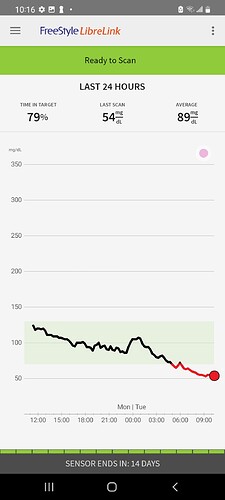
That’s good to hear! I mean, I’m kinda pissed that the Libre 2 is so inaccurate and that I spent $200 and got all freaked out about being insulin resistant, but overall relieved that I’m actually insulin sensitive. Maybe the Libre 3 (whenever it’s available) will allow for calibration.
You don’t understand how it would be dangerous because you don’t understand medicine. Peter Attia is measures his parameters. I don’t understand your point. Rapamycin + SGLT2 can unmask beta cell dysfunction and drive insulin lower- fact.
It’s clear you do not have a background in science or medicine. You should not be referencing subjective experience. It has no validity here.
Consider your hypothesis of the insulin model grossly inaccurate.
Fasting has been higher last 2 days (dropped to 70s today) but I haven’t stress tested it with anything other than small boxes of raspberries/blackberries (neither which increased my BG to an appreciable extent). I’ve been surviving on thinslim breads for the last few days whihc aren’t supposed to increase BG but did (but only to a max of 115 which is fine). No need for SGLT2 inhibitors while I still have my thinslim breads on me.
I can get a glucose testing strip for calibration but I’ve often had difficulty consistently drawing enough blood to get into the glucose monitor.
Wow, way to go, very professional, making unfounded (and completely incorrect) personal attacks on what is normally a group with no trolls. Congrats on dragging it into the gutter.
I don’t mind being wrong if/when I’m wrong. In fact, if it is dangerous to take SGLT2 inhibitors with rapamycin, then I’m the first who wants to know.
Please provide some sources on this. We try to be data driven here. I’ve not seen any data suggesting that SGLT-2 inhibitors will drive insulin down dangerously low, independently of food consumption, glucose absorption delay…
My understanding, from the Peter Attia / Richard Miller podcast and related papers:
SGLT2 inhibitors
- Canagliflozin is in the class of drugs known as SGLT2 inhibitors
- SGLT2 inhibitors has been around for a while and is used pretty readily in patients with type 2 diabetes as it blocks the re-uptake of glucose so that more glucose is excreted in the urine
- It affects the process in the kidney that deals with very high glucose levels without having much scope for causing toxicity
Perhaps he’s referring to this phenomenon (euglycemic diabetic ketoacidosis) which occurs with extreme rarity in diabetic patients taking SGLT2 inhibitors:
[SGLT2 Inhibitor–Induced Euglycemic Diabetic Ketoacidosis: A Case Report - Kidney Medicine]
https://www.kidneymedicinejournal.org/article/S2590-0595(20)30031-5/fulltext
I saw this paper a couple of months ago and was initially concerned until I read the full text. The rare cases of euglycemic ketoacidosis have turned up mostly in patients using SGLT2i off-label for type 1 diabetes (dangerous since they can’t shut down ketosis without insulin) or in type 2 diabetics who have either progressed to the point of extremely low insulin secretion or who are undergoing major trauma/surgery, infection and/or decreased food/fluid intake.
Euglycemic ketoacidosis is rapidly reversible with fluids, carbs and insulin. Since non-diabetics can secrete our own insulin, my take-home message was to make sure I stay hydrated and to stop the SGLT2i if I get sick or with any major metabolic challenges (and to make extra sure to stay hyrated/fed during those states, since the effects of the SGLT2i appear to last up to 10 days after stopping!). I could also see a potential problem if taking SGLT2i while doing an extended fast or fasting-mimicking protocol, with or without rapamycin on board.
Now if rapamycin were a potent and rapid inhibitor of insulin secretion at the doses typically used for anti-aging purposes (thus mimicking a type 1 diabetic taking SGLT2i), then I could see a real potential problem here.
But is it? It seems hard to quantify in the papers I’ve read so far in human subjects. It definitely can suppress insulin production, but is this only in high doses and/or chronic rather than intermittent use in humans? That’s what Blagosklonny seems to suggest (requires chronic high doses):
[Fasting and rapamycin: diabetes versus benevolent glucose intolerance | Cell Death & Disease nature.com)](Fasting and rapamycin: diabetes versus benevolent glucose intolerance | Cell Death & Disease
They say 50% of electronic messages are misunderstood- in which case I’m sorry for responding as such.
I posted with the intention of helping someone with poor responses to carbohydrates and I took your post as an unscientific argument rather than a scientific debate or discussion. I can clearly see that you were not arguing rather than questioning my thoughts.
Again, sorry for the negative-context response.
Thanks for clarifying. I truly do want to know your thoughts on rapa+SGLT2 inhibitors and why you consider them dangerous. Is it the euglycemic ketoacidosis I mentioned above?
That’s exactly right and we don’t have sufficient published case studies only clinician experience unfortunately.
In aging, the ratio of proinsulin (immature protein) to insulin decreases, first-phase insulin decreases, fasting insulin or insulin produced the wrong times increases etc.- in general glucose regulation which is governed by a complex system tends to become more dysfunctional. The pancreas is vulnerable to internal and external environmental factors and more on topic, beta cells require homeostasis to regulate mTOR to produce the mature form of insulin. Intermittent doses of rapamycin are powerful at suppressing mTOR1 and that makes the beta cell extremely vulnerable. In the presence of rapamycin physiological functions requiring minute amounts of mTOR1 are hindered rather than suppressed; again variable.
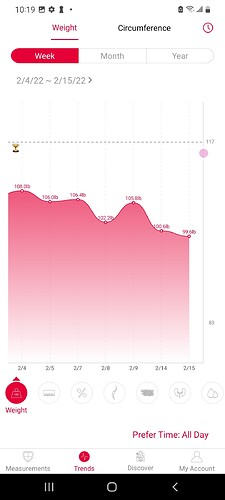
For large populations, I hypothesis intermittent doses of rapamycin will lead to positive outcomes for healthspan indication, but for some it will drive insulin to low and still have a positive outcomes even though it’s a undesired result. An example is “[InquilineKea]” seen in this thread, although they may consider a strict ketogenic to mitigate elevated post-prandial glucose responses, his response to glucose is not of a healthy response and we can hypothesis insulin involvement based on what’s probable. Suggesting or hinting SGLT2 alongside ketogenic diet, in this case could be very irresponsible without first checking for a pulse.
What we see with clinician experience is a decrease in insulin for most people to a varying degree, some significantly raising blood sugar which is unmasking beta cell dysfunction. Furthermore, an unstudied polypill of rapamycin and SGLT2 in populations that are not being monitored could be dangerous. Combined, there is an increased risk or incidence with the addition of canagliflozin, specifically, which has greater concerns than other SGLT2 on the topic of insulin and DKA just from the study of pharmacology alone. We don’t have any studies determining the safety and efficacy of intermittent rapamycin dosing regime in healthy populations and we certainly do not have any combining SGLT2 and rapamycin in large populations indicated for healthspan. My point is if the outcome accounted for 5% of the populations using the combination, which I believe is probable, that is a large number of reports and the combination should be monitored which many are not doing.
On your reference of Blagosklonny, he hypothesizes that the decrease in insulin and change in energy metabolism is a variable in improved outcomes, which I agree. He does not suggest canagliflozin for many reasons.
Note that DKA onset can be within 24 hours and can be severe. As you mentioned very low-risk for canagliflozin only. Besides DKA, consider consistently, moderately elevated ketones and/or fatty acids a risk for long-term healthspan.
Thanks for the detailed response. So to recap, you are recommending against the combination because of the potential side effects, specifically risk of acute ketoacidosis, chronic moderate ketosis and/or elevated fatty acids. What if one were to check urinary ketones each morning for a week or two, including the 2-3 days after a weekly/biweekly rapa dose while also taking an SGLT2i? If there are no ketones or minimal ketones, would that be reassuring? Also, regularly monitoring lipids (which anyone taking rapa should be doing anyway). Would that check the main boxes for playing it safe (or at least more safe), in your opinion? Any other suggestions for monitoring while taking the combo? Thanks!
BTW the higher my blood glucose gets, the worse the discrepancy between the CGM and glucometer. I ate a Trader Joe’s veggie pizza just to push my metabolic limits (980 kcal, 136g carbs) about 90 minutes ago. Glucometer shows 130 which is what I’d expect for nondiabetic and fit person taking empagliflozin 12.5 mg QD, but CGM shows 169(!!!). I don’t know how this CGM ever got approved (and this is my 2nd Freestyle Libre 2).
When I’ve gone into Labcorp they’ve commented that my blood flow isn’t so great (from the perspective of filling up the test-tube quickly). They recommended I drink more water in the morning before my test. That recommendation might be helpful for you also for your at-home finger prick testing.
Ugh, after a several day break, I finally put on the CGM again. And… after overnight… it started out at 120 (this was after a night when I dined on 2 lbs strawberries, vegan queso, and lots of cole slaw - so it must have been higher for many hours). I took a break from SGLT2 inhibitors too, but now I had to take them. AGH I thought I solved my issues.
Will get more SGLT2 inhibitors in the mail tomorrow so I won’t feel scarce with them.
Also taking Adderall NOW today so I can make fasting SO much easier (ugh I feel fully functional but it took several hours to kick in)
Have you factored your Adderall into your blood glucose readings?
My second Freestyle Libre 2 stopped working after 6 days, so they’re sending me a new one. Given how inaccurate they’ve been compared to my glucometer, I’m not sure if I’m even going to apply this one.
InquilineKea, do you have a glucometer and have you used it alongside your Freestyle? Mine was maybe 10-15 points higher then glucometer at fasting, but the farther away from baseline the less accurate (30-40 points too high after high glycemic loads, also 20+ points lower after exercise compared with glucometer!)
Alex, your weight is only approx. 100lbs? Wow - if thats accurate (and not just your left leg) you’re going to live forever…
Have you practiced CR in the past?

I took extremely high dose melatonin - like 60 to 80 mg altogether… apparently this REALLY affects insulin…
https://www.nature.com/articles/1002103
^maybe this is why all the nut binges early January caused my blood pressure elevation? This is why I need to not go on so many nut binges again. Sometimes, eating 4-5 lbs of raw vegetables is not satiating enough. Maybe this means I just need to add more olive oil to them (olive oil is not as addicting as nuts are)…
Why would you take 80mg of melatonin?