None of that is statistically significant. Better powered RCTs are needed.
Right, which is why I call it a signal. Still disturbing, I’d rather the signal be in the opposite direction. But yes, we need rcts, no question.
And we have the RCTs. And as far as I know SGLT2i perform very well in this subgroup (that is I guess the majority subgroup in heart failure and CKD for which the drugs are approved).
Why? We’re targeting hallmarks of aging, not targeting cardiovascular only? What about preventing potentially hundreds of thousands of errors and damage from occurring? Am I missing something?
Association of SGLT2 Inhibitors with Incident Cancer: SGLT2i and Incident Cancer 2024
SGLT2i administration was associated with a reduced risk of cancer (HR 0.80, 95% CI 0.70-0.91). Particularly, SGLT2i administration was related to a lower risk of colorectal cancer (HR 0.71, 95% CI 0.50-0.998). […] The risk of developing cancer was comparable among individual SGLT2is (P-value of 0.1738).
Our investigation using nationwide real-world data demonstrated the potential advantage of SGLT2i over DPP4i in reducing the development of cancer in individuals with diabetes.
Am I reading this right: they followed the cohorts for 2+/-1.6 years, so a maximum of 3.6 years, and the SGLT2i users hazard ratios were 20% less? That seems inordinately dramatic lowering over a span of less than 4 years (minimum even more absurd 0.4 years). Furthermore, for colorectal cancer it’s as drastic as some 30% - CRC takes roughly 10 years to develop from a polyp, and here the studied population was newly prescribed patients for both drugs, so it’s not like they were on the drugs for 10+ years, and only observed for the last 2+/-1.6 years. That would imply that some had perhaps precancerous or cancerous polyps, and the SGLT2i prevented the polyps from turning diagnosable CRC.
I don’t have access to the full study, but I’m very unclear how to read this based on the abstract.
Long-Term Effects of Empagliflozin in Patients with Chronic Kidney Disease 2024
In a broad range of patients with chronic kidney disease at risk for progression, empagliflozin continued to have additional cardiorenal benefits for up to 12 months after it was discontinued.
(@Neo: confirms that your idea of intermittent use might be beneficial)
Regression of plaque burden: Cardiovascular Health - #1374 by adssx
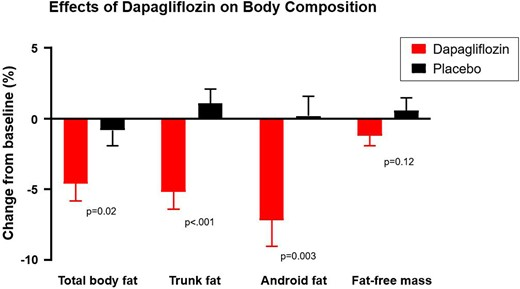
In patients with HFpEF, dapagliflozin decreases body fat, particularly trunk fat, suggesting greater effect on visceral adipose, which is correlated with favorable hemodynamic effects. Dapagliflozin also tends to reduce FFM, which may relate to reduction in total body water with or without reduction is muscle mass, in tandem with modest decreases in bone mineral content.
That’s good news!
After further adjustment for age, sex and comorbidities, those with SGLT2I had a lower adjusted hazard ratio of mortality (aHR: 0.64 [95% CI: 0.60–0.68]). We conclude that SGLT2I medication should be considered first choice in patients suffering from DM and cancer.
The SGLT2i’s look so promising, but so do the GLP-1 agonists. Acarbose seems like a great addition also to Rapa among others for its potential effects on mTORC2, and the ITP results of course.
I’m just wondering if/how members use these 3, if at all. Combining them would increase the risk of DKA and DK, hypoglycemia. But each class of drugs have different mechanisms of action, each has their own (potential) benefits, and while there is some overlap, they are not entirely redundant.
The suggestion to use SGLT2i intermittently is interesting, but also inconclusive at this stage.
As far as I know, combining SGLT2i and GLP-1RAs does not increase the risk of DKA, DK, and hypoglycemia. It might even lower the risk according to these papers:
- Adverse event reporting of combining SGLT2 inhibitor and GLP1 receptor agonist: a real-world study from FAERS 2024: The results showed that the PRR of SGLT2i-related adverse events including diabetic ketoacidosis (DKA), ketosis, reproductive tract adverse events, urinary tract infection, and other adverse events, decreased in individuals using both SGLT2i and GLP1RA compared with those using SGLT2i alone, and the signal of fracture was not detected.
- Cardiovascular, Kidney and Safety Outcomes with GLP-1 Receptor Agonists Alone and in Combination with SGLT2 Inhibitors in Type 2 Diabetes: A Systematic Review and Meta-Analysis 2024: “Serious adverse effects and severe hypoglycemia were also similar regardless of SGLT2 inhibitor use (P-heterogeneity=0.29 and 0.50, respectively).”
Adding acarbose to the mix might increase the risk, but I don’t think we have data on that.
First thing these agents are for Type 2 Diabetics, who generally don’t get DKA unless they actually have Type IIIC Diabetes. I’ve not seen a single case of a patient on mono or dual therapy with these agents with DKA or hypoglycemia, UNLESS they are on another agent than can cause hypoglycemia (e.g. insulin or a sulfonylurea). Not so say it has never happened, but I’ve worked in high volume urban ER’s, including big regional hospitals for 25+ years and if this complication happens - they are seen and diagnosed in the ER.
So my personal experience would be to not be worried about a complication that is so rare, I’ve never seen it.
You are right, data is lacking. But it is likely also uncommon for patients to use SGLT2i, acarbose and a GLP1 combined. I only found this case study of Asian patients with T2D that developed DK, while on high dose acarbose and a SGLT2-i. https://jcimcr.org/pdfs/JCIMCR-v5-2950.pdf
Ahh this is a big nothing. Ketosis without acidosis? Who cares. That’s my present state right now, haven’t consumed calories today and will have ketosis. A truly irrelevant publication.
Of all the things that go into a diagnosis of DKA, ketones are the easiest and least specific. They are necessary for the diagnosis, but it is so easy to get ketones in one’s urine.
We only clinically care about this when there is metabolic derangement and build up of blood ketones to where there is a acidosis (minimal criteria are Glucose untreated of >250 mg/dL, Arterial pH<7.30, Bicarbonate of <18, Ketones measured in blood or urine, Anion Gap>10). By far, the most important is the degree of acidosis.
So ketones without acidosis is something I see frequently in people on no meds, in diabetics, etc. I ignore it as it is easy to get and I’ve never seen any health consequences from it. Every person on a keto diet would gain this authors interest as they’d have exactly the same findings.
A related question, but a bit different. From all I have read it seems that maintaining a low/normal fasted glucose level as well as maintaining as low as possible a spike (after food intake) is very important for health.
Since these SGLT2-i and GLP1 seem to be in the spotlight nowadays, I was wondering what is the opinion (if any) on the relation between longevity and having/maintaining low glucose levels? Has this been explored/tested on? e.i. people that naturally had lower G levels lived longer, or people who were on these lowering G level drugs lived longer etc…
Thanks Dr.Fraser, for your insights. You’re right of course that in healthy individuals with normal insulin function, ketosis is usually self-limiting. But what I’m concerned about is whether a combination of an mTOR inhibitor such as Rapa with 3 types antidiabetic medications could increase the risk of hypoglycemia. And research suggesting Rapa has been associated with glucose intolerance and insulin resistance. That made me wonder if such potential metabolic disturbances could increase the risk of DKA.
Also since I’m unsure how an individual on (higher) doses of Rapamycin may be able to respond to metabolic stress, such as low glucose availability, by regulating ketone production and utilisation. But perhaps I’m overthinking this. And granted, I’m resorting to case studies. Then again: how many patients have been using such drug combinations.
https://diabetesjournals.org/care/article/47/1/140/153876/Euglycemic-Ketoacidosis-in-Two-Patients-Without
I use Jardiance 10mg in the morning, 100mg Acarbose before lunch and dinner (does not eat breakfast ) and 850mg Metformin before bed time. No problems at all. Previously pre diabetic, now I am a long way away from that.
You can see insulin resistance on a cyclical basis with my second high dose topic. This is then followed by high insulin production which causes lower glucose (but not for me hypoglycemia). Then that fades, but I start the cycle again.
Thanks a lot, John, those are interesting observations. Is it possible to draw any conclusions how long approximately the insulin resistance lasts for you after taking such a high dose?
Thanks for sharing Goran. Both SGLT2i and GLP-1RA have glucose-dependent actions, so perhaps it’s indeed not really an issue. Adding the acarbose makes me wonder a bit.
Good to hear you’re not experiencing any issues while taking a pretty high dose of Acarbose with Jardiance and Metformin.
Per previous discussions/studies (somewhere way earlier in the thread), it was concluded that most SGLT2i drugs (with the exception of canagliflozin, since it also blocks SGLT in the intestines) actually don’t acutely reduce postprandial glucose spikes. Empa and dapa act in the kidneys to help dump glucose, but this happens too late to affect the post-meal spike.
Perhaps over time, with loss of visceral fat and increased insulin sensitivity, all of the SGLT2i drugs would indirectly help w/postprandial glucose spikes to some extent, if a person were previously insulin resistant (?)
got you, but I thought acarbose is supposed to do that? that’s why I was wondering if maintaining a low (post food) G level is one of Acarbose’s mechanisms for longevity (as opposed to just microbiome health)