John it had a video transcript at the bottom after pressing more. It would have taken you directly to the subject matter. All this posted transcript not necessary.
That still does not explain why the ratio of albumin to creatinine in urine is considered to be a proxy for inflammation. I don’t see what the mechanism is.
I know that albumin in serum is vulnerable to lots of short term changes like fasting and creatinine in serum can be increased by exercise. I would expect that creatinine in urine would follow that and similarly with albumin hence the ratio could vary by a lot on factors not relating to the permeability of the intima in the kidney.
The intima in kidneys is exactly identical to intima in arteries through out the body including heart, brain, etc. The degree of inflammation in kidneys will be the same in all the arteries through out the body
What do you mean by “inflammation”?
This is a good paper which explains why the intima in the kidney is different to more generally (although not only the kidney).
This explains what fenestrated means
That does NOT seem to be correct - see below. What do you base it on?
I’ll research this more before the next time I consider doing any non MRI, ultrasound or Dexa imaging.
But while CT imaging can be very valuable, it does seem like it should be traded against the risks of it: see for instance
Study reveals CT scan overuse could account for 1 in 20 new US cancers
A new study published in JAMA Internal Medicine reveals that the radiation dose currently used in routine computed tomography (CT) examinations in the United States is projected, using modeling, to eventually account for 5% of all new cancer diagnoses annually. The study estimates a range of 80,000 to 127,000 projected cancers based on sensitivity analyses, with a central estimate of approximately 103,000 future lifetime cancers from CT scans performed in 2023, and provides 90% uncertainty limits for these projections.
Paper: https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2832778
People can research themselves but @KiwiGuy ‘s statement may not bit be correct:
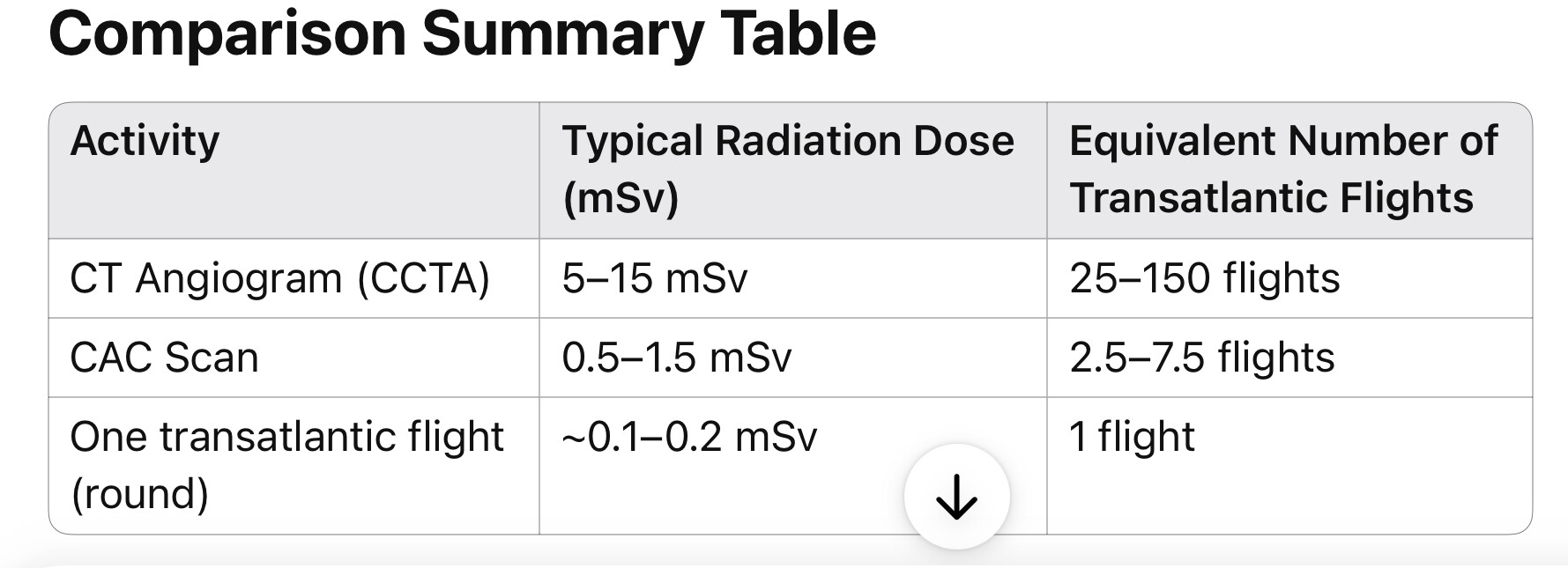
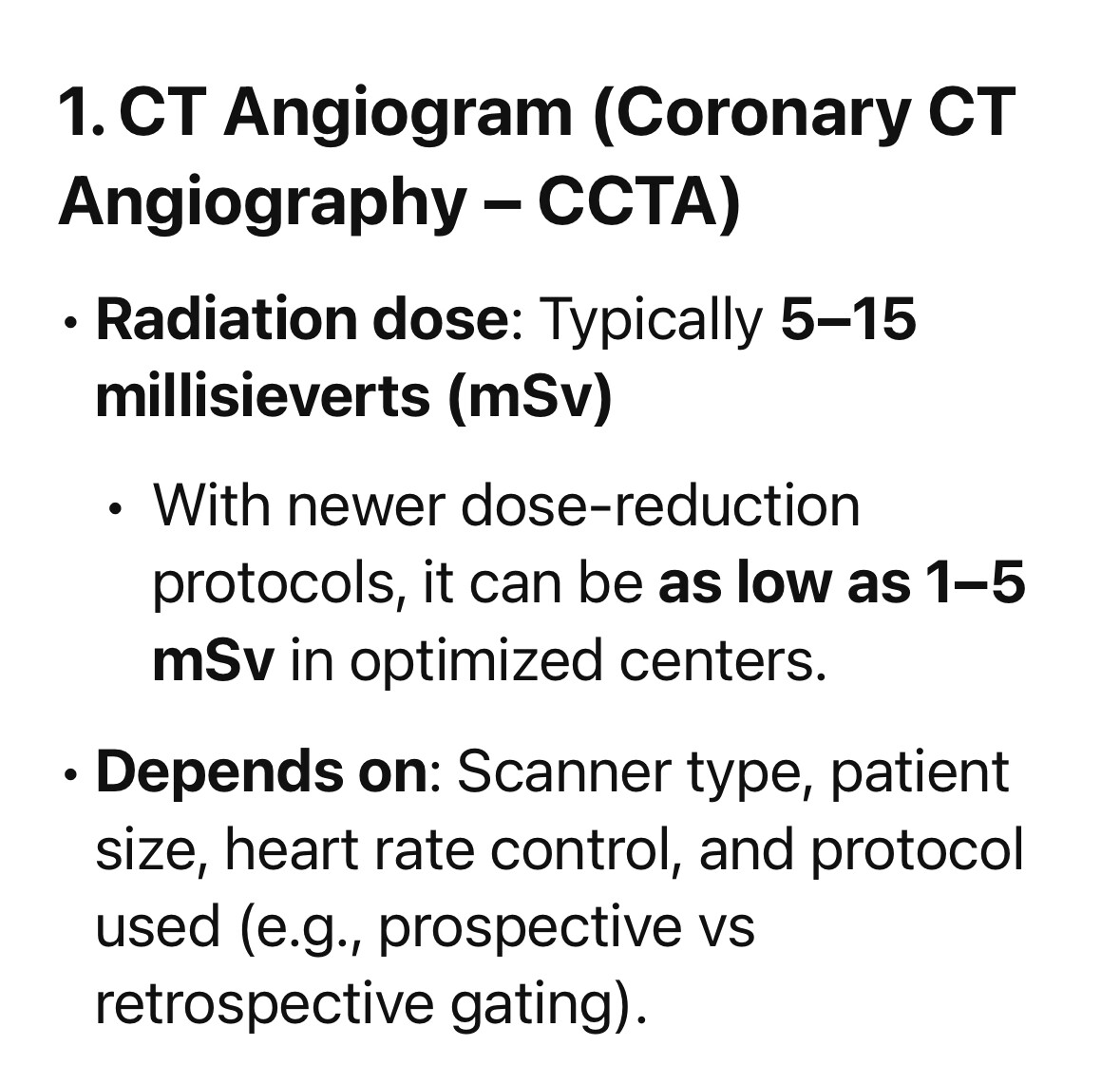
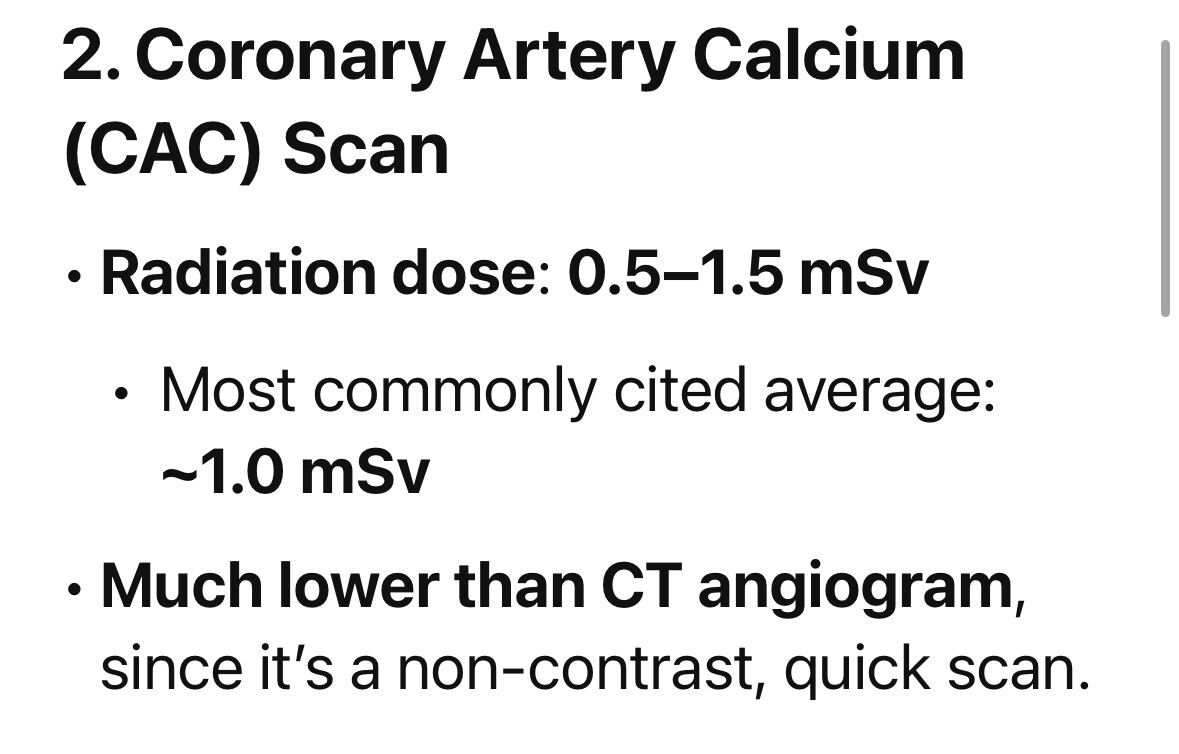
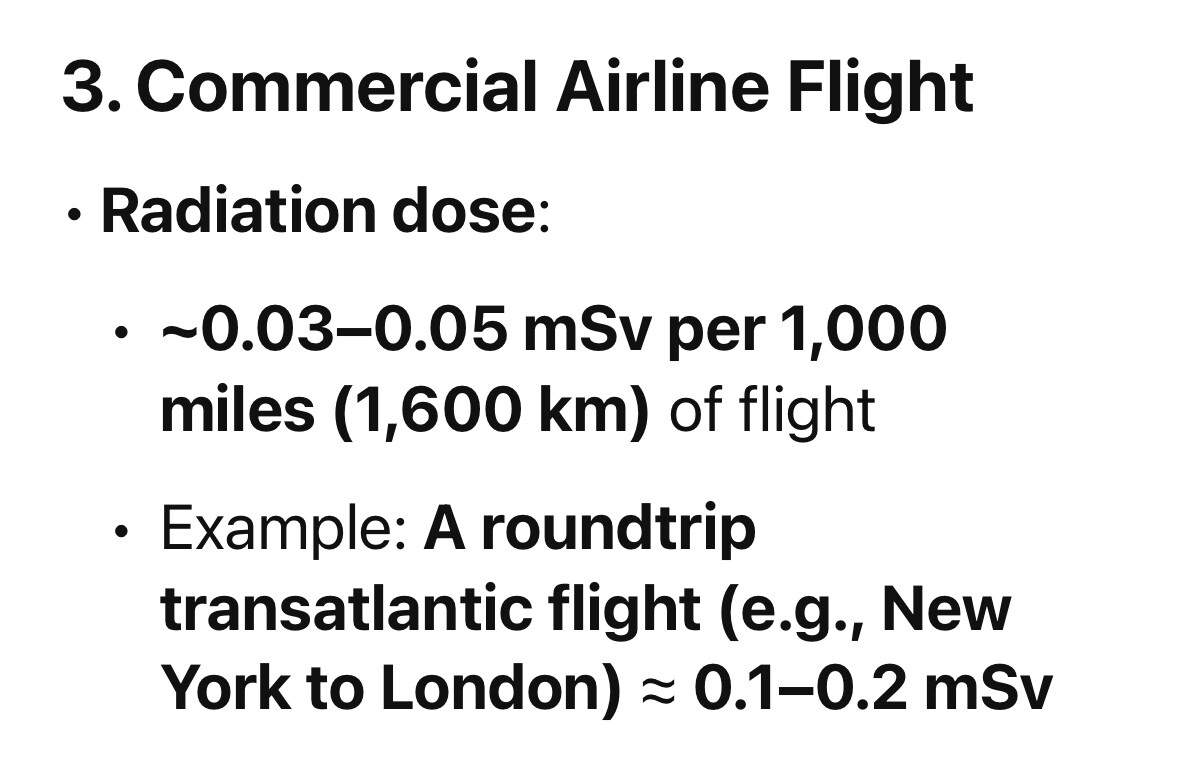
Two different AI models gave a similar answer on comparing the radiation to air flight:
Unpacked as
Sorry to be picky here, but atherosclerosis is literally defined by the formation of lesions in the arterial wall. You can’t have those lesions without lipids. You can have inflammation, poor blood flow, aneurysms, or other vascular problems, yes, but you can’t have atherosclerosis without lipid accumulation. So maybe not the only factor, but certainly the most important.
I do agree that lipids don’t magically accumulate by themselves, and some sort of insult to the arterial endothelial layer is necessary. However, I don’t think it’s realistic that people will be able to live without that happening. There’s evidence that even just the simple shear forces of the blood flow itself is injurious. There are examples of foetuses with arterial plaque. So the lipids are by far the most influential thing, and they’re easily modifiable. I would say that one only needs to worry about EC senescence, differentiation etc once their ApoB is below like 40mg/dl. Otherwise you’re missing the wood for the trees.
In some way, this represents a microcosm of the entire problem in the field. Heart attacks and strokes are still the biggest killers in the world, completely unnecessarily, when we already have a bunch of different ways to prevent the majority of them. But you still have people doing shots of coconut oil and other crazy stuff due to simple misinformation.
Appreciate the links — but let’s not get carried away.
My CTA was 1.31 mSv — that’s roughly 9–13 long-haul flights worth of radiation. Not trivial, but not exactly playing with uranium either. If that level of exposure were genuinely dangerous, we’d see sky-high cancer rates in pilots, flight attendants, and astronauts — people who get this kind of dose every few weeks as part of their job. But we don’t. Airline industry studies consistently show no meaningful increase in solid tumor cancer rates, even among long-haul crew with decades of exposure.
Now, the JAMA paper claims 103,000 future cancers from CT scans performed in 2023. That’s not based on observed data — it’s a hypothetical projection, based on the linear no-threshold (LNT) model, which assumes that any radiation exposure increases cancer risk, linearly and cumulatively. That model is widely debated and likely overstates low-dose risk, especially with modern imaging protocols.
Just to put that claim in perspective:
- Smoking kills ~160,000 Americans from cancer every single year — real data.
- JAMA suggests CT scans from one year might eventually cause 103,000 cancers — modeled guesswork, and not all would be fatal.
So essentially they’re implying that one year of CT scans is nearly as carcinogenic as all smoking in the U.S. in the same year. That’s… bold.
CT overuse should absolutely be questioned. But a 1.3 mSv cardiac CTA, done for the right reason on a modern scanner, is incredibly low-risk. The idea that this sits anywhere near smoking in terms of cancer risk is pure extrapolative fiction — and wildly out of step with what we see in high-exposure professions like aviation.
So we don’t disagree in a broader sense. I think it is worth controlling lipids. Statins have their role in this. Personally I keep an eye on LDL-C, ApoB and Lp(a).
How ironic that I am reading this right now while on an international flight WiFi
I worked at the Nevada Test Site for 15 years in my younger days. I worked in the “forward area”. This was during the era of underground testing, but occasionally the tests vented (leaked radiation), so on a couple of occasions, I received more than my fair share of exposure to ionizing radiation, specifically radioactive xenon and iodine.
Although there weren’t many studies about low-dose exposure to ionizing radiation, I did visit Oak Ridge National Laboratories. While there I talked to health physicists who were studying the survivors of Nagasaki and Hiroshima. They were surprised that the amount of leukemia and other effects of high radiation exposure was lower than expected.
I am 84 and still living to tell the tale.
If you have watched any of the videos about the aftereffects of wildlife in the high-radiation areas around Chernobyl, it appears that plant life and wildlife, including feral cats, are thriving in the absence of people, many years after the initial incident.
“Some early animal studies, and even some more recent ones (e.g., on certain strains of mice or beagle dogs exposed to very low, continuous gamma irradiation), have reported extended mean lifespans or reduced disease incidence in the low-dose groups compared to unexposed controls.”
In any case, here are a couple of articles that support the idea that a bit of radiation isn’t particularly harmful. Albeit current health physicists will probably tell you all ionizing radiation is harmful.
The theory on which low radiation exposure being beneficial is:
“Hormesis is the concept that biologic systems can respond in a positive way, or be stimulated by, physical or biologic exposure to low doses of an agent that is toxic at higher doses (1). Additionally, hormesis is defined as “any physiological effect that occurs at low doses which cannot be anticipated by extrapolating from toxic effects noted at high doses” (2). Therefore, radiation hormesis is the theory that biologic systems can respond positively to exposure to low doses of ionizing radiation.”
I am not myself persuaded that a little bit of DNA damage is a good thing.
Here is a tidy transcript, summary, and critique of the video “Hormesis from Low-Dose Radiation” (YouTube link).
 Tidy Transcript
Tidy Transcript
Title: Hormesis from Low-Dose Radiation
Hormesis was first shown to extend life over a century ago when low doses of radiation increased the lifespan of beetles. Scientists originally intended to use x-rays to sterilize grain pests, but instead, low doses made the beetles live longer.
This effect was later replicated using gamma rays and in over a dozen other insect species—houseflies, crickets, wasps, mosquitoes—showing consistent lifespan extensions of 20–60%.
What’s going on?
Hormesis is thought to be an adaptive response to low-level stress. The body perceives a mild insult, triggering a compensatory overcorrection that more than offsets the initial damage—resulting in a net benefit.
In radiation’s case, high doses damage DNA and kill cells. But DNA repair machinery is metabolically expensive to run full-time. Low-dose radiation may signal a DNA-damaging environment, prompting the body to ramp up its repair systems. This increased DNA protection might explain the longer lifespan observed—what doesn’t kill you makes you stronger.
Hormesis might not be limited to insects. One study claimed that survivors of the Hiroshima and Nagasaki bombings who were exposed to low-dose radiation had lower cancer mortality and longer lives compared to unexposed people. In contrast, those closer to the blast suffered higher cancer rates and shorter lives.
Some of the longevity benefit might be due to superior medical care provided under the Law Concerning Relief to Atomic Bomb Survivors, but hormesis may also play a role.
Marie Curie, who discovered radioactivity and later died of radiation-induced bone marrow failure, is quoted: “Nothing in life is to be feared; it is only to be understood.” Her remains were buried in a lead-lined coffin.
Why would animals evolve to withstand radiation?
Because the Earth is constantly bombarded by cosmic rays—our bodies receive ~20,000 hits per second. What happens if we remove that exposure?
Experiments show that single-celled organisms like Paramecia grow poorly in lead-shielded boxes, and the thicker the shielding, the more their growth is inhibited. Human cells under these conditions show increased DNA damage and mutations.
This suggests that natural background radiation might have a beneficial hormetic effect by keeping our stress-response systems engaged.
Even a foot of lead only blocks about one-third of cosmic rays. To reduce exposure more drastically, researchers went over a mile underground into SNOLAB (Sudbury Neutrino Observatory) in Canada.
Unexpectedly, fish raised underground grew larger and heavier than surface fish. Researchers speculated that radon gas trapped in the mine may have offset the lack of cosmic rays—so the results remain inconclusive.
Conclusion: We don’t yet know enough about low-dose radiation to exploit hormetic effects safely. Fortunately, there are safer ways to leverage hormesis for health and longevity.
 Summary
Summary
- Hormesis is a biological phenomenon where low-dose stressors (like radiation) trigger adaptive, overcompensating protective responses.
- First shown in beetles in the early 20th century, radiation hormesis increased lifespan across multiple insect species.
- The suggested mechanism is DNA repair upregulation in response to mild DNA damage.
- Some data from atomic bomb survivors indicate that individuals exposed to lower radiation doses had lower cancer risk and longer lifespans, possibly due to hormesis—but confounding factors like enhanced medical care complicate interpretation.
- Natural background radiation may play a low-level regulatory role in cell growth and DNA stability. Shielding organisms from it leads to more, not fewer, mutations.
- In one deep-underground study, fish grew larger, possibly due to altered radiation environment, but radon exposure complicates conclusions.
- Caution is urged: radiation hormesis may exist, but its safe exploitation in humans is not yet justified.
- Safer hormetic strategies include exercise, intermittent fasting, and phytochemicals.
 Critique
Critique
 Strengths
Strengths
- Clear, logical structure: Moves from insect studies → mechanistic theory → human epidemiology → background radiation → lab experiments → conclusion.
- Balanced skepticism: Emphasizes the uncertainty surrounding the safety and generalizability of radiation hormesis.
- Wide-ranging examples: Covers both controlled lab observations and historical human data, broadening relevance.
- Scientific humility: The final takeaway urges caution, discouraging premature therapeutic use of radiation hormesis.
 Weaknesses
Weaknesses
-
Overinterpretation of A-bomb survivor data:
- The claim that low-dose-exposed survivors lived longer is controversial.
- Many studies (e.g., Preston et al., Radiation Research, 2003) emphasize increased cancer risk even at low doses.
- The observed benefit may be survivorship bias or due to better medical care, not hormesis.
-
Inconclusive mechanistic evidence:
- DNA repair activation is plausible but still speculative in long-term lifespan enhancement.
- Animal data is solid for insects, but poorly replicated in mammals, particularly humans.
-
Fish study lacks rigor:
- Confounding by radon undermines any claim about suppressed cosmic rays.
- Growth rate changes in fish are not equivalent to increased healthspan or lifespan.
-
Potential for misapplication:
- The video could unintentionally encourage pseudoscientific practices involving radiation exposure.
- Needs stronger disclaimers about dose-dependent toxicity.
 Conclusion
Conclusion
While radiation hormesis is a scientifically interesting phenomenon with some experimental support, especially in simple organisms, it is not currently a safe or validated approach for human longevity. The video provides a thoughtful exploration but must be interpreted cautiously due to:
- methodological limitations in human data,
- unresolved mechanisms, and
- the inherently toxic potential of ionizing radiation.
Practical takeaway: Stick to well-studied forms of hormesis—like exercise, thermal stress, and dietary restriction—to promote health and longevity safely.
Would you like a list of peer-reviewed studies on radiation hormesis or background radiation effects on DNA stability?
Fascinating
I think I’ll still be on the conservative side until much more info comes out
But very interesting hypothesis
Statins as Antithrombotic Drugs
https://www.ahajournals.org/doi/10.1161/circulationaha.112.145334
“In this review, we present experimental data in support of the ability of statins to interfere directly with the clotting system and platelet activation, as well as the clinical settings that suggest that statins exert beneficial effects related to their antithrombotic properties.”
Effect of statins on platelet function in patients with hyperlipidemia
“It is generally assumed that cholesterol reduction by statins is the predominant therapeutic result underlying their beneficial effects in cardiovascular disease. However, the action of statins may be partially independent of their effects on plasma cholesterol levels, as they combine lipid lowering with positive effects on hemorheological conditions and endothelial function. We evaluated the impact of statin treatment on platelet adhesion to fibrinogen (spontaneous and ADP-activated), along with ADP, collagen or ristocetin-induced aggregation in type II hyperlipidemic patients. The study group included 70 persons: 50 patients affected by type II hyperlipidemia without concomitant diseases and 20 healthy volunteers. The effects of 8-week statin treatment (atorvastatin 10 mg/day, simvastatin 20 mg/day, or pravastatin 20 mg/day) on platelet activation were evaluated. Regardless of the type of statin, a significant decrease in ADP-induced platelet aggregation was observed: for atorvastatin 50.6 ±12.8% vs. 41.1 ±15.8% (p < 0.05), for simvastatin 57.2 ±18.0% vs. 44.7 ±22.1% (p = 0.05), and for pravastatin 55.8 ±19.5% vs. 38.8 ±23.3% (p < 0.05). There was no significant effect of statins on collagen or ristocetin-induced platelet aggregation and adhesion. Therapy with statins beneficially modifies ADP-induced platelet aggregation in patients with hyperlipidemia and does not affect spontaneous or ADP-induced platelet adhesion to fibrinogen and platelet aggregation induced by collagen or ristocetin.”
The Effects of Statins, Ezetimibe, PCSK9-Inhibitors, Inclisiran, and Icosapent Ethyl on Platelet Function
https://www.mdpi.com/1422-0067/24/14/11739
Effect of Statins on Platelet Activation and Function: From Molecular Pathways to Clinical Effects
https://onlinelibrary.wiley.com/doi/10.1155/2021/6661847
Antiplatelet Actions of Statins and Fibrates Are Mediated by PPARs
https://www.ahajournals.org/doi/10.1161/atvbaha.108.183160
Independent association of Lp(a) with platelet reactivity in subjects without statins or antiplatelet agents
I met with a new cardiologist today who did an EKG.
This was my first since starting rapa, and he noted it looked better than any of my previous EKG results he had access to.
I don’t know how common or not this is, but incase this is unusual, I wanted to share my n=1 in the event that rapa might be a contributing factor.
He didn’t give you anything in writing did he? Or explain any details at all?
It’s interesting because I didn’t think getting your CAC up to 400 would even change the ekg. It shouldn’t have been bad in the first place. Mine is up there, I have a yearly stress test, I think 12 leads doing ekg on the treadmill. He never sees anything wrong.
How can a EKG look better or worse and not binary good or bad?
You can have more or fewer ectopics for instance. It’s not binary.
He spent two hours with me!!!). But this is one thing he didn’t go over in detail.
For clarity, I’ve never had a bad ekg (no one has ever said a word, but I assume if it were bad, I would have heard something). So, I assume this is just degrees of good.
Also, he said my results from my 2022 stress test were impressive (yay)…
He said he sees that most of my plaque is in my right ventricle (I have no idea if there is any significance to this).
I talked to him at length about doing the CLEERLY CCTA.
My brother’s cardiologist said he didn’t recommend it because the plaque affects their ability to see. My internist said the same thing.
I was still thinking that perhaps it’s still a good thing to consider because at worse it’s not useful, but at best it could be lifesaving. He explained the downside of doing it with a heavy plaque burden. First there is the radiation that we all know about (I don’t know how big of a deal this is, aside knowing less is better).
He said my CAC was almost 500 a decade ago, so we know it’s going to be somewhat worse now. When the machine doesn’t have a clear view, there will often be false positives… meaning, it will mistake it for a lot of soft plaque and narrowing (he explained this in a much more technical way that I wish I could repeat to you).
He said when we see that, we have to er on the side of caution and do an angiogram which has risks… and I might have put myself at risk for no reason.
I’m still not sure what to do… if anyone has opinions on any of this, by all means do chime in.
Here is a question about a stress test for you. He does want me to do another stress test in 6 months. He wants it to be with an ultrasound instead of nuclear just to limit exposure. If we are hiking etc and have no shortness of breath, it was my impression that we are doing our own form of a stress test and don’t need an official one. If you are doing a yearly test, I’ll assume there is value…can you explain that to me? I don’t mind doing it other than trying to save the money if there is no benefit.
@A_User yeah, what Adssx said ![]()
The stress test is part of the package I get with my concierge. There is no image. He puts on I think it’s 12 leads and gets a panel of ecg’s. He watches them as I do a 15 minute ramp up on the treadmill (Bruce Protocol if you want to try it). It ends with a run at 22 degree angle and he insists I get my HR to 140 I think. I have no problem usually I can go to 160. I think by looking at this he can tell if my heart is not being fed well enough.
I’ve been doing it for 10 years at least and I think if I’ve been running and I’m in good condition it’s harder to get to the HR he wants to see. If I’ve been in the field too much and not getting exercise I can get it right up there. The heart must have ways of being more efficient as you improve condition.
It sounds like maybe I’m not getting a stress test? Certainly not a nuclear.
I was worried about the contrast on the cleerly. It turns out to be iodine, not so bad. For some reason I thought the CCTA was MRI. It’s CT, so x rays. This makes me a little less worried about it. The MRI would use gadolinium which (to me) seems a little more dangerous. The reading I have done for my daughter, since she is imaged with CT every 3 months for the cancer, is that before a CT you should megadose with melatonin. It can help prevent damage from the x rays. She has been doing this. She does a couple hundred maybe a half hour before.