I bought this one, but there is many options.
Metformin, thiazolidinediones, pioglitazone, GLP1RAs and SGLT2is were associated with significant reduction in risk of dementia. When studies examining metformin were divided by country, the only significant effect was for the United States. Moreover, the effect of metformin was significant in Western but not Eastern populations. No significant effect was observed for dipeptidyl peptidase-4 inhibitors, α-glucosidase inhibitors, or insulin, while meglitinides and sulphonylureas were associated with increased risk.
Metformin, which remains the first-line medication for the management of type 2 diabetes, did show benefits for dementia risk in our meta-analysis, yet newer treatments may confer greater risk reduction for dementia; this finding is of importance, given the extensive use of GLP1RAs and SGLT2is in clinical practice at present.
The meta-analyses showed an overall protective effect of:
metformin [RR 0.83 (0.71-0.96)],
thiazolidinediones [RR 0.770 (0.593-0.999)],
pioglitazone [RR 0.74 (0.55-0.98)],
GLP1RAs [RR 0.35 (0.16-0.78)] and
SGLT2is [RR 0.39 (0.20-0.76)] on risk of dementia.
DPP-4is, α-glucosidase inhibitors and insulin had a neutral effect on risk of dementia, while meglitinides and sulphonylureas were associated with increased risk.
Yet another study that found that for dementia prevention, acarbose is useless (“neutral”), while GLP1RAs and SGLT2is seem magical. Metformin is “meh”, especially useless for Asians.
You’ve convinced me. The next Med I’ll add is empagliflozin or canagliflozin.
Your are really driving my interest in SLG2i. ![]()
Have you found anything negative? Because I know a lot of doctors and they seem not as convinced as you… but I have a box of Jardiance (Empaglifozin) sitting in my cupboard for a while now. Maybe I should give it a try.
My main concern or maybe is just my obsessiveness is trying to figure out how many calories are you loosing via glucose excretion. I am currently doing CR(ON) of 10% and this keeps my weigh stable and adding Empaglifozin would effect this balance?
I also was wondering if I could take it intermittently (EOD) and if I could do it half of 25mg pill.
Haha, actually, I’m not trying to convince anyone other than myself… For context, I’ve had issues with my glucose levels, especially reactive hypoglycemia. Acarbose improved the situation, but not enough. I suggested a GLP1RA to the doctor (based on this paper + their overall positive effects) to which he answered: “GLP1 will increase your insulin, you have reactive hypo, you don’t want more insulin” and prescribed an SGLT2i. Before starting it, I did my research and the more I looked, the more impressed I was. So I started dapagliflozin (5 mg, then 10 mg per day). I’ve been taking it for exactly 1 month now, and, I don’t want to jinx it, but I feel way better…
Here are all the “negative” things I’ve found:
- UTIs and fungal infection: we discussed it a lot. The risk seems limited among non-diabetic people with good hygiene and can be limited even further with cranberry products. I started taking cranberry pills, I hope they’re as effective as cranberry juice,
- DKA: risk seems non-existent in non-diabetic people, but those on a keto diet should look further at this,
- It’s recommended to stop them 3 days before surgery because of DKA risk after fasting for surgery (Figure 1 is nice btw): I’m OK with that,
- Lipid profile: SGLT2-inhibition increases total, LDL, and HDL cholesterol and lowers triglycerides: Meta-analyses of 60 randomized trials, overall and by dose, ethnicity, and drug type 2023 but “Overall, changes were modest and not likely to be of clinical relevance.” (according to DrLipid, it’s “not an issue”)
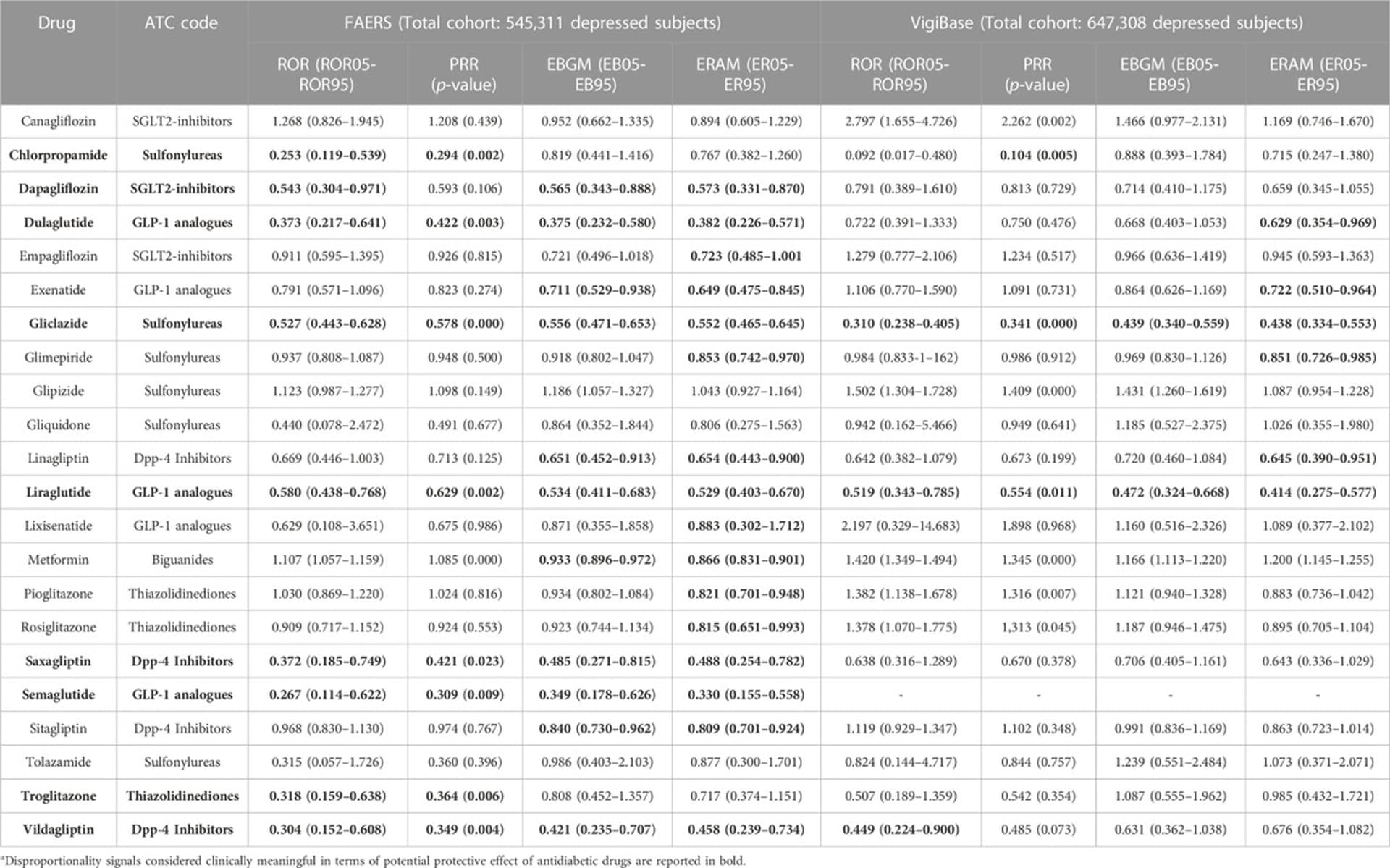
- It’s unclear which one is “best” between cana, dapa, empa, and others. My understanding so far that is they’re overall identical but there might be subtle differences for some applications (for instance, dapa might be potent to prevent depression: The potential antidepressant effect of antidiabetic agents: New insights from a pharmacovigilance study based on data from the reporting system databases FAERS and VigiBase 2023, while cana and empa might be better for PD: Repurposing the inhibitors of MMP-9 and SGLT-2 against ubiquitin specific protease 30 in Parkinson’s disease: computational modelling studies. 2023)
- Some early studies (2014, so 1y after their approval) reported an increase in PTH and bone fractures: SGLT2-inhibitors Trigger Downstream Mechanisms That May Exert Adverse Effects Upon Bone 2014. However, two serious meta-analyses (one Italian and one Chinese) from last year concluded that there was no elevated risk: Effect of SGLT2 inhibitors on fractures, BMD, and bone metabolism markers in patients with type 2 diabetes mellitus: a systematic review and meta-analysis 2023 and Adverse effects of sodium-glucose cotransporter-2 inhibitors in patients with heart failure: a systematic review and meta-analysis 2023
- Increased urinary frequency during the day, but not at night (I noticed this as well, which I think is not so bad because I was not drinking enough water before, now I drink more): Changes in overactive bladder symptoms after sodium glucose cotransporter-2 inhibitor administration to patients with type 2 diabetes 2018
- SGLT2is inhibit mTOR, so should you cycle them? What’s the optimal dose? Are lower doses better? (the ITP is now testing a lower dose of cana) However, I don’t know how their mTOR inhibition potency compares to rapamycin. Daily SGLT2i is maybe like microdosing rapa, I don’t know.
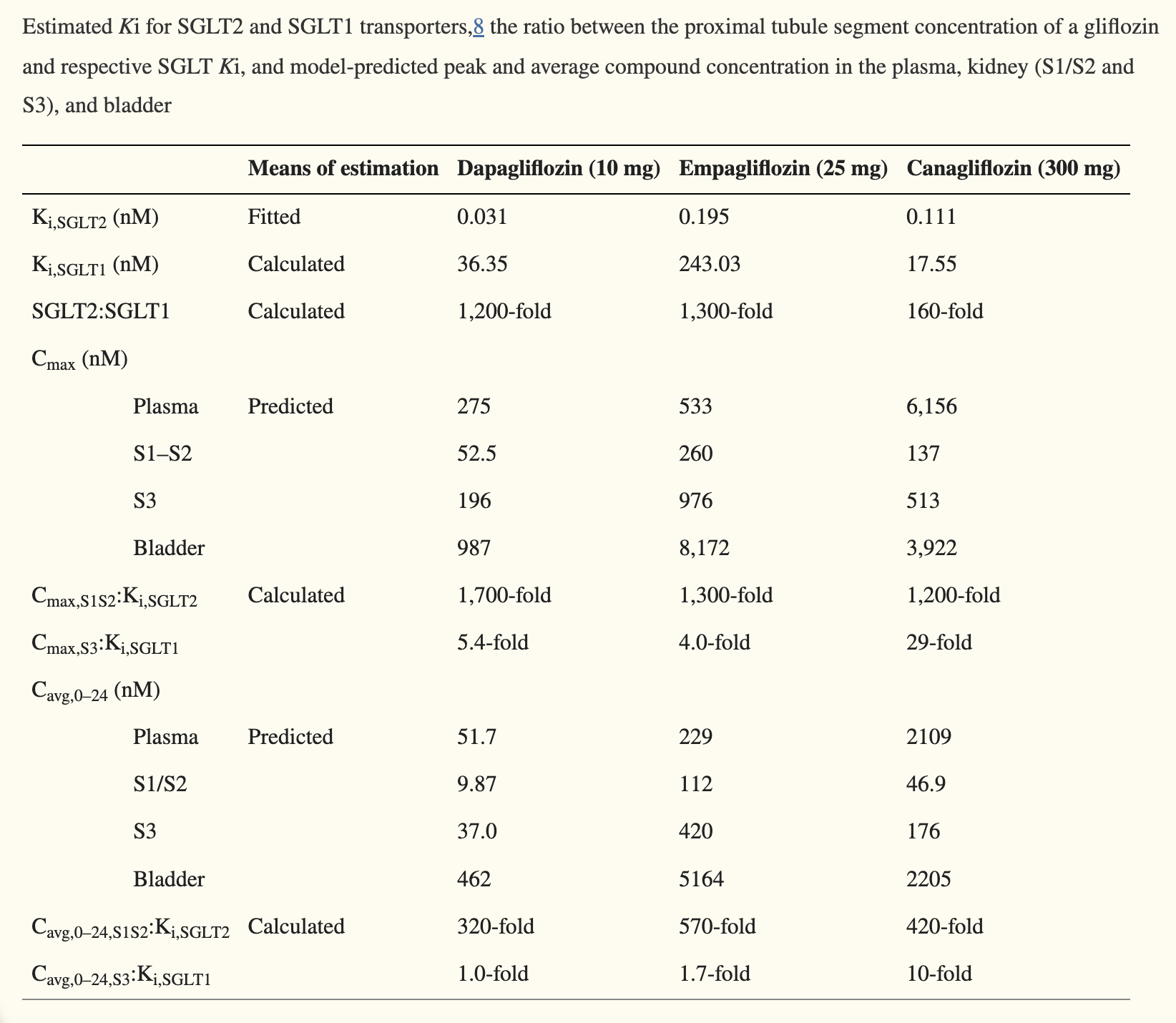
One difference — that I don’t know how meaningful — is that Cana is also SGLT1i not only SGLT2i, while the other main ones are just SGLT2i I believe.
(And we don’t know how much the SGLT1i was behind the ITP results)
Not sure how much to weigh that, but it is nudging me towards Cana until more data on that comes out.
@adssx do you have a sense for what direction it takes for mTORC2? See this decedent discussion:
I have the opposite reasoning ![]() Because empagliflozin and dapagliflozin are highly selective for SGLT2, I feel like they’re safer (and they seem to be, based on trials and longitudinal data). But there’s really not enough evidence around this.
Because empagliflozin and dapagliflozin are highly selective for SGLT2, I feel like they’re safer (and they seem to be, based on trials and longitudinal data). But there’s really not enough evidence around this.
I know nothing about mTORC2, but this 2023 paper concludes: mTORC1 and SGLT2 Inhibitors-A Therapeutic Perspective for Diabetic Cardiomyopathy - PubMed
Further studies are warranted to establish the underlying cardioprotective mechanisms of SGLT2is under diabetic conditions, with selective inhibition of cardiac mTORC1 but the concomitant activation of mTORC2 (mTOR complex 2) signaling.
I haven’t payed much attention to these drugs yet but I will soon since they look so promising.
But do you mean because that the mechanism of action is more clean? (It’s less of a dirty drug). And as you say based on trials and longitudinal data as well.
Canagliflozin binds to SGLT2 and a bit SGLT1. Sotagliflozin binds to both well. All others (including dapa and empa) bind to SGLT2 only. I think I posted a few papers previously showing that empa and/or dapa had better positive effects and fewer adverse events than cana. But nothing super convincing yet.
Canagliflozin would have to be shown to be much better than the others for me to take it again. I put up with an uncomfortable lower digestive system with canagliflozin for months before I stopped taking it.
Correct me if I’m wrong but you switched to empa and did not experience such issues, right? or maybe was at @admin who said that?
Reason for my chime in, I’m about to place my first order of empa.
I switched to Empa because I had some sort of “exhaustion” side effect with Cana. its a pretty rare side effect, from my research, so I moved to Empa. Empa has been fine with no obvious side effects. But for anyone else, this likely is not a reason for Empa over Cana.
Yes, I have switched to empa with no discernable side effects.
I’m not sure it is the opposite - we both acknowledge the following I think
-
Cana may have some more risks on diabetic patients based clinical data
-
Cana but no other SGLT2i or other SGLT1i has been tested in ITP multiple times and each time been successful
-
Cana is both SGLT2i and SGLT1i and the other SGLTi’s that people are taking her on the forum are generally “pure” SGLT2i
-
We cannot know for sure if the SGLT1i part was needed for the Cana ITP longevity results to have been consistently reached
Perhaps the summary is
Cana in “expected” space is perhaps higher risks and higher longevity benefit, while E and D might have longevity benefits and might be safer (if you are a diabetic).
The gut does seems to be involved with a lot of longevity things - including in the case of Acarbose and it seems like that may be one of the big differences:
SGLT1 is primarily expressed in intestinal epithelium, whose inhibition reduces dietary glucose uptake, whilst SGLT2 is highly expressed in kidney regulating glucose reabsorption.
And/or stopping the update might be different that regulating reabsorption down stream
Does anyone have access to:
Does anyone know which SGLTi Peter Attia uses? and/or which one his clinic prefers to prescribe?
—
Also found the below interesting with respect to above:
Summarizing what we know about canagliflozin:
- We don’t know whether the positive effect of canagliflozin is due to its impact on glucose, SGLT2, or SGLT1
- The literature is showing, for example… effect on tumors specifically, and other things like heart attacks, independent of whatever’s happening in terms of glycemic control
- The shortest, simplest explanation—that the benefits are due to canagliflozin’s effect on glucose—may not be right. — “There are other ideas that deserve a lot of exploration.”
- Peter reiterates his excitement around canagliflozin: “We are very excited about this class of drugs clinically in our practice; the cardioprotection, renal protection, obviously the glycaemic benefits are all pretty exciting.”
I wasn’t clear enough: I think that besides higher risks, cana might have lower longevity benefits. Indeed, canagliflozin does not seem to perform significantly better than empagliflozin and dapagliflozin in clinical trials and longitudinal studies for T2D, CKD, HF, etc.
Here’s one example among many others: cana seems to be associated with an increased risk of depression while dapagliflozin slashes depression risk by 2: The potential antidepressant effect of antidiabetic agents: New insights from a pharmacovigilance study based on data from the reporting system databases FAERS and VigiBase 2023
It’s just one longitudinal study, so it does not prove much, but there are several signals like this. I have yet to find one study where canagliflozin strongly outperforms dapagliflozin and empagliflozin.
It’s also interesting to look at the number of clinical trials currently recruiting:
- cana: 15 studies
- empa: 97
- dapa: 109
It seems that researchers all around the world are 10x more excited by empagliflozin and dapagliflozin than by canagliflozin.
We actually know for sure that SGLTi benefits are not due primarily to their effect on glucose: in longitudinal studies, when compared to other glucose-lowering drugs such as DPP4, they perform way better: Sodium-Glucose Cotransporter 2 (SGLT2) Inhibitors vs. Dipeptidyl Peptidase-4 (DPP4) Inhibitors for New-Onset Dementia: A Propensity Score-Matched Population-Based Study With Competing Risk Analysis 2021
Similarly, SGLTi are approved for CKD and heart failure, whereas other glucose-lowering drugs are not.
So, for sure, they have systemic effects in addition to their glucose-lowering properties. This is well explained in these recent overviews:
Actually, I’ve just found this paper which may negate the above I’ve just said ![]()
Meanwhile, a retrospective cohort study conducted in Taiwan showed consistent results with our findings with 12,681 new users of dapagliflozin or empagliflozin, i.e., similar risks of composite cardiovascular outcomes and a significantly lower risk of heart failure in dapagliflozin users [36]. Cardiovascular death in this Taiwanese study was also lower in the dapagliflozin group (HR 0.54, 95% CI 0.14–2.12). […] it is intriguing to note that significant differences between users of dapagliflozin and empagliflozin were observed only for these two outcomes. This may allude to intrinsic disparities between the two drugs and could lead us to posit that dapagliflozin may exert more pronounced pleiotropic effects on heart failure outcomes than empagliflozin. For example, different neurohormonal responses might be one of the possible mechanisms. A previous study revealed that empagliflozin significantly increased plasma aldosterone and noradrenaline levels; however, dapagliflozin did not. It was also noted that the change in plasma volume is a key mediator in reducing cardiovascular death among users of SGLT2 inhibitors. Taken together, different neurohormonal responses and the concomitant reductions in plasma volume might synergistically contribute to the further decrease in the risk of heart failure-related events and cardiovascular death in dapagliflozin users. On the other hand, neurohormonal responses may not affect ischemic endpoints such as MI or ischemic stroke, as SGLT2 inhibitors have been found to be independent of pathways governing arterial thrombosis. This is further supported by the pronounced advantages observed in women. Specifically, in our subsequent analysis, the cardiovascular benefits were evident only in women > 50 years. Although individual menopausal status could not be noted, women > 50 years, who were mostly in their peri- or post-menopausal stage and, hence, more susceptible to changes in neurohormones and plasma volume, would have benefited more from dapagliflozin and showed improved cardiovascular outcomes. Secondly, the approximate 2.5-fold greater affinity for SGLT2 and six-fold greater affinity for SGLT1 exhibited by dapagliflozin compared to empagliflozin might have contributed. Currently, the benefits of adding SGLT1 to SGLT2 inhibition are receiving attention. A study with Mendelian randomization data revealed that patients with missense mutations in the SGLT1 gene had reduced risks of heart failure and death. Recent clinical trials, SOLOIST (effect of sotagliflozin on cardiovascular events in patients with type 2 diabetes post worsening heart failure) and SCORED (effect of sotagliflozin on cardiovascular and renal events in patients with type 2 diabetes and moderate renal impairment who are at cardiovascular risk), also raised the possible advantage of additional SGLT1 inhibition for cardiovascular outcomes. Accordingly, the higher SGLT1 and SGLT2 affinity of dapagliflozin compared to that of empagliflozin might contribute to the lower risks of heart failure-related events and cardiovascular death in our study. In addition, several studies have suggested that the SGLT2-independent effects of this drug class, which are presumed to take place in the myocardium, are likely attributed to off-target effects, given the notably low levels of SGLT2 in cardiac cells. Further investigations focusing on differences in off-target effects between dapagliflozin and empagliflozin are needed.
So I still think that dapa and empa are better than cana. But maybe sotagliflozin does SGLT1 inhibition “better” than cana and is even better than all others. Sotagliflozin was only approved in the US in 2023. So it will take time to have good data on sotagliflozin vs cana, dapa, and empa… So far the only comparison we have is this clinical trial of empa vs sota for 8 weeks: identical results except after breakfast where sota is more potent (better glucose, insulin, GIP, and GLP-1 AUCs): Metabolic, Intestinal, and Cardiovascular Effects of Sotagliflozin Compared With Empagliflozin in Patients With Type 2 Diabetes: A Randomized, Double-Blind Study
I don’t mind if cana is better for heart disease since that can already be prevented with statins etc. I don’t tend to pay much attention to heart disease for that reason. Possible better mood with dapa is a big plus, and as well if it’s better in other ways.
It makes sense that SGLT2i’s increase risk of UTI’s, since the sugar is dumped in urine.
Is this saying that both dapag and empag have sglt1 effects? And that dapag is stronger for both SLGT2 and sglt1?
I thought only canag and sotag had sglt1 effects.
I don’t understand either, but I assume nothing is black or white:
Here’s another paper we already cited previously: “At approved doses, canagliflozin, but not dapagliflozin or empagliflozin, inhibits renal SGLT1, which may reconcile the differences in clinical efficacy and safety among gliflozins. […] At approved doses, SGLT1 inhibition by canagliflozin but not dapagliflozin or empagliflozin contributed to ~ 10% of daily urinary glucose excretion.” (Differentiating the Sodium‐Glucose Cotransporter 1 Inhibition Capacity of Canagliflozin vs. Dapagliflozin and Empagliflozin Using Quantitative Systems Pharmacology Modeling )