Yeah I follow him and agree with him on most things except high hematocrit. I’d be concerned that the increased risk of thrombosis from oral estrogen would offset or even have a net detrimental effect when weighed against a 40% decrease in Lp(a).
Sorry, I did not respond earlier.
You can find many medical papers, especially ones two years or older, here for free.
https://sci-hub.se/
“Sci-Hub has the largest (> 88 million documents) database of full-text scientific papers, available for free. Approximately 80% of the collection are articles from scientific journals, most of them dedicated to the subject of medicine. That is followed by physics, chemistry and biology, humanities, etc. The entire collection is available for download on the torrent network, and takes up about 100 terabytes of space.”
Amazingly, you can download the entire collection if you have the time and space.
Sorry, here is the paper you paid for.
“https://sci-hub.se/https://pubmed.ncbi.nlm.nih.gov/9150696/”
A great paper.
Thanks for sharing… I have been on HGH for nine months to rebuild the thymus…
RapAdmin found and posted where rapamycin does similar thymus regeneration in a female mouse study.
CAD prevention and benefits on top would be fantastic.
I’m familiar w/sci-hub and have used it many times. They have the 1997 paper (the one you linked to) but not the 2023 paper, which is the one I paid for and posted above.
Emily Latella, says sorry!
Interesting David… I am getting a Coronary Calcium Scan in January 2026. Will see if anything has changed.
The designer cytokine IC7Fc attenuates atherosclerosis development by targeting hyperlipidemia in mice
https://www.science.org/doi/10.1126/sciadv.adx3794
Designer drug targets both heart disease and diabetes
Anecdotally, I have checked Lp(a) on HGH and without HGH and there isn’t much of a difference. I’m fortunate enough to have a low level either way though.
Just sharing this article about a study that shows exposure to light at night might increase heart attacks. It was just in Jama 10/25
The study
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2840489
Back in 2005 (age 49) I was diagnosed with a coronary artery spasm via angiogram. It was in the artery next to the widow maker so I got lucky. That artery had about 60% blockage as well so they did not insert a stent. Apparently various type of stress can cause this, physical and emotional. At that time my “emotional” stress was through the roof.
Side note, 6 weeks after that, I went on a solo 2 day motorcycle ride covering 1,000 km. It was not a slow ride, life begins at 200km/hr is my philosophy. My wife asked the logical question, why? It will either set me free or kill me, was my reply and it set me free from the emotional roller coaster I had been on.
In 2013 I was having pain in my left arm, went to a cardiologist and did the tests and he gave my heart a clean bill of health, had no idea what the pain was. Six months later it was diagnosed as a referred pain from a injury to my ininfraspinatus, took a year to work that out but all good ever since.
2025, July my PCP asked when the last time I’d been to a Cardiologist and she then referred me to one as a precaution for this old guy.
I have no symptoms, no shortness of breath, no chest pains, I’m a fully functioning, hard working, old guy LoL! she loves to refer me to specialists!
July did a stress test with ultrasound. 2 dark spots were detected, 4 months later a repeat test, only 1 dark spot, Apparently ultrasound imaging is not the best option for this type of imaging as it provided 1 false positive. Oct 27 I was sent for a nuclear heart scan. That came back with a definitive blockage that the radiologist deemed to be medium to high risk.
Nov 3 went for an angiogram. Three possible outcomes 1) nothing needs to be done, 2) insert a stent, 3) by-pass surgery
Was pretty cool watching the process, at one point they pulled the dye thingy out and inserted something that vibrated (later identified as the drill thingy), then pulled that out and reinserted the dye thingy ![]() don’t mind the highly technical description of the process,
don’t mind the highly technical description of the process,
Diagnosis was a CTO, chronic total obstruction. With collateral circulation or arteriogenesis that was basically a “fix” my body was providing. There are levels to this and mine is pretty high as I do not have any of the symptoms that poor collateral regrowth provides.
I attrite this to more good luck, good genes and my last 2 years of peptide therapy, specifically daily BPC 157 + TB500 (aa43) to keep my old body primed to heal. Both these peptides support arteriogenisis.
And of course the 1000km ride at speed ![]()
New from Christine Glorioso. A really good story:
The discovery of PCSK9’s role began in 2003 when researchers identified gain-of-function mutations in the PCSK9 gene in French families with familial hypercholesterolemia, a condition that causes dangerously high cholesterol from birth. Shortly after, scientists discovered the flip side: people with loss-of-function mutations in PCSK9 had remarkably low LDL cholesterol and dramatically reduced cardiovascular disease risk.
In one landmark 2006 study, participants with these protective mutations had 28% lower LDL cholesterol and an 88% reduction in cardiovascular disease risk.
This genetic evidence was so compelling that it launched a pharmaceutical race to inhibit PCSK9- and remarkably, the first drugs were approved just 12 years after the initial discovery.
PCSK9 Inhibitors prevent PCSK9 from doing its job, which in turn increases the number of receptors available to clear cholesterol, lowering LDL levels. Statins work through different mechanisms by inhibiting HMG CoA reductase as well as other effects. Together the two classes of drugs are synergistic when used in combination.
The PCSK9 longevity gene- therapeutics, heart health, brain health, and supplements
There are some oral PCSK9I drugs under development. I’m looking forward to these as injections are inconvenient.
Enlicitide decanoate (MK-0616), developed by Merck, is a promising oral macrocyclic peptide that has shown significant LDL-C reduction in Phase IIb trials and is currently in Phase III clinical development.
AZD0780 is another oral small molecule PCSK9 inhibitor in Phase II trials that has demonstrated robust efficacy in lowering LDL cholesterol levels.
Other oral candidates, such as DC371739 and CVI-LM001, are also being investigated in earlier phase clinical trials.
The question is, with an APOB of 58, is there any reason to use a PCSK9I to lower it further? Or replace the statin? (5 mg Atorvastatin)
Great news that it was sorted! CTO is not the worst thing, since at least it was stable. But that’s definitely a warning sign of a tendency to build plaque.
I assume they gave you medication to take? (Plavix?)
And dare I ask - how are the blood lipids now?
AI Summary:
Biological Age and Cardiovascular Disease Risk
- In 2025, the speaker’s biological age was calculated to be 35.4 years, which is 17 years younger than their chronological age.
- The biological age clock, known as pheno age, has its limitations, particularly in its exclusion of cardiovascular disease biomarkers.
- Despite this limitation, pheno age is still significantly associated with cardiovascular disease-related mortality, showing a 10% increased risk of death for every one-year increase in biological age.
- The speaker intends to analyze their blood test data over the past decade, particularly focusing on cardiovascular disease biomarkers.
Blood Testing Process
- The speaker uses altabtest.com to select specific blood tests, which are then processed at Quest Diagnostics.
- Results are typically received within five days of testing, allowing for timely analysis.
- The speaker emphasizes the importance of frequent testing, averaging six times per year to gather more accurate data over time.
Lipid Panel and HDL Analysis
- The speaker’s HDL level was measured at 60 milligrams per deciliter, which falls within the optimal range of 50 to 69 milligrams per deciliter.
- Cumulative testing shows that the speaker has maintained an average HDL level of 58 milligrams per deciliter over 19 tests spanning three years.
- The speaker previously averaged 45 milligrams per deciliter over 44 tests, indicating a significant improvement in HDL levels.
- APO A1 is noted as a potentially better predictor of cardiovascular disease mortality risk, and the speaker has been monitoring this biomarker as well.
APO A1 Measurement
- The reference range for APO A1 is above 115 milligrams per deciliter, with an optimal range suggested to be between 150 and 180 milligrams per deciliter.
- The speaker’s current APO A1 levels are flagged with an orange arrow, indicating they are below the optimal target.
- A strong correlation (0.95) between APO A1 and HDL levels in the speaker’s data suggests that measuring both may not be necessary.
- The speaker aims to achieve an optimal HDL level of around 67 milligrams per deciliter to simultaneously optimize both biomarkers.
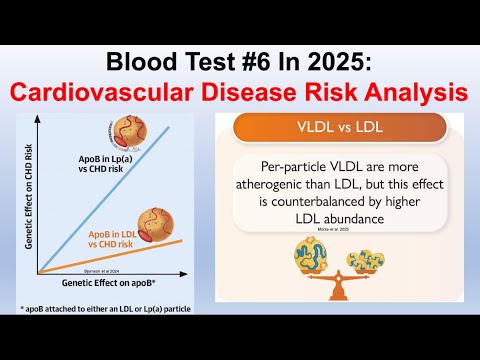
Lipoprotein Analysis
- The speaker discusses the importance of lipoproteins containing APO B, including VLDL, lipoprotein A, and LDL, in assessing cardiovascular risk.
- APO B levels below 90 milligrams per deciliter are considered good, with less than 70 being optimal, particularly for those without pre-existing conditions.
- The speaker’s APO B level was measured at 59 milligrams per deciliter, which is favorable according to their interpretation of the literature.
- The speaker emphasizes that diet and exercise, rather than medication, have contributed to their favorable APO B levels.
Lipoprotein A and Cardiovascular Risk
- Lipoprotein A levels for the speaker were measured at 81 nanomoles, which is outside the normal range, indicating a potential risk factor for cardiovascular disease.
- The speaker has a history of variable lipoprotein A levels, with past results ranging from 70 to 145 nanomoles.
- The speaker notes that lipoprotein A is resistant to reduction, but they are working on finding effective methods to lower it.
- High-sensitivity C-reactive protein (hsCRP) levels were significantly lower than the threshold associated with increased cardiovascular disease risk, suggesting a favorable outcome.
Triglycerides and VLDL
- The speaker’s triglyceride level was measured at 78 milligrams per deciliter, which is within a generally acceptable range but higher than their optimal target of less than 45 milligrams per deciliter.
- Over 63 tests in the past decade, the speaker’s average triglycerides were 60 milligrams per deciliter, although recent tests show a slight upward trend.
- The speaker expresses concern about the implications of rising triglyceride levels on cardiovascular health as they age.
LDL Levels and Optimization Strategies
- The speaker’s LDL level was measured at 57 milligrams per deciliter, which is considered low and could be associated with increased coronary heart disease mortality risk.
- The speaker aims to balance their lipid profile by potentially allowing for a higher LDL level while decreasing lipoprotein A and triglycerides.
- The speaker emphasizes the importance of tracking multiple biomarkers together to achieve an optimal cardiovascular health profile.
Dietary Correlations with Biomarkers
- The speaker tracks dietary intake meticulously to analyze correlations between diet and biomarkers, specifically lipoprotein A.
- There is a significant positive correlation between net carbohydrate intake and lipoprotein A levels, indicating that higher carb intake is associated with higher lipoprotein A.
- The speaker has reduced their average daily net carb intake in hopes of lowering lipoprotein A levels in future tests.
- Total fat intake showed an inverse correlation with lipoprotein A, suggesting that higher fat intake may help lower lipoprotein A levels.
Future Testing and Monitoring
- The speaker plans to conduct another blood test on October 27th to assess the effects of dietary changes on their biomarkers.
Nope, had it 20 years ago for 4 months and it was discontinued
New Pill From Merck Could Slash Cholesterol Levels, Trials Show
The drug targets the PCSK9 protein, and could give millions of people a more affordable option to reduce their heart disease risk.
Merck, the company that introduced statins to the world nearly 40 years ago, has a new, intensely powerful pill that can slash levels of dangerous LDL cholesterol to levels almost never seen in adults.
The new pill, enlicitide, blocks a liver protein, PCSK9, that slows the body’s ability to clear cholesterol. With most PCSK9 blocked, LDL levels plummet and rates of heart attacks and strokes in high risk patients fall by up to 20 percent in just the first year.
At least six million adults in the United States are eligible for drugs that block PCSK 9.
Merck’s head of research said the goal is to make the pill affordable. It would be an alternative to expensive biweekly or monthly injections of monoclonal antibodies that do the same thing. But only around one percent of eligible patients take the injections, which include Praluent by Regeneron and Sanofi, and Repatha by Amgen. Many patients don’t want to inject themselves, and insurers put up obstacles to paying, cardiologists say. The drugs’ list prices are more than $500 a month.
Multiple studies over the years have shown that the lower the LDL level, the better — heart attack and stroke rates drop as LDL levels fall. And there appears to be no downside to having an astonishingly low LDL level, including one in the teens or twenties. Adults who are not taking cholesterol-lowering drugs usually have levels above 100.).
“Lower is better for sure,” said Dr. Daniel Soffer, a cardiologist at the University of Pennsylvania.
Read the full story: New Pill From Merck Could Slash Cholesterol Levels, Trials Show (NYT)
At this point I go all out
high dose statin/ezetimibe/bempedoic acid/psyllium husk, and a wealth of other supplements to crush that ldl below 30
I wish the psk9 inhibitors were cost affective than I’d have the full arsenal
You’d expect that to drive down the cost of existing medicines, especially repatha in this case. You’d be sorely mistaken!
It’s going to be interesting to see the pricing (and prescription requirements… do you need to “fail” on a cheaper statin before they’ll pay for a PCSK9 Pill?).
In theory the market for pills is much, much larger than the injections (people hate injections, generally) and they have refrigeration requirements. So the price can be much lower and still generate vast revenues… we’ll see.
Whatever. I’ll just wait for those pills to become available in India, one way or another. India has a truly epic size problem with CVD. The government will make it a top priority to get ahold of these meds by hook or by crook, patents be damned. And when they become available, I’m placing my order. I have zero faith in the insurance industry in the US, their willingness to cover them unless you’re on the verge of death if not actually clinically expired, or the pharma companies and PMBs marketing them at anything less than the price of your first born. I have no desire to deal with obstinate doctors, ghoulish companies and other bloodsuckers along the chain. Order from India, done. First however let’s wait until the drugs actually come out and then hit India. Then we’ll talk. YMMV.