Comes from Australia
Thanks I’ll try this first.
Less aggressive than Dayspring and others, but still lower than current standards in many areas:
Open access paper:
Optimal low-density lipoprotein is 50 to 70 mg/dl: Lower is better and physiologically normal
The normal low-density lipoprotein (LDL) cholesterol range is 50 to 70 mg/dl for native hunter-gatherers, healthy human neonates, free-living primates, and other wild mammals (all of whom do not develop atherosclerosis). Randomized trial data suggest atherosclerosis progression and coronary heart disease events are minimized when LDLis lowered to <70 mg/dl. No major safety concerns have surfaced in studies that lowered LDL to this range of 50 to 70 mg/dl. The current guidelines setting the target LDL at 100 to 115 mg/dl may lead to substantial undertreatment in high-risk individuals.
https://www.sciencedirect.com/science/article/pii/S0735109704007168
That’s a really old paper (2004), so surprising to see it here now, I read it about 9 or 10 years ago when I started to learn about this. Old but good.
Ah, my bad. I saw it today on Twitter and assumed it was a new paper.
It’s actually more aggressive than what Dayspring recommends to most people: Cardiovascular Health 2024 - #1436 by adssx
I’ve always found that O’Keefe paper a bit odd. it doesn’t provide any new data but merely collates data from other papers. However… it’s a bit dodgy
If you check out the references they don’t support the 50 to 70 mg/dl figure at all.
The Hunter gatherer paper referenced gives a figure of 202 mg/dl total cholesterol for hunter gatherers
Whereas the O’Keefe paper says:
“Evidence from hunter-gatherer populations while they were still following their indigenous lifestyles showed no evidence for atherosclerosis, even in individuals living into the seventh and eighth decades of life 15, 16. These populations had total cholesterol levels of 100 to 150 mg/dl with estimated LDL cholesterol levels of about 50 to 75 mg/dl”
the fact that they then include the 50 to 70 figure in the title of their paper is terrible science.
Bad news for a new Lp(a) lowering drug
Source:
https://x.com/drlipid/status/1885304735260901458?s=46
Dayspring and Attia on cardiovascular health.
This week, on episode #334 of The Drive, Peter sits down with Tom Dayspring, M.D., a world-renowned expert in clinical lipidology and a previous guest on The Drive.
In this episode, Tom explores the foundations of atherosclerosis and why atherosclerotic cardiovascular disease (ASCVD) is the leading cause of death worldwide for both men and women. He examines how the disease develops from a pathological perspective and discusses key risk factors, including often-overlooked contributors such as insulin resistance and chronic kidney disease. He breaks down the complexities of cholesterol and lipoproteins—including LDL, VLDL, IDL, and HDL—with an in-depth discussion on the critical role of apolipoprotein B (apoB) in the development of atherosclerosis. Additionally, he covers the importance of testing various biomarkers, the impact of nutrition on lipid levels, and the vital role of cholesterol in brain health, including how cholesterol is synthesized and managed in the brain, how it differs from cholesterol regulation in the rest of the body, and how pharmacological interventions can influence brain cholesterol metabolism.
They also discuss:
- Defining atherosclerotic cardiovascular disease (ASCVD): development, risks, and physiological impact
- The pathogenesis of ASCVD: the silent development over decades, and the importance of early detection for prevention of adverse outcomes
- How aging and lifestyle factors contribute to rising apoB and LDL cholesterol levels, and the lifestyle changes that can lower it
- How statins might affect brain cholesterol synthesis and cognitive function, and alternative lipid-lowering strategies for high-risk individuals
- More
I watched/listened today… it hurt my brain ![]()
If you are more or less familiar with the basics of what ApoB is and atherosclerosis, you can safely skip about the first half of this video - nothing new here that hasn’t been beaten to death. More detail and interesting information, in particular about cholesterol metabolizm in the brain is in the second half, and the closer toward the end, the more interesting it got - I certainly learned some new stuff. YMMV.
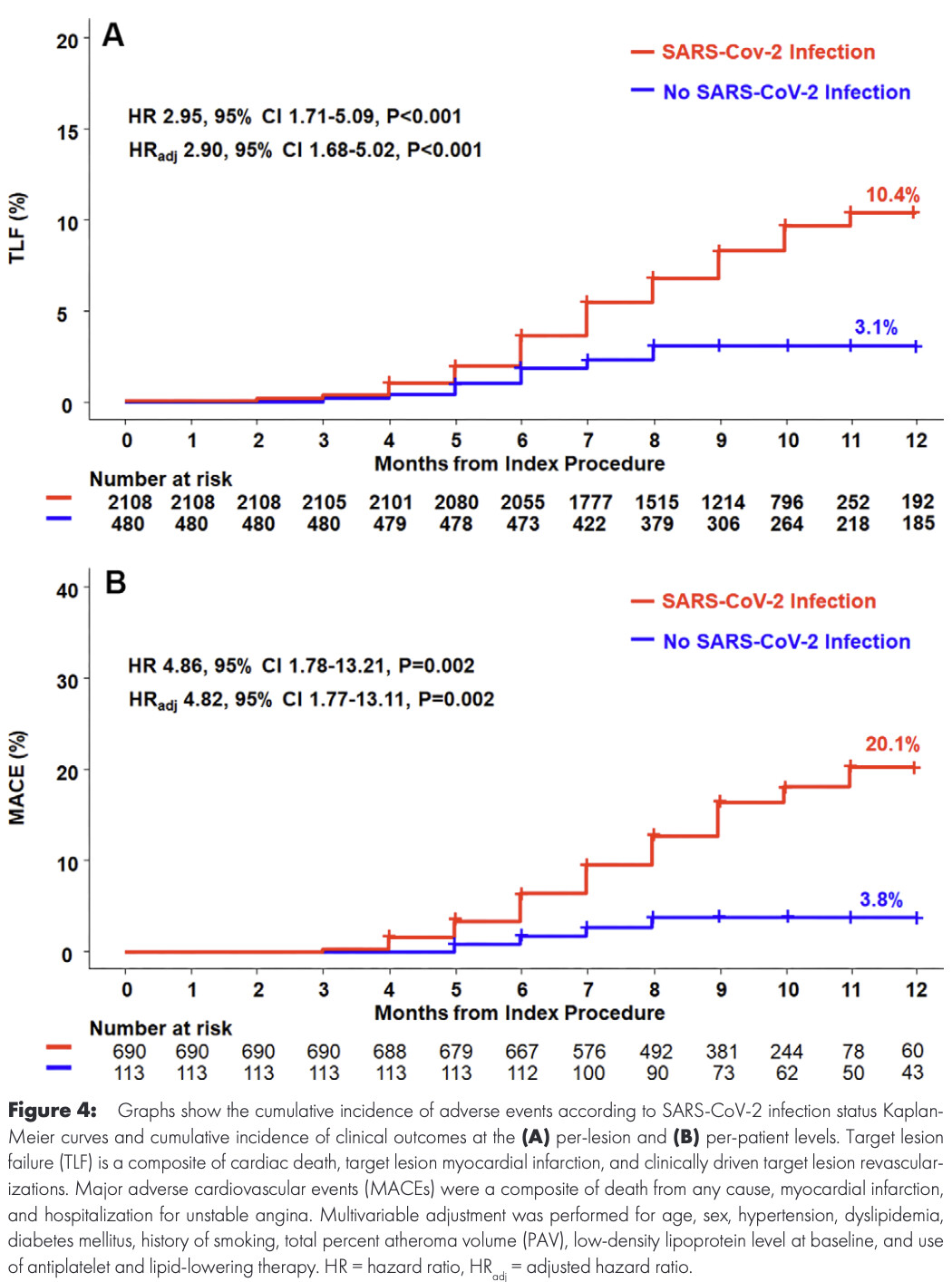
A new study found severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection was associated with the rapid growth of plaque in the coronary arteries and an increased risk of cardiovascular events. The results were published in Radiology .
More information: SARS-CoV-2 Infection Association with Atherosclerotic Plaque Progression at Coronary CT Angiography and Adverse Cardiovascular Events, Radiology (2025).
Open access paper: https://pubs.rsna.org/doi/10.1148/radiol.240876
That’s a timely release, I just tested positive for COVID this morning and I also have severe CAD.
The short summary is that it’s the inflammation that is the likely driver of that increase and that the inflammation can persist for at least 1 year (They don’t have data for a longer period). I found elsewhere that inflammation can persist for 3 years or more.
Inflammation contributed to plaque progression:
• Causal mediation analysis suggested PCAT inflammation accounted for 10.3% of total plaque growth and 5.7% of noncalcified plaque growth .
• Suggests persistent inflammation post-COVID-19 plays a role in coronary disease progression .
The whole paper is interesting BTW.
So let’s test the inflammation (hsCRP) post COVID and make sure it’s back to normal.
Agreed - the first half is a rehash of stuff already covered in this thread. But, I found the talk about the role of cholesterol in the brain very interesting. I’ve lined up the podcast for this section below:
At the end they said no one will fund statin trials to see if they prevent dementia.
The NIH is doing this with PREVENTABLE, cost $70 or 90 M iirc. STAREE in Australia.
Both testing atorvastatin to prevent dementia.
Well, insofar memory formation is implicated in dementia I am not optimistc when it comes to statins:
The Effect of Statin Treatment on Synaptogenesis in the Hippocampus
“Deranged lipid homeostasis has been implicated in neurodegenerative diseases. Cholesterol reducing compounds such as statins have received special attention for the possibility that they may be able to ameliorate or prevent cognitive loss associated with neurodegeneration. However, there is much dissension concerning the actual effect of statins on cognitive function. The aim of this study is to investigate the effects of pitavastatin on hippocampal synaptogenesis because the hippocampus is crucial for memory formation. We also evaluated the effects of pitavastatin on local hippocampal estrogen synthesized in the hippocampus itself and its effect on Brain-Derived Neurotrophic Factor (BDNF). Using a hippocampal cell line, H19-7, we found that hippocampal neurons exposed to pitavastatin demonstrate a significant reduction in the synaptic marker postsynaptic density protein 95 (psd-95). The pitavastatin treated neurons also exhibited decreased production of local estrogen and their expression of BDNF mRNA was decreased. These results suggest that statins reduce the ability of hippocampal neurons to form synapses by restricting the production of local estrogen. Because neural connections in the hippocampus are crucial for memory formation, our findings implicate statins as medications that may compromise cognitive function.”
Mechanistic, in vitro, studies are second lowest on the evidence hierarchy. It can pretty much be thrown in the garbage bin for that reason.
Which is why I don’t think it’s dispositive, but I’m not optimistic. Of course, I’m awaiting trials, but not holding my breath. YMMV.
As non-primary endpoint in trials all statin trials have either had a neutral or positive effect on dementia. The largest study ever being done in older adults in America is atorvastatin, so they have a good reason for choosing it. Who knows.
The acetyl-coa metabolism is clearly relevant to memory formation.