Edit: the graph in the preview doesn’t really show the conclusion. The conclusion is that combination therapy is better than statin monotherapy.
Glad I’ve smashed my own LDL-C to lower than 40 mg/dl. If only I can do the same for Lp(a) soon!
Edit: the graph in the preview doesn’t really show the conclusion. The conclusion is that combination therapy is better than statin monotherapy.
Glad I’ve smashed my own LDL-C to lower than 40 mg/dl. If only I can do the same for Lp(a) soon!
It looks to me like most of the effect is driven by Lee et al, which looks like a cohort study.
The largest analysis to examine the best way to lower levels of “bad” cholesterol in patients with blocked arteries shows that they should immediately be given a combination of a statin and another drug called ezetimibe, rather than statins alone. This could prevent thousands of deaths a year from heart attacks, strokes and other cardiovascular diseases.
If it was done early it would be millions of deaths every year.
The age-standardized change is flat, doesn’t that suggest that there has been no increase?
Prof. Banach said, "Cardiovascular disease kills around 20 million people a year worldwide. Based on our previous analysis, we estimate that if combination therapy to reduce LDL-C was included in all treatment guidelines and implemented by doctors everywhere for patients with high cholesterol levels, it would prevent over 330,000 deaths a year among patients who have already suffered a heart attack, and almost 50,000 deaths alone in the U.S.
This is cause enough to advocate for Ezetemibe + statin.
Start everyone on EZ+statin early before they have developed plaque and save 20 million people a year worldwide. This should be a no-brainer, but for some reason it isn’t.
No increase in CVD deaths in any age group, so why would it be HFpEF? It’s most likely just aging population (more people >70yo => higher share of CVD deaths vs other causes of deaths)
https://www.rapamycin.news/t/cardiovascular-health/7459/1720?u=adssx
The effect on all-cause mortality (OR, 0.81; 95% CI, 0.67 to 0.97; P=.02) is insane! Ezetimibe ![]()
You said it. Specifically, “Now, we’ve basically used up the benefits of the improved treatment and the deaths are catching up again.” Though I know you’re going to try and weasel your way out of this.
So a better question is, "what happened in who were turning 40 in 2010 (i.e. those born in 1970).
I don’t find this convincing as an explanation for the sharp reversal in the mortality rate in 2010.
I wouldn’t be looking at what happened in 2010 that suddenly caused a bunch of deaths.
When you see a large change in the mortality rate, you should absolutely look first at the surrounding social or economic or disease factors - unemployment, war, covid, etc.
I don’t need to weasel because what I wrote is still true. If you interpret that as “we are getting worse at treating CVD” then that’s entirely a problem with reading comprehension.
I am reporting what the authors of that statistical analysis study (where the graph came from) and the president of the AHA said when he presented those data. He talked about better AMI therapy (reperfusion), better cholesterol management, smoking cessation as contributing to the decreases, and HFpEF, diabetes contributing to the increase. The sex difference narrowing is because in the 1990s and early 2000s massive efforts were put into educating doctors that women have hearts and get heart disease too.
IMO, it seems that people are trying to imagine that one dramatic thing has happened which can explain everything. If you zoom out the Y axis, the changes are much more modest and noisy. That sudden, skyrocketing spike of 2010 is… nothing more than a return to the 2005 numbers. In fact, women are still better off in 2020 than 2005, according to the graph.
Of course you are entitled to your own beliefs, and if you don’t “buy” this version maybe you can submit your alternative hypotheses and data for peer review somewhere.
“Game-Changing Study on Heart Health and Cholesterol: New Insights Revealed”
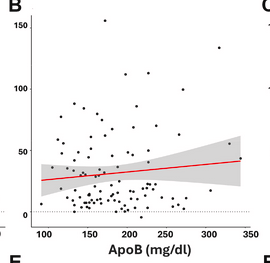
No association between LDL or ApoB and plaque buildup?
“We are confident neither LDL or ApoB were associated with plaque progression.”
This is a very interesting video.
Nick Norwitz: Ph.D., Oxford; MD, Harvard
Short Critique of the KETO-CTA Study
The average ApoB increase over 1y was 3 mg/dL? And they expected to see significant CAC increase with that?!
The study itself is “fine”, but this is a pretty dumb interpretation of it IMO. It’s nowhere near game-changing, and it certainly doesn’t undermine the Apo-B/plaque hypothesis in any way.
It is absolutely a fact that LDL-C/Apo-B contribute towards plaque. However, that doesn’t guarantee that plaque will form or grow linearly every time they are present. Many factors go into whether plaque is formed or regressed or stabilised, including the amount of arterial stress (blood pressure, nitric oxide, smoking etc), how efficient you are at clearing accumulated lipids, the immune response to the plaque, the amount of smooth muscle cell proliferation etc etc. We know the ketogenic diet is “weird” and tends to produce blood tests results far outside of the normal range, and it’s possible that it affects some of those processes in a way which offsets the higher ApoB.
As for the study itself, as the post above says, it’s a small number of people, who are obviously health conscious enough to stick to a keto diet, so it’s a very atypical population. And the followup is only one year, which isn’t long enough to really detect much plaque growth. We can also see in the table that the average participant already has a positive CAC score, thus they already have advanced atherosclerosis, and it’s no surprise that people with higher baselines tend to get worse. If you understand the basic mechanisms of ASCVD, there is absolutely nothing unusual about that, because we know that arterial injury begets more accumulation, which causes more injury, which causes more accumulation…
The discussion section does a nice, honest job of summarising the study. We should all stay away from Youtube videos and social media:
While both LDL-C and ApoB are independent risk factors for atherosclerosis, the absolute risk associated with elevated LDL-C and ApoB is context-dependent, including the etiology of the elevations in these biomarkers as well as interactions with other risk markers
This is well-known in the field for decades. There are kids with familiar hypercholesterolemia who get myocardial infarctions in their teens. And there are people who managed to smoke, drink and have sky-high ApoB their entire lives and never have an MI. A risk factor is just that, and nothing is guaranteed.
Thus, these data are consistent with the observation that high LDL-C and ApoB among a metabolically healthy population have different cardiovascular risk implications than high LDL-C among those with metabolic dysfunction, who constitute a majority proportion of the population
Exactly as I said above.
What kind of changes are we expecting in noncalcified plaque volume (NCPV) if LDL-C or apoB is between 50-60 mg/dl or lower compared to the results in this study over 1 yr with apoB at 180 mg/dl (in a similar population)?
No apoB is below 100 mg/dl, but it looks like half had an increase of 25+ mm3, one person regression, or am using the wrong graph? What would be the result at 30, 40, 50 mg/dl apoB? ![]()
Am I asking the right question?
>on keto diet
>works well
>apoB through the roof, doctor is panicking
>it’s fine though CAC = 0
>no advanced disease yet
>smokers who have lung cancer have more progression in cancer
>no lung cancer, it’s fine to smoke
>see this study showing that smoking for 1 year is only bad if you have lung cancer
>it makes lung cancer worse then
>an advanced bayesian analysis shows that 9x likely that this is the case
>no need for an adequately powered study
>can you believe this
>everyone must see this documentary
>if you have lung cancer see your doctor
Lustgarten Xeeted this (paywalled):
https://academic.oup.com/eurjpc/advance-article-abstract/doi/10.1093/eurjpc/zwaf088/8105613?
Related commentary (not paywalled):
zwaf196.pdf (183.4 KB)
Try probenecid.
https://www.drugs.com/compare/allopurinol-vs-probenecid
Allopurinol has an average rating of 7.4 out of 10 from a total of 91 ratings on Drugs.com. 64% of reviewers reported a positive effect, while 20% reported a negative effect.
Probenecid has an average rating of 9.7 out of 10 from a total of 7 ratings on Drugs.com. 100% of reviewers reported a positive effect, while 0% reported a negative effect.
https://www.jacc.org/doi/10.1016/j.jacc.2017.12.052
In this large cohort of 38,888 elderly gout patients, treatment with probenecid appears to be associated with a modestly decreased risk of CV events including MI, stroke, and HF exacerbation compared with allopurinol.
The commentary is really interesting, and does a good job of balancing the strengths of the study and the wider knowledge in the field. I am personally not yet ready to be convinced that Lp(a) isn’t a risk factor, but, it’s clearly not a simple 1 = 1 type relationship where higher is guaranteed to be worse. That’s good news for somebody like me who fits the demographics of this paper quite well (younger, male, and I’d be in Q5 for Lp(a)).
As we know, some people have horrible circulating lipids but keep a low atherosclerotic burden their whole lives, whereas other people steadily build plaque with ApoB levels of 70mg/dl. There’s a huge amount of factors which go into plaque accumulation, regression and calcification, not just your circulating lipid concentrations. It’s really interesting to see more nuance being added to the overall picture.