More good news: Empagliflozin slows down natural kidney senescence via Six1/Wnt4/NF-κB pathway 2025
We included 18 cohort studies (1,164,774 participants). In cohort studies, combination therapy was associated with a lower risk of MACE (RR 0.56 [95% CI 0.43, 0.71]; low certainty of evidence) and the kidney composite endpoint (RR 0.48 [95% CI 0.32, 0.73]; very low certainty of evidence) relative to SGLT2 inhibitor or GLP-1 RA monotherapy. Combination therapy was also associated with a lower risk of all-cause mortality (RR 0.50 [95% CI 0.40, 0.63]; low certainty of evidence), cardiovascular mortality (RR 0.26 [95% CI 0.16, 0.43]; low certainty of evidence) and hospitalisation for heart failure (RR 0.67 [95% CI 0.64, 0.71]; moderate certainty of evidence).
Pretty good.
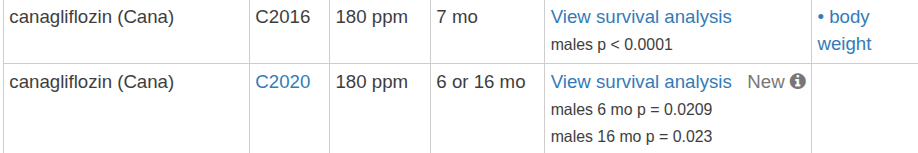
An SGLT2 drug, Jardiance, is now among the top ten Medicare drugs by total expenditure — and the SGLT2 inhibitor class did very well in the ITP mouse longevity studies, which I believe is a first.
So it’s clearly a valuable class and one I’ve put on my “must-have” list. If push came to shove, I’d spring for the branded American version, but I had been using Indian dapagliflozin, which recently ran out. Fortunately, I just got a prescription for another of the flozin family, bexagliflozin.
I ordered the bexa through AgelessRX — they were extremely easy to work with. I even entered the wrong address by mistake (auto-fill), and they replaced the shipment free of charge. Their prices are reasonable, and the customer service has been excellent. Highly recommended.
Depending how these numbers are intrepreted, we’re talking a top 3 ITP drug. So yeah, I’m in.
Tom, can you share the price that AgelessRX charges for bexagliflozin?
It was $125 a month, so $4 a pill. At some point I might approach my regular PCP about it. It would be nice to have all my medicines with one physician, but rapa? E3? 17alpha? ain’t never gonna happen. But these glifozins aren’t that weird. I think bexa is $50 per month at Cuban’s Cost Plus Drugs.
Intranasal insulin and empagliflozin were safe alone or in combination for mild cognitive impairment/AD.
Insulin improved cognition and markers of inflammation and immune function.
Empagliflozin reduced markers of vascular injury and neurodegeneration.
A longer, larger trial is needed to validate these results.
Press: New trial finds two commonly available drugs may delay Alzheimer’s 2025
“For the first time, we found that empagliflozin, an established diabetes and heart medication sold under the brand name Jardiance, reduced markers of brain injury while restoring blood flow in critical brain regions,” said Suzanne Craft, an author of the study from the Wake Forest University School of Medicine.
“We also confirmed that delivering insulin directly to the brain with a newly validated device enhances cognition, neurovascular health and immune function,” Dr Craft said.
“Because empagliflozin or intranasal insulin improved tau tangles, cognition, neurovascular health and immune function, we believe these treatments could offer real therapeutic potential, either on their own or in combination with other Alzheimer’s therapies,” she added.
Which ones? AllDayChemists is still shut down, and I’m out of canagliflozin.
Maulik is shipping
Thanks! Can’t find anything on “maulik” with Google. Any additional details?
See Maulik info here: A Combination of Rapamycin and Trametinib Extended Maximum Lifespan by up to 35% - #129 by RapAdmin
https://alz-journals.onlinelibrary.wiley.com/doi/10.1002/alz.70639
Our findings are in agreement with and enhance other real-world observations on GLP-1 receptor agonists, SGLT-2 inhibitors, and AD. In our study, compared to DPP-4 inhibitor initiation, we find HRs ≤ 0.69 (P values ≤ 0.001 [Figure 1]) for GLP-1 receptor agonist initiation and SGLT-2 inhibitor initiation. In a recently published study using Florida-based (i.e., a US state–based) EHR data, compared to other second line antidiabetic drugs (e.g., DPP-4 inhibitors, sulfonylureas, thiazolidinediones, etc.) initiation, the HRs were ≤ 0.67 (all P values < 0.05) for GLP-1 receptor agonist initiation and SGLT-2 inhibitor initiation
Probably one of the better review articles comparing of GLP1 vs SGLT2 for Alzheimers, since it differentiates between GLP1 and DPP 4 inhibitors (I’ve seen reviews that for some reasons lumped DPP4 inhibitors and GLP1 agonists in the same basket, and then comparing them to SGLT2 inhibitors ) . I would like to see a more refined comparison that distinguishes between long acting vs short acting GLP1 agonists in the future (when comparing them to SGLT2 inhibitors) , on future studies on heart, kidney, liver disease.
Is rapamycin an SGLT2 inhibitor?! University of Mississippi paper: mTOR blockade prevents progressive proteinuria but induces hyperglycaemia in obese Dahl salt-sensitive rats before puberty 2025
Interestingly, we observed that renal sodium glucose cotransporter 2 (SGLT2) expression was significantly elevated in SSLepRmutant rats versus SS rats, and rapamycin markedly reduced renal SGLT2 expression in SSLepRmutant rats. Overall, these data indicate that mTOR plays an important role in renal metabolic disease in obese SSLepRmutant rats before puberty and suggest that rapamycin might prevent renal hyperfiltration associated with obesity by decreasing renal SGLT2 activity.
Our study shows that hyperinsulinaemia-driven mTORC1 activation and SGLT2 upregulation contribute to early renal injury in obesity, independent of hyperglycaemia. Rapamycin reduced insulin levels, downregulated SGLT2, lessened renal injury and increased anti-inflammatory cytokines (interleukin-4 and interleukin-10). These findings highlight mTORC1 inhibition as a potential early intervention for obesity-related renal disease in children, moving beyond traditional blood pressure and glucose control.
Additionally, the renal protective effects of rapamycin were accompanied by significant reductions in renal SGLT2 expression in SSLepRmutant rats. The most interesting finding was that chronic treatment with rapamycin reduced plasma insulin levels and stimulated hyperglycaemia.
Second, in SSLepRmutant rats, rapamycin-induced hyperglycaemia was accompanied by reduced renal expression of SGLT2, leading to increased sodium excretion and potentially preventing any rise in arterial pressure. These findings suggest that the arterial pressure response to rapamycin might depend on age and dietary salt intake.
Prior studies have shown that insulin enhances SGLT2 activity (Nakamura et al., 2015), which can impair the tubuloglomerular feedback response and increase GFR (Gérard et al., 2022). In the present study, elevated insulin levels in vehicle-treated SSLepRmutant rats were associated with increased creatinine clearance and renal SGLT2 expression. Treatment with rapamycin reduced insulin levels, renal SGLT2 expression and GFR. These findings suggest that insulin-stimulated SGLT2 expression might contribute to renal hyperfiltration in non-diabetic, obese children with early renal disease.
Together, these findings suggest that rapamycin might protect against obesity-related renal injury not by lowering blood glucose, but by disrupting the insulin–SGLT2–hyperfiltration axis.
Our findings suggest that hyperinsulinaemia-induced activation of mTORC1 and increased SGLT2 expression might contribute to early renal injury in obesity, independent of hyperglycaemia. Rapamycin attenuated these effects by reducing insulin levels, downregulating SGLT2 and decreasing markers of glomerular and tubular injury. This highlights a potential therapeutic role for mTORC1 inhibition in early-stage renal disease, particularly in the context of hyperinsulinaemia-driven renal dysfunction. Moreover, the observed anti-inflammatory effects of rapamycin, including increased renal IL-4 and IL-10, further underscore its promise as a new therapeutic strategy.
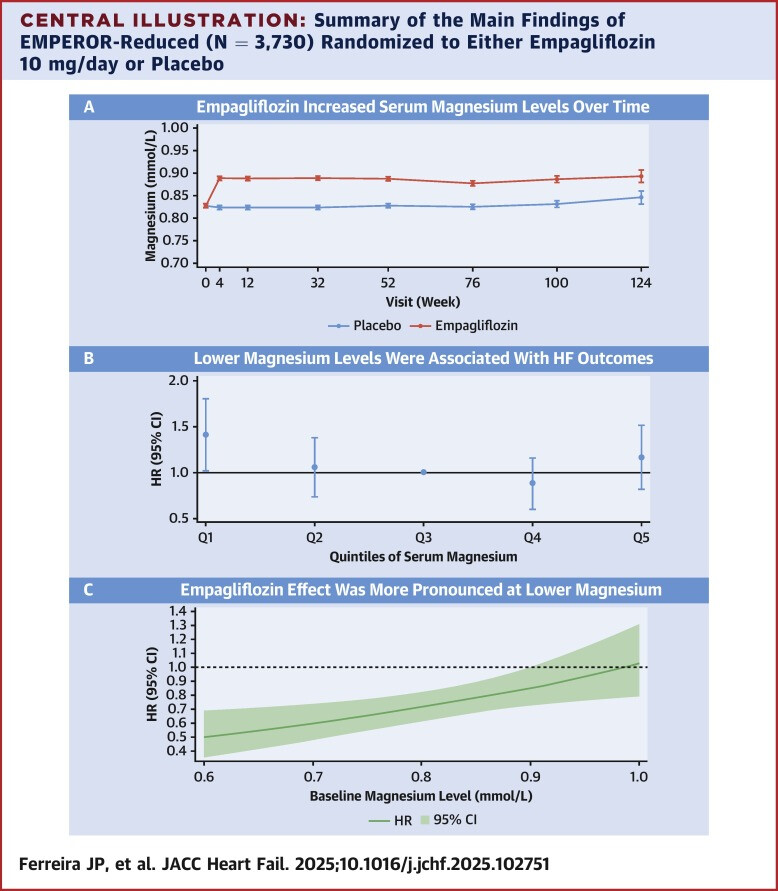
Empagliflozin rapidly increased magnesium levels by 0.05 mmol/L. The relative odds of experiencing lower magnesium levels were reduced with empagliflozin.
Interesting because this replicates the findings of an earlier study. It’s basically a magnesium supplement too.
Boy, that’s a very looooong limb to go out on. I’m not saying it can’t be relevant - as the authors speculate - to “obese prepubescent children with early renal disease”, but as they also note in those particular rats (SSLepRmutant) SGLT2 expression is very elevated to begin with. I suspect many things can interfere with such already very elevated SGLT2 expression, and I’m not sure how that would look in normal level SGLT2 expression, would rapamycin still inhibit SGLT2? Also, as noted this is effect of rapamycin is downstream from the insulin-hyperglycemia axis, so how relevant it’s going to be in normoglycemic normal level insulin, I don’t know.
It’s interesting, but not something I’m going to get super excited over, as my ambition is to lower insulin levels and also glucose levels. Rapamycin here might be orthogonal to those who already use an SGLT2i, such as empagliflozin (as I do). YMMV.
SGLT2 Inhibitors and Kidney Outcomes by Glomerular Filtration Rate and Albuminuria
https://jamanetwork.com/journals/jama/fullarticle/2841163
"Key Points
Question Do the kidney protective effects of sodium-glucose cotransporter 2 (SGLT2) inhibitors vary by estimated glomerular filtration rate (eGFR) or albuminuria?
Findings In this meta-analysis that included 70 361 participants in 10 trials of SGLT2 inhibitors vs placebo, SGLT2 inhibitors significantly reduced progression of chronic kidney disease (CKD), serious acute kidney injury, and kidney failure. The relative risk reduction for CKD progression was consistent regardless of eGFR and albuminuria. Significant reductions in the annual rate of eGFR decline were observed across all subgroups, including when participants with and without diabetes were analyzed separately.
Meaning These findings support the routine use of SGLT2 inhibitors to improve kidney outcomes across the full spectrum of kidney function and albuminuria among patients with type 2 diabetes, CKD, or heart failure."
What do you think about this study? My own experience is that dapagliflozin caused me anxiety. I might try again at some point, perhaps with empagliflozin.
https://www.sciencedirect.com/science/article/pii/S2213398424000514
T2DM patients taking SGLT2 inhibitors exhibited significantly higher levels of thyroid-stimulating hormone (TSH) compared to controls (p < 0.001). Additionally, T2DM patients on SGLT2 inhibitors showed a higher prevalence of mild to moderate depression (p < 0.001, odds ratio = 1.74) and cognitive impairment (p = 0.039, odds ratio = 1.32) compared to controls. Subgroup analysis revealed varying effects among different SGLT2 inhibitors on depression and cognitive function
To be clear, the subjects taking an SGLT2i had a history of diabetes while the controls were healthy subjects without a history of diabetes. This is not a study of two randomized groups of healthy subjects where one group took an SGLT2i and one did not. It was also not a study of two randomized subjects with T2DM where one group took an SGLT2i and one did not.
Indian paper = trash most of the time. IIRC, other studies looking at SGLT2 and depression found benefits or neutral.