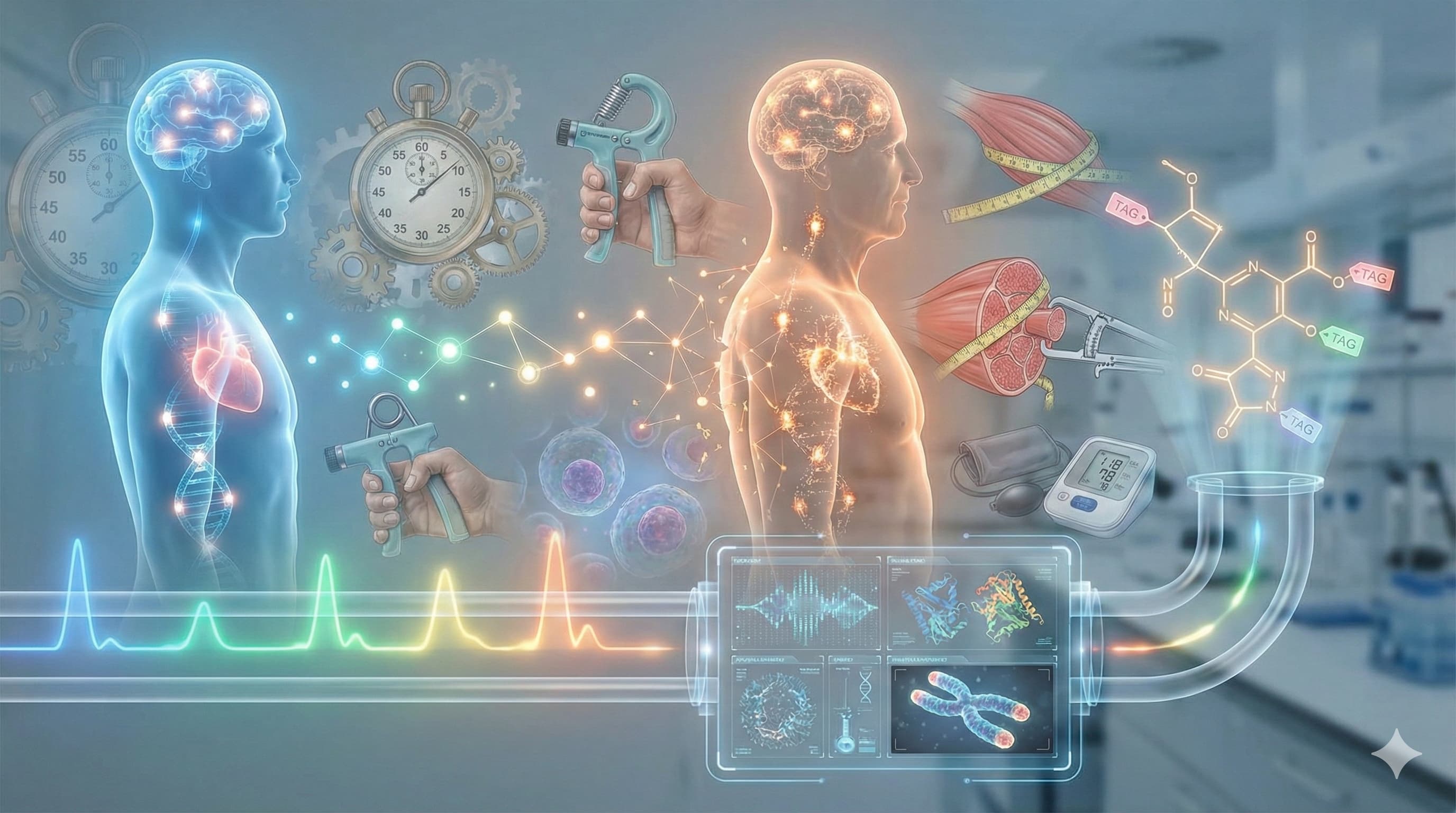
In an important move for the longevity field, a global consortium of experts has published a consensus statement defining the essential “biomarkers of aging” for human intervention studies. For years, the biotech and biohacking communities have suffered from a “Tower of Babel” problem—every study uses different yardsticks (telomeres, methylation, frailty indices), making it impossible to compare the efficacy of rapamycin against metformin, or sauna protocols against caloric restriction. This paper, published in the Journals of Gerontology: Series A, solves that by using a rigorous Delphi consensus method to identify the 14 most reliable, validated markers of biological age.
The important development here is standardization. The experts moved beyond hype-driven metrics (like commercial telomere length tests, which failed to make the cut) and settled on a robust mix of functional, physiological, and molecular markers. The consensus prioritizes markers that are not just theoretically interesting but are responsive to interventions, mechanically plausible, and clinically feasible. For the biohacker and investor, this list is the new “shopping list” for validation: if your protocol or portfolio company isn’t moving these needles, it likely isn’t slowing aging. The inclusion of GDF-15 and DNA Methylation clocks alongside classic functional tests like Grip Strength signals a maturity in the field—merging high-tech omics with the undeniable reality of physical function.
Context:
- Institution: Multi-institutional consensus (Lead authors from Newcastle University, UK; University of Manchester, UK; and others globally).
- Country: International (UK, USA, Portugal, Japan, etc.).
-
Journal Name: The Journals of Gerontology: Series A (Biological Sciences and Medical Sciences).
Source Material: An Expert Consensus Statement on Biomarkers of Aging for Use in Intervention Studies
Impact Evaluation: The impact score of this journal is 3.8 (JIF 2024), evaluated against a typical high-end range of 0–60+ for top general science. Therefore, this is a Medium impact journal in the broader scientific landscape, but considered Elite/Tier-1 specifically within the niche of aging biology and gerontology.
The Biohacker Analysis
Study Design Specifications
- Type: Delphi Consensus Study (Expert Panel Decision-Making). Not an In Vivo/Clinical Trial.
- Subjects: Expert Panel of researchers and clinicians (n=Unknown from snippet, typically 20-50 experts in Delphi studies) spanning diverse disciplines (biology, geriatrics, epidemiology).
- Lifespan Data: N/A. The output is a consensus agreement (70-98%) on specific biomarkers.
Mechanistic Deep Dive & The Consensus List
The following report details the mechanistic rationale for the 14 consensus biomarkers identified in the Perri et al. (2025) study.
The expert panel selected these biomarkers not just for their ability to predict death, but because they serve as readable outputs for specific Hallmarks of Aging. The consensus divides broadly into Molecular Signals(upstream causes) and Functional/Phenotypic Outputs (downstream consequences).
I. The Molecular & Systemic Panel (Upstream Drivers)
These markers monitor the “Engine Room”—the cellular and biochemical processes driving the rate of aging.
1. GDF-15 (Growth Differentiation Factor 15)
-
Mechanistic Rationale: Mitochondrial Dysfunction & Integrated Stress Response (ISR).
- GDF-15 is a mitokine secreted by cells under stress. It is arguably the most sensitive blood-based signal for mitochondrial distress and “somatic” (body-wide) cellular injury. It rises with age and correlates with the burden of senescent cells.
- Biohacker Note: It is the “Check Engine” light for your mitochondria.
2. IGF-1 (Insulin-like Growth Factor 1)
-
Mechanistic Rationale: Deregulated Nutrient Sensing.
- IGF-1 is the primary output of the Growth Hormone/IIS axis. It represents the body’s decision to prioritize Growth/Reproduction over Maintenance/Repair. Lower levels (within a physiological range) are associated with extended lifespan in model organisms (downregulating mTOR), while very low levels in humans predict frailty (sarcopenia).
3. DNA Methylation (Epigenetic Clocks)
-
Mechanistic Rationale: Epigenetic Alterations.
- These clocks measure the accumulation of methyl groups on CpG islands in DNA, effectively tracking “entropy” in gene regulation. They are currently the best proxy for the Pace of Aging—measuring how fast the biological clock is ticking relative to chronological time.
4. IL-6 (Interleukin-6)
-
Mechanistic Rationale: Cellular Senescence & SASP.
- IL-6 is a primary cytokine in the Senescence-Associated Secretory Phenotype (SASP). Senescent (“zombie”) cells secrete IL-6 to alert the immune system, but in aging, this becomes chronic, damaging surrounding healthy tissue and driving sterile inflammation.
5. hsCRP (High-Sensitivity C-Reactive Protein)
-
Mechanistic Rationale: Chronic Inflammation (“Inflammaging”).
- While IL-6 is the signal, CRP is the systemic response produced by the liver. It quantifies the overall inflammatory load on the vascular and metabolic systems. Elevated CRP is a direct driver of endothelial dysfunction and accelerates biological aging.
II. The Functional & Phenotypic Panel (Downstream Consequences)
These markers monitor the “Chassis”—the structural integrity and functional capacity of the body.
6. Hand Grip Strength
-
Mechanistic Rationale: Loss of Proteostasis & Neuromuscular Integrity.
- Grip strength is not just about hand muscles; it is a validated proxy for overall neural drive and total body protein reserves. It correlates strictly with telomere length and all-cause mortality. It tests the ability of the nervous system to recruit motor units (Neuromuscular Junction health).
7. Muscle Strength (General)
-
Mechanistic Rationale: Sarcopenia & Stem Cell Exhaustion.
- Measures the functional output of muscle tissue. Decline indicates a failure in satellite cell proliferation (stem cell exhaustion) and mitochondrial bioenergetics within the muscle fibers.
8. Muscle Mass
-
Mechanistic Rationale: Metabolic Reserve.
- Skeletal muscle is the primary “sink” for glucose and a reservoir of amino acids for the immune system. Loss of mass (sarcopenia) leads to insulin resistance (Deregulated Nutrient Sensing) and frailty.
9. Gait Speed
-
Mechanistic Rationale: Integrative System Failure.
- Walking requires the precise coordination of the visual, vestibular, proprioceptive, and musculoskeletal systems. A slowed gait indicates “systemic entropy”—the degradation of neural processing speed and energy availability. It is widely termed the “6th Vital Sign” in geriatrics.
10. Timed-Up-and-Go (TUG)
-
Mechanistic Rationale: Dynamic Stability & Power.
- This tests “explosive” power (getting out of the chair) and agility (turning). It reveals deficits in fast-twitch muscle fibers (Type II), which atrophy first during aging.
11. Standing Balance Test
-
Mechanistic Rationale: Neurodegeneration & Vestibular Decline.
- The ability to balance on one leg degrades rapidly with age due to loss of proprioceptive nerve fibers and cerebellar processing speed. It is a direct functional readout of neural aging.
12. Blood Pressure
-
Mechanistic Rationale: Vascular Stiffness & Endothelial Dysfunction.
- As arteries age, they lose elastin and accumulate collagen/calcium (stiffness). Systolic pressure rises as the vessels can no longer expand to accommodate blood flow, directly damaging the brain and kidneys (microvascular damage).
13. Cognitive Health
-
Mechanistic Rationale: Neuroinflammation & Synaptic Plasticity.
- Measures the functional output of the brain. Decline signals neurodegeneration, often driven by vascular aging and systemic inflammation crossing the blood-brain barrier.
14. Frailty Index
-
Mechanistic Rationale: Accumulation of Deficits.
- Aging is the accumulation of damage. The Frailty Index quantifies this by counting deficits (e.g., hearing loss, tremor, exhaustion). It mathematically models the “tipping point” where the organism loses the redundancy required to maintain homeostasis.
Novelty
The novelty lies in the exclusion and ranking.
- What’s In: GDF-15 is officially mainstreamed as a top-tier aging biomarker, validating what niche researchers have said for years.
- What’s Out: Telomere length is notably absent from the top consensus list, reflecting the growing view that it is too variable and poor at predicting individual intervention success compared to epigenetic clocks.
- Harmonization: This provides the first “ISO standard” for longevity trials, allowing us to finally compare apples to apples across different biotech startups.
Critical Limitations
- Consensus, not = Truth: A Delphi study reflects current opinion, not necessarily biological truth. If the experts are collectively wrong (e.g., overvaluing a popular clock that turns out to be noisy), the consensus preserves that error.
- Cost vs. Access: While “Grip Strength” is free, reliable DNA methylation and GDF-15 testing remain expensive and hard to access for the average consumer, limiting “Citizen Science” applicability.
- Lack of “Response” Data: The study identifies what to measure, but does not yet provide the definitive “Unit of Change” (e.g., how much does GDF-15 need to drop to equal 1 extra year of life?).