The CAC correlates with, but doesn’t in any way define the degree of coronary artery disease. You can have a CAC that is 90% tile and have no plaque … and be scared about the CAC or you can have a 20% CAC score and have extensive plaque. Now if you have a critical lesion or lots of disease I think it helps to know and consider how aggressive on is with their therapy. It is true that without ischemic findings on workup on a population basis, there is little benefit to intervening for many cases as a statistical matter. I’d however say if I have a 90% lesion of my LAD, I’d certainly be contemplating treating over waiting for an event (which is commonly fatal).
@DrFraser
Can you comment on what the cardiologist said, and that google confirmed, that if one has a high CAC score, the hard plaque might alter the accuracy of the CCTA.
When does one choose to have a nuclear stress test over a CCTA (excuse me if I’m conflating all the names… it seems CCTA, Cleerly, and CTCA are all the same?)
Is this robust to the point @A_User and I have made in the past about the relevant risk period to think about is many decades and not just clinical trial durations?
(for cases like Apo B where we understand that mechanism with high enough probability and that it is something that is compounding over time)
So based on this, do you think there is even any value in the calcium score by itself? It seems not, right?
The CTCA involves more cost - regionally $311-$600 cash pay through MDSave.com, but with a physician order.
CT Cardiac Calcium is $45-$200 typically.
There is more radiation exposure, need for an IV and exposure to contrast with the CTCA.
So I take a look at people who are very low risk of having any disease - and a CT Cardiac Calcium is sensible. Any non-Zero score gets a CTCA.
I have a lot of patients who have had CTCA’s including those with high calcium scores - and the results are useful and interpretable. In areas of heavy calcification in the vessel wall, we still usually see the vessel nicely, but it can limit interpretation. Adding Cleerly is of value in these cases or in cases where there is a reasonable plaque burden.
I don’t think that’s the best criticism of the study, it’s a observational study like many others and they controlled for a few factors (and Lp(a) and hsCRP). You can see the CI’s widening below the 5th percentile. If the methodology allowed for it then the short term would suggest no effect long term because it was statistically significant according to the authors.
Our analysis (Figure) also suggests that the relationship of LDL-C to MACE tends to flatten below ≈90 mg/dL, the range encompassing most patients in the triglyceride-lowering trials, although the wide CIs at the lower range of LDL-C do not exclude a monotonic relationship across the full LDL-C range.
A flattening of LDL-C with MACE or increase in all-cause mortality happens all the time in studies with this design, contrary to RCT’s.
Residual confounding…
What’s the added value of the CTCA in terms of treatment? With a positive calcium score isn’t the ideal treatment aggressive lipid lowering through medication and diet and exercise? So how would CTCA results change that? E.g. my understanding is that studies show that preventative angioplasty is virtually never warranted.
The value add is #1 Many times a CT Cardiac Calcium Score is elevated and yet there is no coronary artery disease in the lumen of the arteries. For example, in 2021 I had a CT Cardiac Calcium of 92 all focused proximal LAD. Late 2021 I got pericarditis almost certainly due to a Covid-19 vaccine and clinically looked somewhat similar to an occlusion MI, so I got an immediate heart cath – Zero disease at all - totally clean.
So if I presumed I had disease based on the CT Cardiac Calcium, I’d be more aggressive with my lipids and also more worried I had disease … when I had none.
We’ve also seen the converse, a CT Cardiac Calcium that is minimal with significant Coronary Artery Disease.
It’s a nice screening tool - but doesn’t actually answer the question of whether someone has CAD.
As to the point on why bother, as the “evidence” is that stenting preventatively isn’t helpful.
I don’t think we really have a study showing this, under these circumstances. I see a fair number of people with occlusion myocardial infarctions - their CTCA the month before would have shown what? Take this group and act vs observe and see what happens.
The challenge is that only 25-30% of MI’s are due to major lesions – would you be happy with a 95% lesion in your LAD or RCA with conservative management … I’d not. But without a CTCA or a heart cath you’ll not know this.
The problem is scattered disease which with plaque rupture is 70% of MI’s - and this - yes I’d not push for a stent, but we’d be much more aggressive on lipid management and advise aspirin.
@DrFraser sorry to be repetitive but I think you missed part of my earlier question.
It seems you said a lot of calcium will interfere with some of the readings, but I think you notice a clear enough result that it will show you want you need to see, correct?
Just yesterday, my brother’s cardiologist said to get a nuclear stress test instead for this reason.
And my second question is when would you want someone to get a nuclear stress test vs a CCTA. I’m not clear on the differences. I had one 3 years ago. Does it show all the soft plaque but only not the lesions? Is CCTA always better? Do you feel both are good to do? Or partially redundant? Thank you.
If it’s stents we’re talking about they do prevent heart attacks and such when used as they typically do (mostly ACS). Avi did a meta analytic review when debunking Dr. Michael Greger et al on this.
It seems also they prevent heart attacks according to Avi in stable CVD although according to him the effect size is not that significant.
My understanding is that stents provide symptom relief but have no statistical relevance in preventing heart attacks or reducing all-cause mortality.
“While stents are effective in reducing restenosis and the need for repeat revascularization procedures, they do not significantly reduce the incidence of heart attacks. Studies have shown that there is no significant difference in the rates of myocardial infarction between patients treated with stents and those undergoing percutaneous transluminal coronary angioplasty.”
“Compared with standard PTCAs, stents more often prevent restenosis and avoid the need for repeated procedures; however, they do not improve survival or prevent heart attacks. Using stents routinely rather than provisionally has only modest benefits.”
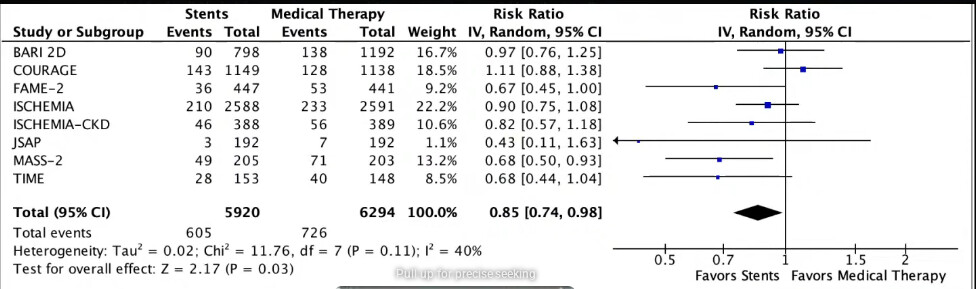
See the image I posted, there’s clearly a 15% reduction in heart attacks, and according to Avi a reduction in total mortality as well.
"The trials included 9918 patients with CHD. How was the study done? The researchers searched the medical literature to find randomized trials that compared coronary stents with PTCA. They found 29 trials that 1) included patients with CHD but no acute heart attack and 2) followed patients for at least 6 months after their procedure. In many trials, patients who had standard PTCA could have a stent if they developed complications or if the PTCA was unsuccessful. This bailout strategy was called provisional stenting. The researchers compared outcomes between groups by using special methods of analysis (meta-analysis). What did the researchers find? The researchers found no differences in numbers of heart attacks, coronary artery bypass surgeries, or deaths between groups. "
That meta analysis were only using trials with older stent technology before they were drug-eluting
And you choose to ignore the error bars of your image.
Argue all you want, my take is that stents preventing heart attacks is not statistically
significant.
End of discussion.
Three of the studies were significant, and we look at the total sum which were.
A recent study published last year showing clear benefit of stents:
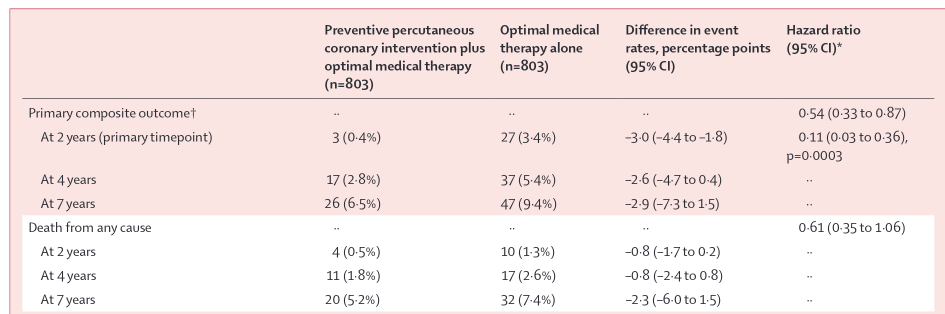
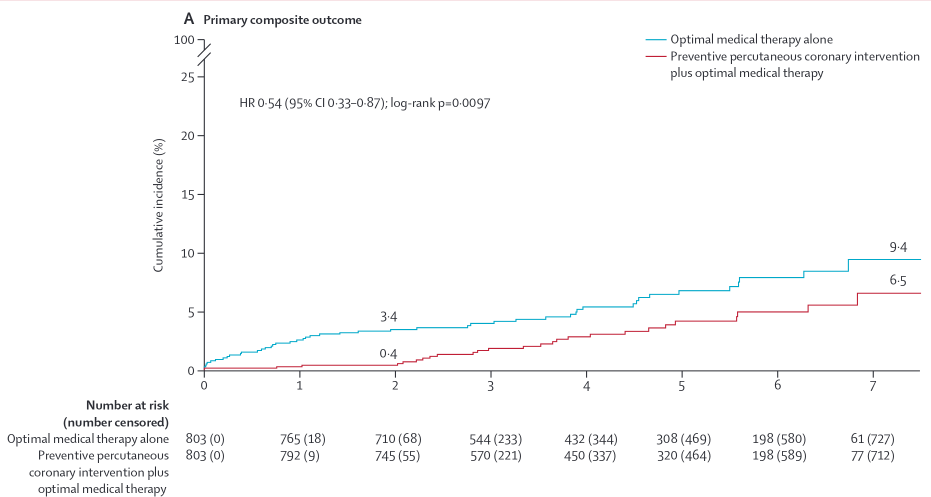
Between Sept 23, 2015, and Sept 29, 2021, 5627 patients were screened for eligibility, 1606 of whom were enrolled and randomly assigned to percutaneous coronary intervention (n=803) or optimal medical therapy alone (n=803). 1177 (73%) patients were men and 429 (27%) were women. 2-year follow-up for the primary outcome assessment was completed in 1556 (97%) patients (percutaneous coronary intervention group n=780; optimal medical therapy group n=776). At 2 years, the primary outcome occurred in three (0·4%) patients in the percutaneous coronary intervention group and in 27 (3·4%) patients in the medical therapy group (absolute difference –3·0 percentage points [95% CI –4·4 to –1·8]; p=0·0003).
Simply reducing events by 89% not bad, and this was also for vulnerable non-flow limiting plaque, trending to a decrease in all-cause death by 40% as well @relaxedmeatball thoughts?
“cobalt–chromium everolimus-eluting metallic stents” is the most cyborg chad sentence ever. The unabomber natural supplementoors have no chance against the cobalt-chromium drug infused stents.
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(24)00413-6/abstract
This is why I find this all so confusing because I have not found a cardiologist (out of only 5) that said they would do a preventative stent, no matter what they saw on a CCTA . @DrFraser says the good ones do and I believe him. I am hoping he answers when you do a CCTA vs a nuclear stress test or vice versa…
I have two nephews who have stents. They both got them to relieve symptoms. Their doctors never told them that they would prevent heart attacks.
“Stents may relieve chest pain (angina), shortness of breath, and fatigue caused by reduced blood flow to the heart.”
Stress test (idk where the ‘nuclear’ came from) is just jogging on a treadmill with some wires attached to you.