Mechanistically even at very low apoB levels, the apoB can still deposit soft plaque at a low rate, but there is some other mechanism that is constantly dissolving soft plaque at some genetically determined slow rate and getting picked up by HDL particles to be recycled in the liver. Unfortunately it is not clear what determines the rate at which soft plaque is picked up, but it may be related to the level of HDL. There are some low quality studies suggesting that on average soft plaque starts regressing below ApoB = 50, but there is a lot of variability between individuals.
For what it’s worth CETPi trials and genetic mutations that increase HDL but doesn’t decrease LDL hasn’t shown any benefits on cardiovascular outcomes.
However, Obicetrapib, a new CETPi will likely change this
Obicetrapib has no off target effects which have limited the results for prior medications in this class
Obicetrapib: There is still Life in the CETP Inhibitor! - PMC
Yup, it’s because it massively lowers LDL.
Do you have evidence of this? I’ve heard the speculation that lipoproteins may have been beneficial in wound healing and fighting viral infections, but I haven’t seen any good evidence of that.
To my knowledge, I’m also not aware of any evidence that people who are aggressively lowering circulating LDL-C have worse wound healing. But I’ll be happy to be corrected. I did ask GPT-5, and it said there’s no evidence, aside from in people who have low lipoprotein levels due to malnutrition or severe systemic diseases, which would obviously massively impact wound healing.
Not really correct, if we’re being picky. The blood vessels form part of the BBB, because the endothelial cells are linked by tight junctions to prevent passage of molecules. They also contain receptors to allow selective transport of molecules between the blood and the brain. However, the whole BBB is formed from a cooperation of endothelial cells, pericytes, glial cells, astrocytes and even neurones - the new word is “neurovascular unit”. The BBB isn’t some wall - it’s a dynamic system which controls what enters and what leaves.
You’re absolutely correct about hypertension being a major risk factor though, and I would assume/hope that anybody taking Rapamycin for health has already covered the absolute basics like controlling their BP.
Is that right? It’s correct that we do build atherosclerotic plaque in multiple arteries. The coronary artery is particularly vulnerable because it is under super high pressure (being basically the first branch off the aorta). Also, I’ve seen some presentations modelling this, and the places where plaque accumulates tend to be where you have branches and the blood needs to change direction, which applies shear forces. You of course can build plaque in other places, such as the carotid, or the middle cerebral artery which supply the brain. However, in brain capillaries (where the BBB is “located”) the flow is low pressure and very slow. I don’t think you’d build plaque or accumulate lipoproteins there.
Nothing. Let’s take a few things as facts:
-
Her current ApoB/Lp(a) level is still enough to build soft plaque. The CTA proves it.
-
You said she already has a great diet and exercises. So we’d assume there’s not much additional room to reduce risk by cutting saturated fat, lowering her BP etc.
The only thing left is lowering her ApoB, from wherever it is now, down to something low enough that she stops building more plaque. Tinkering with an already good diet, or adding supplements isn’t going to make a big difference. The only thing that will significantly move the needle is medication. (I’m aware that you already know this, haha. But some people just need to push to finally start taking the damn pills).
May also be worth her doing a Lp(a) test, just to see whether that might also be involved?
A researcher I know that me that she thinks it’s diffusion. If cholesterols are lower in the blood than in the artery wall, some will leave down the concentration gradient. (Of course some will be trapped, don’t have a diffusion pathway etc)
Dunno.
But where do the initiation of strokes happen? Is it in places with similar historical concentration of lipoprotein as rest of the circulation e.g affected by cholesterol lowering drugs?
There are 2 types of stroke:
-
Hemorrhagic stroke: This is NOT caused by LDL or plaque, but by injury/damage to the blood vessel walls by high blood pressure or head trauma. LDL may actually help speed healing of injured blood vessels.
-
Ischemic stroke, caused by blockage of the blood vessels in the brain, either from plaque in the brain OR (more commonly) from blood clots OR plaque pieces travelling from blood vessels elsewhere in the body where plaque has torn lose causing bleeding and clotting.
Overall, Ischemic stroke is much more common than Hemorrhagic stroke, so it is likely that high LDL will actually increase overall mortality from all types of stroke, even if it reduced mortality from Hemorrhagic stroke.
We do want to know the quantity (percent) of strokes are caused where and by what, if necessary the magnitude of the stroke, and if the initiation area were subject to systemic LDL concentration. I’m suspecting the majority even adjusted for magnitude of strokes were initiated in places with the same LDL particles count that is clogging up the heart.
All that’s good, but may not be enough for those with strong family history of early MIs and with non zero CAC Scans. LP(a) can be reduced if elevated although that’s expensive. What about inflammatory contributors to heart disease? hsCRP elevation is not good, and increases risk associated with whatever your apoB level is. Keeping kidneys healthy would be reflected in good eGFR levels ( > 60), which would allow urine discharge of TMAO - hence minimal TMAO associated risk. If TMAO is elevated, a WFPB diet work. It would also be wise to look at your OxLDL levels, since this is an active molecule that enhances plaque formation. Note that elevated TMAO is likely to increase OxLDL while statin use is shown to lower OxLDL levels, as does Ezitimibe.
Here you go. I know the scientist who did this research.
Rapamycin enhances neurovascular, peripheral metabolic, and immune function in cognitively normal, middle-aged APOE4 Carriers: genotype-dependent effects compared to non-carriers - PMC
Four weeks at 1mg per day is a nice proof of concept, but it would be nice to get a follow up tracking 6mg per week for six months.
Sure you can lower hsCRP if you can.
TMAO has no effect on heart disease risk.
The preponderance of evidence would seem to disagree with you.
I was thinking about a MR study showing or detecting no effect.
We used genetic variants as instruments to test the causal associations. Genetically predicted higher TMAO and carnitine were not associated with higher odds of T2DM, AF, CAD, MI, stroke, and CKD after Bonferroni correction (P ≤ 0.0005). However, we observed that genetically increased choline showed a suggestive association with higher risk of T2DM (odds ratio 1.84 [95% CI 1.00-3.42] per 10 units, P = 0.05). In contrast, genetically predicted higher betaine (0.68 [0.48-0.95] per 10 units, P = 0.023) was suggestively associated with a lower risk of T2DM. We observed a suggestive association of genetically increased choline with a lower level of body fat percentage (β ± SE -0.28 ± 0.11, P = 0.013) but a higher estimated glomerular filtration rate (0.10 ± 0.05, P = 0.034). We further found that T2DM (0.130 ± 0.036, P < 0.0001) and CKD (0.483 ± 0.168, P = 0.004) were causally associated with higher TMAO levels. Our Mendelian randomization findings support that T2DM and kidney disease increase TMAO levels and that observational evidence for cardiovascular diseases may be due to confounding or reverse causality.
I am not a brain expert, but what I do know is that any form of atherosclerosis isn’t just about the systemic LDL-C concentration. The anatomy of the actual artery is important, and that obviously varies between people. (Plus all the usual variables like blood pressure, reactivity of your immune system etc). I have no idea how you’d measure historical concentration of lipoproteins though.
For ischaemic strokes, the initiation site is sometimes in the brain itself (middle cerebral artery etc) or immediately upstream of the brain (like the carotid, which is why people look at that by ultrasound as a clue to the condition of your arteries). You can also generate clots from other places, like in the heart if you have atrial fibrillation, and the clot can shoot up and lodge somewhere else.
Anyway, I think the larger point is that for most people, they’re more likely to die from ASCVD than anything else, and lowering your LDL-C is pretty much the best safeguard against that.
I’m differentiating which strokes we have control of with LDL-C lowering therapies and which strokes we don’t. Those strokes under the influence of systemic LDL concentration rather than past the BBB is what I mean, and since risk from LDL-C is never a snapshot but historical concentration, I mean what’s been in the past. Initiation because as you say the stroke can travel to the brain. So amount and magnitude of strokes in this area lets us know which ones we can prevent with reducing LDL-C solely.
This basically is the more precise question IMO.
gpt-oss-120b wrote RR reduction lifetime stroke risk is reduced by 80% by combining apoB to ~30, BP 115/80, no type 2 diabetes, normal weight. I should’ve added kidney function to the question.
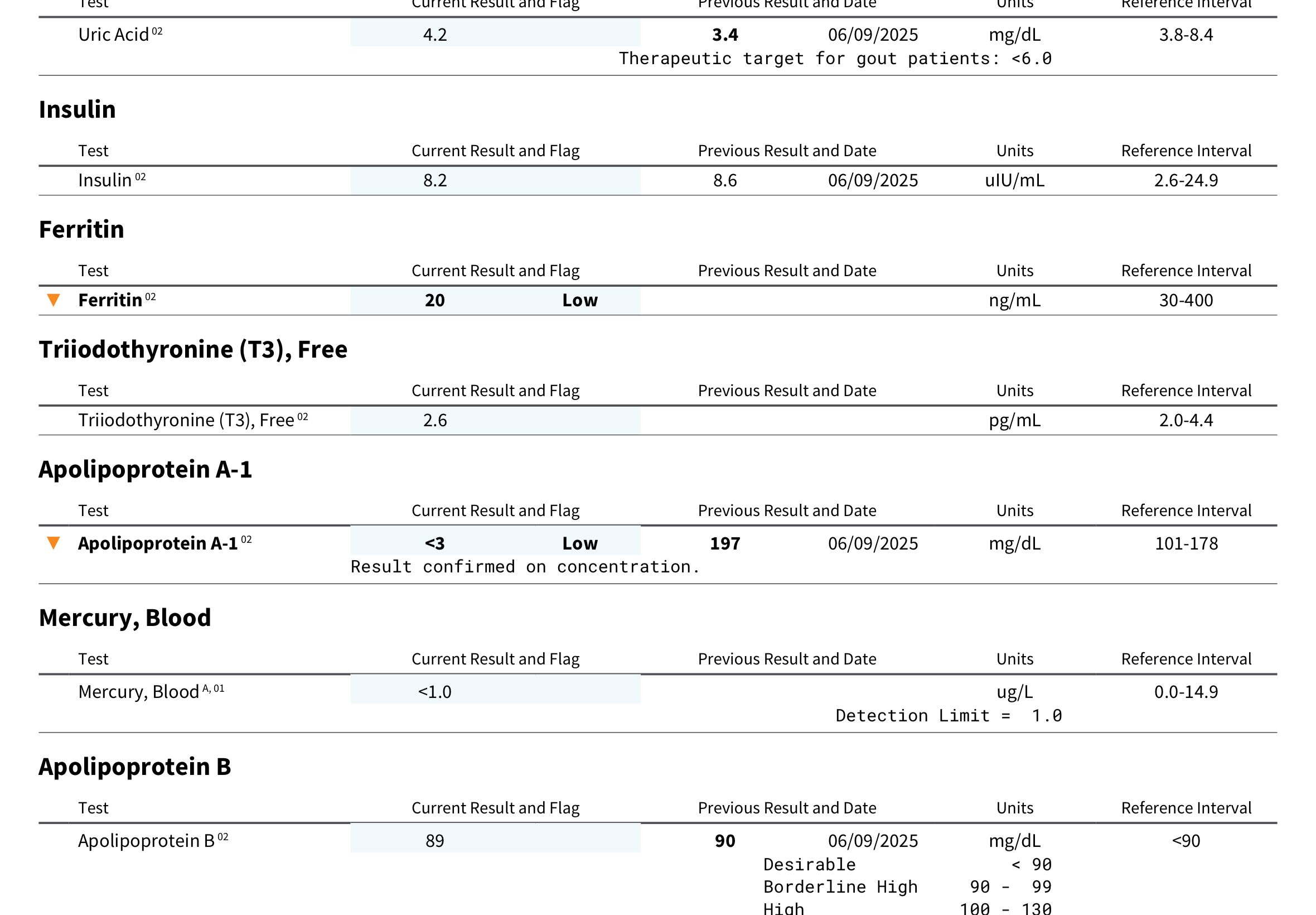
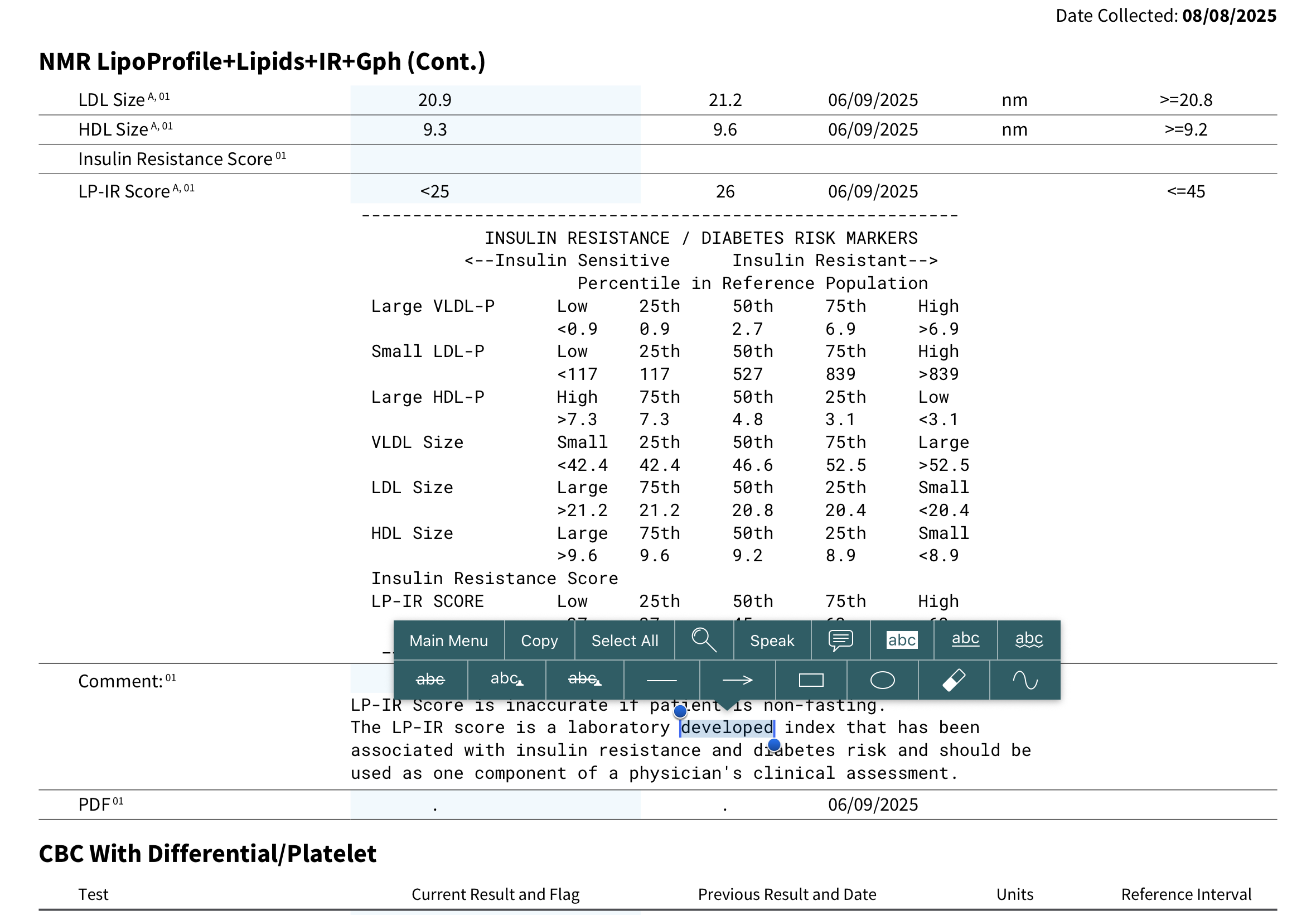
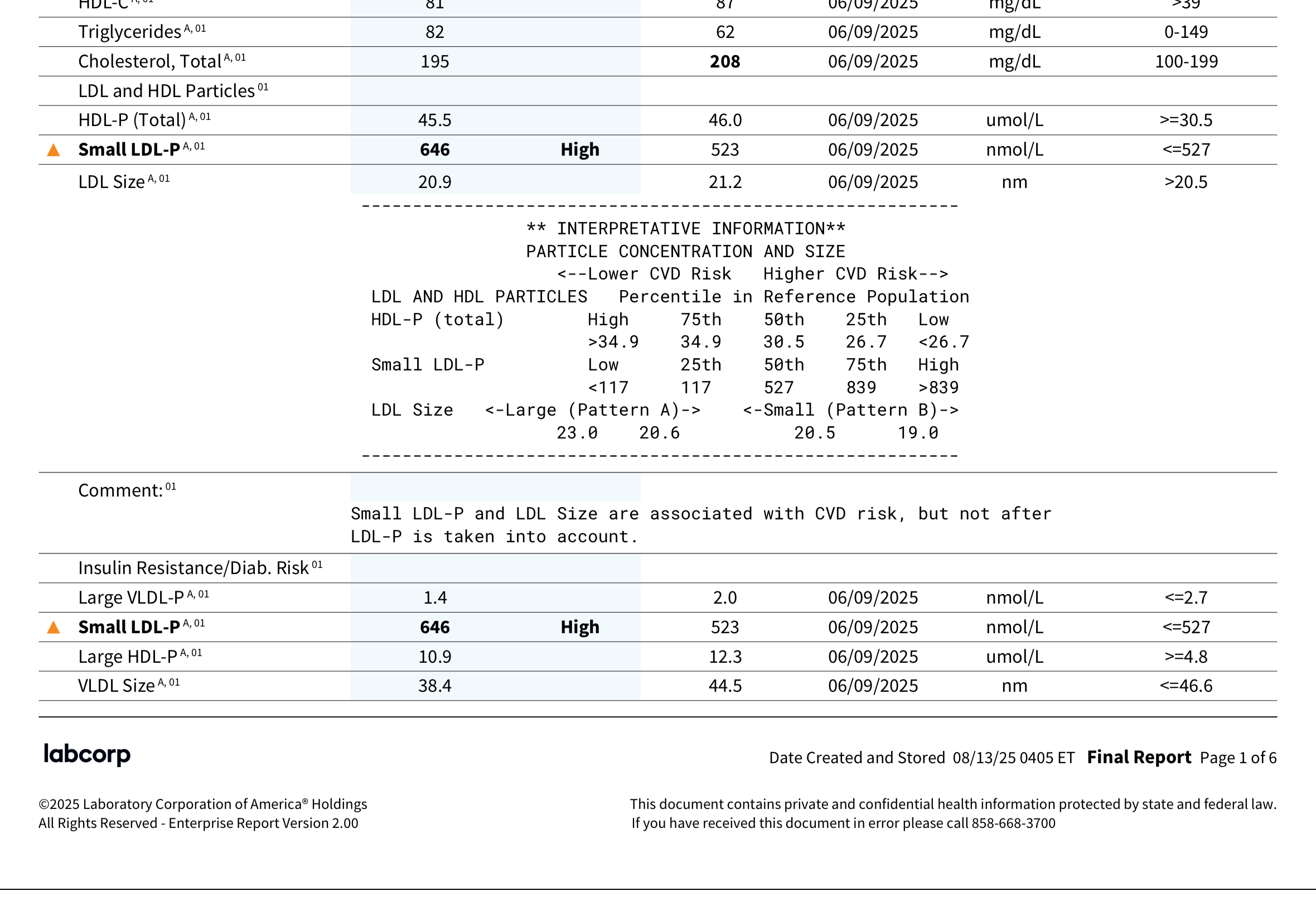
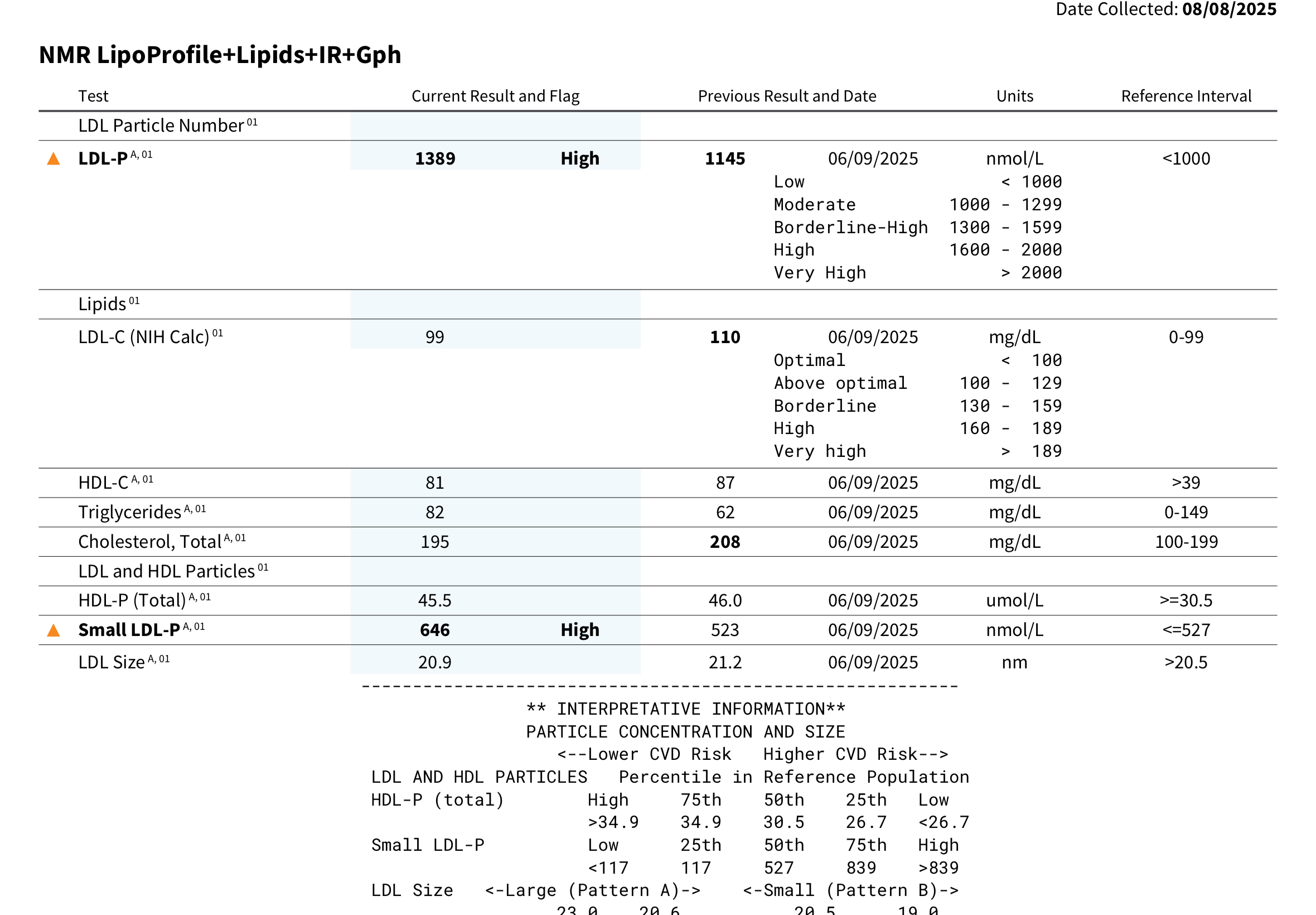
As promised I’m posting results of the n=1 experiment wrt. lipid medication. No changes in diet or exercise or other lifestyle factors, sleep, level of stress insofar as I can tell (low), supplements. The only med change was going from the Zydus brand sirolimus 6mg/1-week to Eris/Biocon brand same dose and schedule, have been on it ever since that test, so 8 weeks of the Eris for this test. This test (3) keeps pitavastatin 4mg/day but substitutes 10mg/day ezetimibe for the previous 180mg/day bempedoic acid.
So the tests are as follows - each intervention roughly 6 weeks with no washout period:
(1)pitavastatin 4mg/day alone (switched from atorvastatin 10mg/day)
(2)pitavastatin 4mg/day + bempedoic acid 180mg/day
(3)pitavastatin 4mg/day + ezetimibe 10mg/day - CURRENT RESULTS test on 08/08/25
And the next test is ongoing since 08/09/2025, the results will be in a blood test on 10/28/25:
(4)pitavastatin 4mg/day + bempedoic acid 180mg/day + ezetimibe 10mg/day
Pitavastatin 4mg/day alone vs pitavastatin 4mg/day + bempedoic acid 180mg/day vs pitavastatin 4mg/day + ezetimibe 10mg/day
Pita alone - 5 months; Pita + BA - 39 days.
Legend: Pita alone - PA; Pita + BA - P+BA; Pita + ezetimibe P+EZ
Total Cholesterol: PA - 228 mg/dL ; P+BA - 208 mg/dL; P+EZ - 195 mg/dL
LDL-C Calc: PA - 123 mg/dL ; P+BA 110 mg/dL; P+EZ - 99 mg/dL
Trig: PA - 93 mg/dL ; P+BA - 62 mg/dL; P+EZ - 82 mg/dL
HDL: PA - 89 mg/dL ; P+BA - 87 mg/dL; P+EZ - 81 mg/dL
I’m not thrilled with this. The decline in LDL is pretty marginal. No change in ApoB (delcine from 90 to 89). The trigs and HDL going in the wrong direction, as is the entire lipid profile (number of small LDL increase, size of LDL decrease etc.)
A truly bizarre result for Apolipoprotein A-1:
Apolipoprotein A-1:
"Apolipoprotein A-1 02 <3 Low mg/dL ref.101-178
Result confirmed on concentration."
My previous A-1 on 06/09/25 was 197 mg/dL. What??
A lot of other biomarkers going in the wrong direction.
For me ezetimibe 10mg/day has been an overall, FAIL.
Ezetemibe is an add on. It is best used with a statin and/or Bempedoic Acid. My family and I have had excellent results with Ezetemibe and RCTs have also shown the same.
I’m sorry your results didn’t turn out as well as the RCTs, but we all have different reactions to different medications.
Right. I was hoping ezetimibe as add on to the pitavastatin would be a win, but it completely wrecked my lipid profile. Since 08/09/25 I’ve been on Brillo EZ, 180mg/day bempedoic acid and 10mg/day ezetimibe in addition to the pitavastatin 4mg/day. October 28, I will have my next test, so curious to see what happens. I’m not optimistic. My options are shrinking. I may have to start thinking about a PCSK9i, while waiting for some drug to crush my also sky high Lp(a). What a mess.
And all of this on a diet optimized to eliminate as far as possible saturated fat, EPIC amounts of fiber, including multiple kinds of soluble fiber, psyllium etc., pescetarian etc. good exercise, low stress etc.
Yes, we all have our individual biological makeups, and mine is trying to kill me by atherosclerosis (fortunately, CAC score zero at 65yo).
I can only envy people’s good lipid profiles and responsiveness to meds. Luck of the draw, I pulled a joker from the lipid panel deck. ![]()