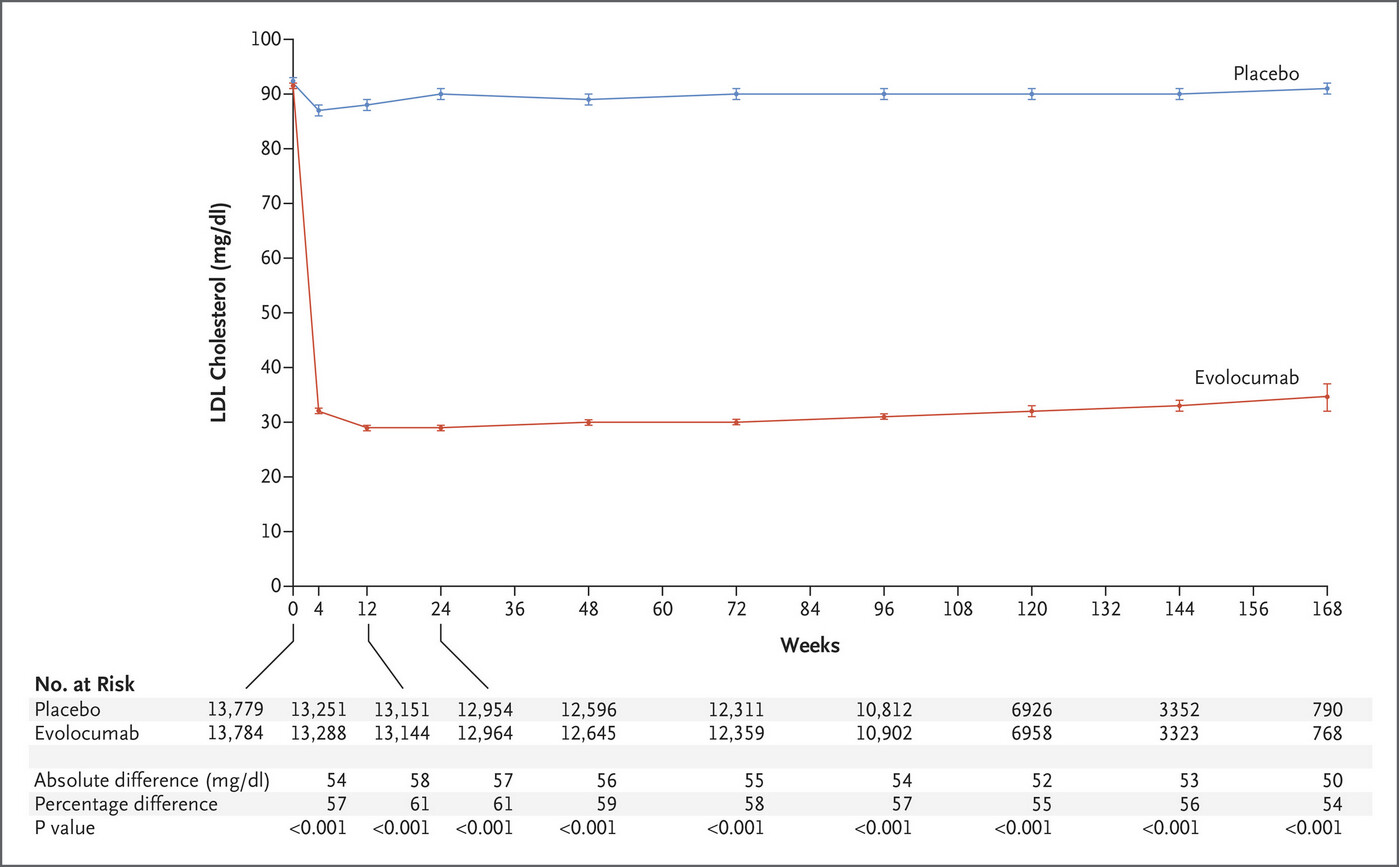
Vytorin Efficacy International Trial (IMPROVE-IT) lowered LDL cholesterol levels from 70 mg per deciliter (1.8 mmol per liter) to 54 mg per deciliter (1.4 mmol per liter) and significantly reduced major cardiovascular events.
Specifically, there was a 17% reduction in the risk of the key secondary end point among patients in the top quartile for baseline LDL cholesterol level, in whom evolocumab lowered the median LDL cholesterol level from 126 mg per deciliter (3.3 mmol per liter) to 43 mg per deciliter (1.1 mmol per liter) (with the achieved level similar to that achieved with ezetimibe in patients in the lowest quartile for admission LDL cholesterol levels in IMPROVE-IT16), and there was a 22% reduction in the risk of the key secondary end point** among the patients in the lowest quartile for baseline LDL cholesterol level, in whom evolocumab lowered the median LDL cholesterol level from 73 mg per deciliter (1.9 mmol per liter) to 22 mg per deciliter (0.57 mmol per liter). These observations align well with the effects of evolocumab on coronary atherosclerotic plaque volume in the Global Assessment of Plaque Regression with a PCSK9 Antibody as Measured by Intravascular Ultrasound (GLAGOV) trial17 and show that continued cardiovascular benefit can be accrued even when LDL cholesterol levels are reduced to 20 to 25 mg per deciliter (0.52 to 0.65 mmol per liter), a range that is well below current targets.
Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease
I agree. I think 50 should be the target not 70 for ApoB and LDL. Is there any evidence of benefit below 50? @A_User
Thomas Dayspring said the purpose of the cholesterol in LDL and VLDL is to give structure to the particles to make them spherical and a substantial amount of cholesterol in LDL was transported from HDL.
He also said VLDL is necessary for triglyceride and fat soluble vitamin transport but that apoB 30 mg per dl is enough for that.