Amen to that, plus add resveratrol and calcium to the list of overhyped sups.
Simon Hill has posted a followup video to the one above, this time doing a deep dive into his full blood test results including biological age. Not everyone who’s a health influencer is this transparent and I appreciate him doing this.
O3:
1. Tidied transcript (edited for readability, filler words and ad‑breaks removed)
Intro (0 – 2 min)
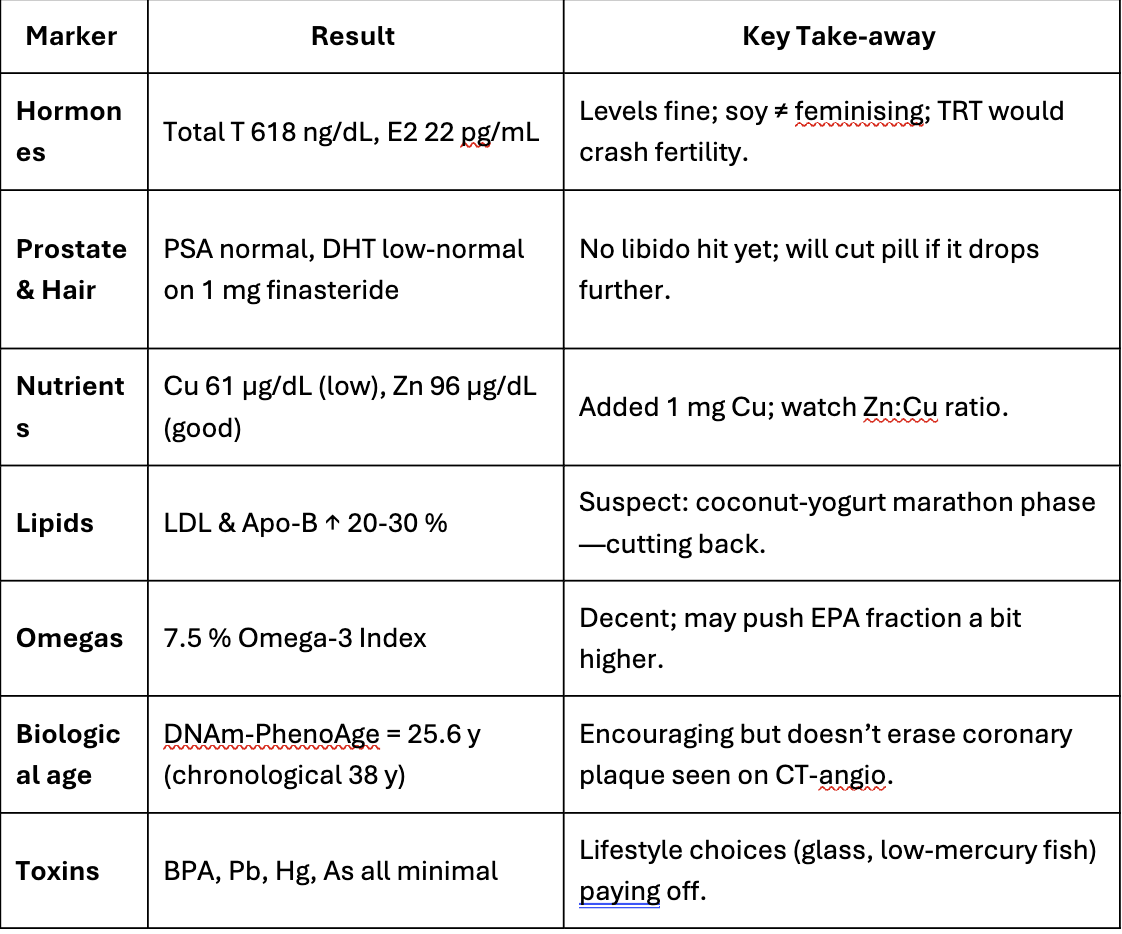
I’m starting to wonder if I’m oversharing. You already have my blood tests, sperm results, CT‑angiogram… and now you’re getting my biological‑age report. I just received a panel of 100‑plus biomarkers from Function Health and a few things jumped out, including one blind‑spot even I’d missed. I’m sharing the full results because data and transparency help us all—whether that means lifestyle tweaks, supplements, or a chat with your doctor.
What we’ll cover
- Hormones (testosterone, oestrogen, FSH, LH)
- Nutrient status (with one surprise deficiency)
- Thyroid health
- Cardio‑metabolic markers (Apo B, glucose) & environmental toxins
- My biological age (using Dr Morgan Levine’s PhenoAge clock)
Hormones & fertility (2 – 8 min)
- Estradiol‑2: 22 pg/mL—well inside the male range (10‑40). Soy doesn’t “feminise” men; meta‑analysis of 38 RCTs confirms no effect on testosterone or oestrogen.
- Total T: 618 ng/dL, free T: 108 pg/mL—both healthy. No need for testosterone‑replacement therapy (TRT) when levels and energy are good.
- HRT shuts down endogenous T and sperm production, risking infertility. My FSH (6.9 IU/L) and LH (4 IU/L) are normal, matching last year’s favourable semen analysis.
- Clip with urologist Dr Ramy Ghayda: exogenous testosterone often drives sperm count to zero; 15–20 % of men never recover testicular volume.
Prostate & DHT (8 – 14 min)
- PSA panel all normal.
- DHT low‑normal—expected, because I started 1 mg finasteride for hair‑loss. Side‑effect (reduced libido) hasn’t appeared; if DHT drops too much I’ll halve the dose.
Nutrient panel surprises (14 – 22 min)
- B‑12 (via MMA & homocysteine) and vitamin D (57 ng/mL) solid.
- Omega‑3 “omega‑check” 7.5 % (EPA 2.5 %, DHA 3.3 %, DPA 1.6 %).
- Iron: Hb 15.7 g/dL; ferritin 39 ng/mL (low‑normal) but saturation 44 %.
- Zinc good (96 µg/dL) but copper low (61 µg/dL). Likely linked to zinc supplementation competing for absorption; I’ve switched to a multi with 1 mg copper.
- Magnesium, iodine, selenium all fine.
Thyroid & cardio‑metabolic (22 – 25 min)
- TSH, free T3/T4 and antibodies normal.
- Glucose, insulin, HbA1c perfect; CRP very low.
- Weak spot: LDL‑C and Apo B up ~20–30 %—probably the coconut‑yoghurt phase while marathon‑training. I’m sensitive to lauric‑acid saturated fat.
Environmental toxins (25 – 27 min)
Aluminium, arsenic, BPA, lead, mercury all minimal; BPA undetectable.
Biological age (27 – 29 min)
DNAm‑PhenoAge estimate: 25.6 y— ≈13 y younger than my calendar age. Encouraging, but not a free pass; my CT‑angiogram shows early plaque, so LDL/Apo B remain priorities.
Take‑home messages (29 – 33 min)
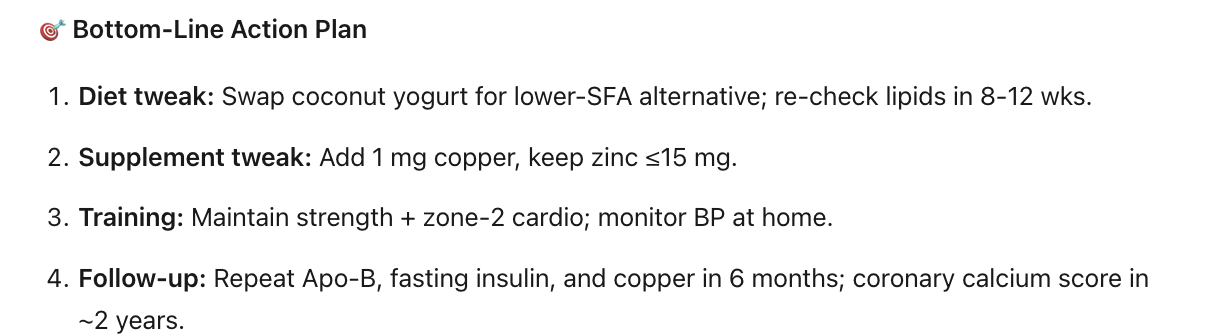
- Annual labs + regular blood‑pressure checks catch issues early.
- Health is dynamic; address weak links before they snowball.
- Grateful for the privilege of access—aim is to normalise preventive care.
(Full 33‑minute verbatim PDF is in Simon Hill’s show‑notes.)
### 2. Executive summary
- Overall the host, Simon Hill, reports broadly favourable bloodwork: robust sex‑hormone profile, strong nutrient status, excellent glycaemic control and inflammation, minimal toxin exposure, and a “younger” biological‑age score.
- Red flags: slightly elevated LDL‑C and Apo B—likely diet‑induced—and an unexpected copper deficit (possibly from excess zinc).
- Key interventions he plans: reduce coconut‑derived saturated fat, tweak omega‑3 dosing, add 1 mg copper, continue strength/endurance training, monitor labs and blood pressure.
- Educational points: clarifies myths around soy and hormones, cautions against indiscriminate TRT, highlights finasteride’s pros/cons, and stresses routine screening for silent risks like hypertension.
### 3. Critique
| Aspect | Strengths | Caveats / Limitations |
|---|---|---|
| Transparency & structure | Shares raw PDF, walks viewers marker‑by‑marker, explains physiology clearly. | Partnership with Function Health is disclosed but still a marketing tie‑in; viewers may conflate educational content with an ad. |
| Hormone discussion | Correctly notes that normal testosterone + good symptoms ≠ need for TRT; highlights fertility suppression with exogenous T—consistent with clinical reviews. (PMC) | Omits mention of alternative treatments (e.g., clomiphene, hCG) for symptomatic men who want fertility. |
| Finasteride segment | Gives real‑world DHT data; quotes sexual‑side‑effect prevalence (≈1.5–4 %). (PMC) | Underplays “post‑finasteride syndrome” reports; incidence is low but consequences can be severe and longer‑lasting in some cases. |
| Nutrient insights | Makes a useful point about zinc competing with copper and immediately adjusts supplementation. (Medsafe) | Copper measured once; without ceruloplasmin or repeat testing it’s hard to know if this is chronic or transient. |
| LDL/Apo B rise explanation | Correct that lauric acid (coconut fat) can raise LDL. (The Nutrition Source) | The claim that his spike is “20–30 % from coconut yogurt” is plausible but unverified without a controlled diet or repeat lipid panel. Other factors (training stress, weight change) not explored. |
| Biological‑age reporting | Uses Dr Levine’s DNAm PhenoAge clock and clarifies it’s research‑grade. (PMC) | PhenoAge is validated for population risk, not individual diagnosis; a 13‑year “bonus” can fluctuate several years between draws. May give false reassurance. |
| Take‑home advice | Emphasises affordable, high‑impact checks (blood pressure) and lifestyle before meds; balanced. | Cost of 160‑marker panels (~US $499/year) may be prohibitive; benefits over a standard evidence‑based panel are not discussed. |
Bottom line
Simon Hill delivers an engaging, largely evidence‑aligned walkthrough of his labs and uses them to illustrate practical preventive‑health principles. The episode shines in demystifying biomarkers and cautioning against trendy but unjustified interventions (e.g., elective TRT). Viewers should, however, remember:
- One lab snapshot is not destiny—repeat testing and clinical context matter.
- Biological‑age “clocks” are promising but still experimental; track trends, not single numbers.
- Comprehensive panels and devices marketed direct‑to‑consumer can be helpful if you understand their limits, but the essentials (blood pressure, lipids, HbA1c, kidney/liver panel) remain the highest‑yield for most people.
As always, interpret any abnormal result with a qualified clinician—not just a colourful dashboard.
Sources
(theproof.com, PMC, PMC, The Nutrition Source, PMC, Medsafe)
TL:DR from Kimi, a free Chinese AI agent
In one sentence: Simon’s numbers are solid, but LDL/Apo-B and copper need quick, cheap fixes; the flashy “biological age” is fun but not yet actionable medicine.
I had a CT Angiogram done in November 2024 which found 70% stenosis in my D2 Artery (all soft plaque, zero calcium score). Since then I have been following a protocol to try to stabilise and regress my plaque. At the end of this month I will be having a second CT Angiogram to see if there’s been any change.
Regardless of the outcome, I would like to have both scans reviewed by Cleerly AI (www.clearlyhealth.com). There aren’t any Cleerly providers in New Zealand, so I am hoping to get the raw CTA files from my Radiologist and send them to a Cleerly provider in the USA for analysis.
Two questions:
- Does this sound like something that can be done?
- If yes, are you able to recommend a Cleerly provider I should contact?
Many thanks!!
My understanding is that it’s always done that way. I was told my angio would be local and the CD could be mailed to them. They do a video call or something. I would use the one in Kansas City.
To feed the trolls a bit: Low apolipoprotein B and LDL-cholesterol are associated with the risk of cardiovascular and allcause mortality: a prospective cohort 2025
The study cohort had a median (IQR) age of 46.0 (32.0, 60.0) years, with 7949 (51.8%) males. During a median follow-up of 101.0 months (IQR: 67–137), 1771 (8.8%) all-cause mortality events were observed; 443 (2.1%) deaths were attributed to cardiovascular diseases, while 109 (0.5%) resulted from cerebrovascular diseases. Low apoB and LDL-cholesterol levels were independently linked to an elevated risk of all-cause and cardiovascular mortality. Compared with participants having apoB <90 mg/ dL and LDL-cholesterol levels between 100–129 mg/dL, those with LDL-cholesterol <70 mg/dL (HR, 1.81; 95%CI: 1.39–2.36) and 70–99 mg/dL (HR, 1.28; 95%CI: 1.01–1.62) demonstrated a higher risk of all-cause mortality. Additionally, reduced apoB levels contributed to an increased risk of cardiovascular mortality among individuals with low LDL-cholesterol levels.
It’s a Chinese paper from a random Chinese institution (People’s Hospital of Xinjiang Uyghur Autonomous Region), so low quality.
What the hell? Was about to order the needed meds to lower both even though have them both in higher normal range. What to believe now? people in here (and some other places) shooting for <60 or this study?
Exactly… lol.
My LDL - C is higher normal, but no sign of CVD.
Zero plaque.
Sometimes LDL - C is higher because your body is moving fat lipids out through the blood… like when on HGH.
It’s simple, you trust Western medicine and only start looking into Chinese medicine when it passes a phase 3 clinical trial in either Europe or the US.
This wasn’t about medicine though, we are talking about a cohort study.
I have looked and searched using several search engines and AI sites such as Consensus and the other usual suspects. My takeaway is that it is now clear that a very low LDL and APOB increase the risk of CVD, all-cause mortality, and strokes, especially among the elderly. The Chinese paper you cited is among many that draw the same conclusion.
This represents a summary of papers that I have looked at:
"A compelling and recurring theme in recent research is the observation of a “U-shaped” or “J-shaped” relationship between LDL-C levels and all-cause mortality. This pattern indicates that while very high LDL-C levels are associated with increased mortality risk, so too are extremely low levels, with the lowest risk typically found within an intermediate, often moderately low, range. This consistent demonstration of a U-shaped relationship across multiple large-scale studies fundamentally challenges the long-standing “lower is better” paradigm for LDL-C,"
I have purposely lowered my LDL and other lipids using statins, etc., based primarily on the opinions of doctors such as “Lipid” doctors found on YouTube, X, etc.
The results of my AI searches, as well as reading many of the papers they have produced, convince me that I have lowered my lipids too much through the use of statins.
So, I will stop using atorvastatin to lower my lipids and allow them to return to a more reasonable level.
These cohort studies do consistently show a j curve, but they are readily confounded.
Several significant diseases can cause low ldl-C and apob. So those individuals could easily skew the result.
That said, RCTs and mendelian randomization studies don’t provide any real evidence to support pushing lower than 50 apoB.
And given that the evidence suggests there is little benefit from lowering from 70 to 50 ApoB, I think its reasonable to be sanguine if your apoB is in that range.
That kind of studies is just 8 random dudes from People’s Hospital of Xinjiang Uyghur Autonomous Region playing with regression models on the NHANES data without any real understanding.
People should apply a common sense filter on that kind of “studies” and avoid flip-flopping on what they do just because they see something new.
Those ACM correlations with low LDL vanish when other confounders, like nutrition status and HDL, are taken into account. Low APO-B and LDL by themselves are not enough as there are plenty of bad reasons to have a low LDL.
Thanks for triggering me @adssx ! ![]() I generally try to ignore that kind of stuff.
I generally try to ignore that kind of stuff.
People desperately want to cling to the argument that because high cholesterol is natural, it must be good. But when it comes to cancer that is suddenly bad again.
Because at that level you’ll likely be accumulating soft plaque at a rate that will kill you in your 60s-90s. 20mg pravastatin by itself should bring you below the critical level, you don’t need ezetimibe. And it is one of the safest and best tolerated statins in all aspects.
This has been posted in another thread awhile back, but because there’s been a discussion of the possibility that statins might be longevity enhancing, based on the UK Biobank data and other data sources, I thought it makes sense to post it in the cardiovascular health thread.
A couple of interesting things. The mortality risk reduction was similar in CVD and non-CVD studies. So statins have a positive impact not just on the CV system - at perhaps the cost of other systems - it’s across the board. And this was true of populations with very different diseases as well.
Personally, I take pitavastatin because I have high LDL, ApoB and extremely high Lp(a) (though my CAC score at age 65 was zero). However, I would’ve been taking a statin even if my lipid numbers were within norm, because I believe statins - if your personal physiology tolerates them - have significant pleiotropic benefits, based on my extensive reading of the literature, That said, I think there are better and not as good statins, and you need to match the statin to your situation. For me, it was pitavastatin.
My goal is LDL below 60 mg/dL though below 70 would be acceptable. I don’t see the need to go below 55 for me.
Effect of Statins on All-Cause Mortality in Adults: A Systematic Review and Meta-Analysis of Propensity Score-Matched Studies
It is also important to note that atorvastatin in the ITP did not statistically significantly affect lifespan one way or another, indicating that the mechanistic drawbacks from it are not materializing in real organisms.
I think the ITP tested simvastatin, not atorvastatin. This is why I say it’s important to focus not just on class effects, but individual statins. Atorvastatin was found to have a 10% postive effect on the UK Biobank data study.
I prefer pitavastatin for both personal physiological reasons and general assessment of statins. I am pre-diabetic, so I have issues with glucose control. One of the negative side effects of statins that I personally find worrisome is that they can cause diabetes - this is true for atorvastatin, and glucose control is also an issue with rosuvastatin. Pitavastatin on the other hand, has not been associated with diabetes, or causing elevated blood sugar. So for me, pitavastatin is an obvious choice for that reason alone. However, another reason is that I am a big believer in carefully curated polypharmacy - as I don’t believe you can significantly affect aging or health in general with just one single pill - and pitavastatin is metabolized by a different class of enzymes than other statins like for example atorvastatin, which means that pitavastatin has very few interactions with other drugs - important if you are into polypharmacy. Incidentally, it also means that it interacts less with food - so for example pitavastatin is not affected by grapefruit juice, while atorvastatin is.
But apart from personal physiological reasons, pitavastatin just is a fantastic statin compared to the others. I don’t have time to re-post all the studies for the following claims, but do a search of this site for “pitavastatin” and you’ll find a lot of my posts. It prevents MACE just about better than any other statin. It protects the BBB, preventing LPS from crossing - I posted a paper to that effect. It elevates HDL which can be important to those vulnerable to the metabolic syndrome. It has much lower side effects on the muscles and joints compared to other statins and doesn’t nuke your CoQ10. And much more - do a search. Limitations - there are always limitations - although it is perhaps the most powerful statin by mg, it is prescribed only in low-medium dose 1-2 and 4mg - that may not be enough for someone who is looking for a high-intensity statin (8mg has been used, but not in the US or Europe); also, compared to atorvastatin or rosuvastatin, it doesn’t have quite as many studies as it’s been more popularly used in Japan and the East (S. Korea, Taiwan etc.). OK, I’ll throw you one study I’ve posted before, just to get you started:
Position paper of the Polish Expert Group on the use of pitavastatin in the treatment of lipid disorders in Poland endorsed by the Polish Lipid Association
Ezetimibe - nothing wrong with it. I use it personally. Rosuvastatin, I’m not a fan of compared to pitavastatin, but YMMV, if you need a statin, rosuvastatin is fine.