This was very good. I didn’t expect the research to be so solid.
Dr. Hood is partnering with the Buck Institute:
“I am delighted to welcome Dr. Hood to the Buck family as our Chief Innovation Officer and Distinguished Professor. The opportunity to form a Center with Lee Hood and his Phenome Health team will be transformational for the Buck,” said Dr. Verdin. “We believe combining the novel computational and human characterization engine of Phenome Health with the Buck’s expertise in geroscience, the biology of aging, has the power to redefine how we age and treat—or prevent altogether—the chronic diseases of aging.”
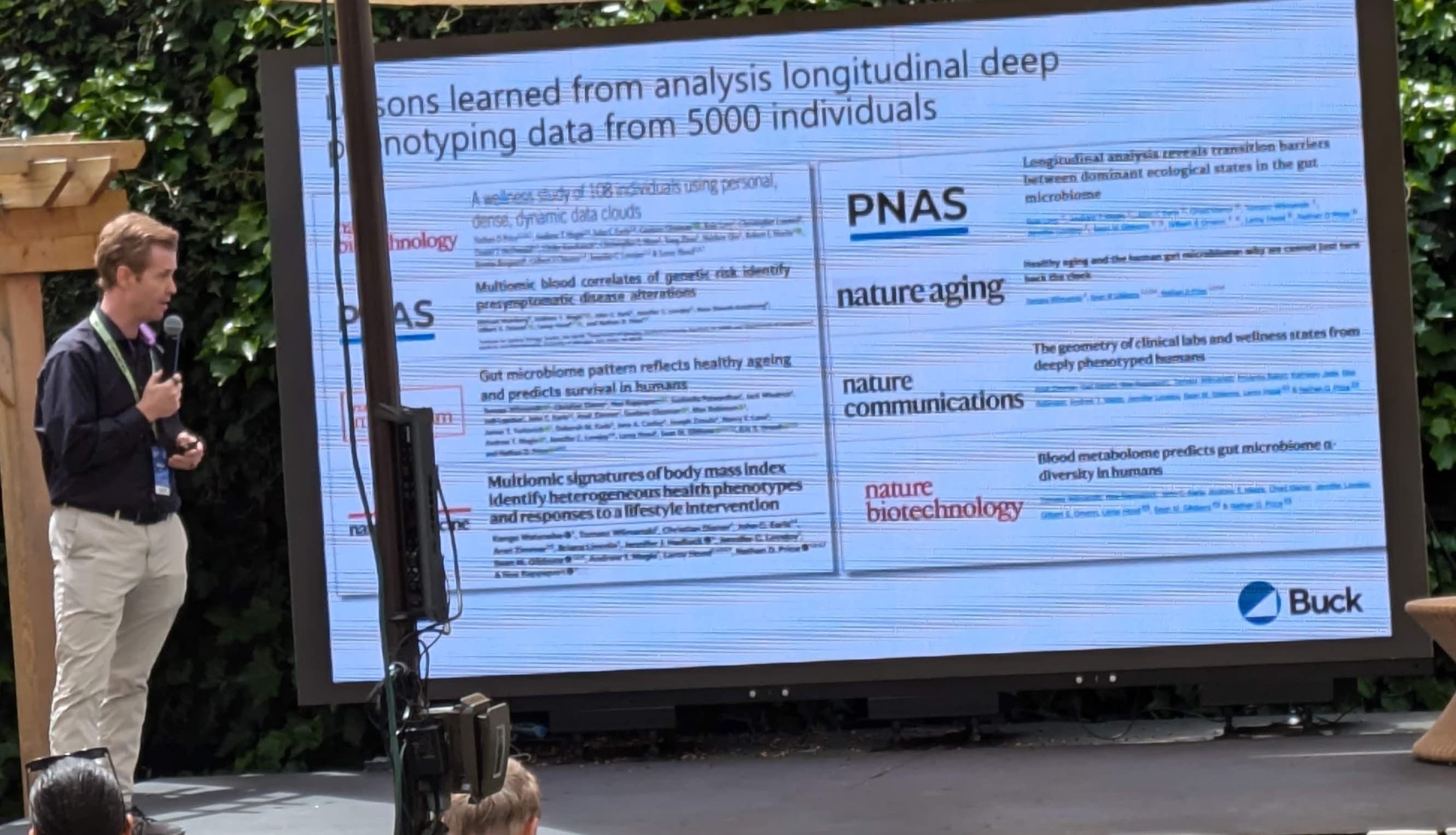
Phenome Health’s platform combines whole-genome sequencing with phenomic data, including social determinants of health, electronic health records, self-tracking data from wearables and self-assessments, cognitive and psychiatric brain assessments, and clinical samples of the blood, saliva, and microbiome. Using next-generation AI, the team integrates these data to understand the biology of aging, its associated diseases and interventions targeting the aging process. The Center will be the nexus for these two distinguished research partners to advance healthspan for everyone. “I could not be more delighted to enter into this partnership with the Buck,” said Dr. Hood. “The Center is uniquely positioned to translate data into understanding healthy aging, ushering in scientific wellness and ultimately extending each individual’s healthspan.”
What does phenome health do? The website looks interesting but I couldn’t find anything I could do.
I need a personal physician that does happy hour. I’ll get by with the book.
But seriously, this all still comes back to money, insurance companies, and a broken health care system at a time when a recession looms.
And, btw, I love that this is in “Popular Mechanics “.
a broken health care system at a time when a recession looms.
I think that something have to be working at some time to be broken. Things that may not work as well as we want may still work as well as they ever did & if they aren’t working worse than they ever did, I would not call them broken.
This is the the way people talk, where the literal sense of the phrase & what is meant aren’t actually the same. I feel that calling it broken isn’t too helpful, because it has a lot of overtones of judgement instead of acknowledging that it’s a work in progress.
Yes, this is a pet peeve of mine. Yes, the system could work better & hopefully, we’ll figure out ways to make that happen. Glasses, fullness & all that … at least we aren’t still bleeding people to death, there has been progress.
On the one hand, we have had arguably some of the best health care available to those who can afford it.
It is amazing that, when the chips are down, how many wealthy people including the Saudis, etc. choose to fly to the U.S. for anything really serious. I also observed this during the 7 years I spent in Europe. In spite of the “Wonderful European Model” people who could afford it tended to head to the U.S. for anything serious.
On the other hand, our system has been rampant with doctors being bought by tobacco and big pharma, etc. Real doctors extolled the merits of particular cigarette brands. Some of us are old enough to remember going to the doctor’s office and getting free samples of drugs on the way out. Doctors have been paid to prescribe certain medications and brands. I don’t know how rampant this is now, but it was pretty common in the past.
So, yes, IMO the healthcare system in the U.S. has been broken for quite some time.
The problem with the US healthcare system is that you need insurance or you are SOL. Insurance even with Medicare isn’t cheap either.
Here in Hong Kong, many people rely on public healthcare because they don’t have insurance. In the US, without insurance you can choose bankruptcy or death. Not a very nice choice to make.
Where is this notion that American healthcare is better?? Maybe it is just more capitalistic and are willing to take on patients who are willing to pay. And if you are seriously ill, you are scared and scare people are easier to open their wallets.
And in reality, I cite a friend oncologist, the American healthcare is better for 1 maybe 2 percent of patient that would profit from treatments outside guidelines.
Nowhere did I say the U.S. healthcare system is better. What I do believe is that we have a preponderance of the world’s best doctors. The main problem in the U.S. is access to the system and incentivized fraud.
MHO, the main problem with medicine, in this country or any other, is the lack of real solutions to many of the problems people have.
A lot of people have chronic health issues & by definition, chronic health issues are ones for which medicine doesn’t have a solution. If it didn’t, the problem would be solved, not chronic.
I think that the main thing medicine needs to improve is a lot of research. Research really does find solutions & the solutions can be made available to people. It doesn’t do any good to have access to health care if the health care can’t solve their problems. They still have the problem, they just go see doctors about it, who don’t help – not because they don’t care, but because they don’t have help to give.
“A lot of people have chronic health issues & by definition, chronic health issues are ones for which medicine doesn’t have a solution”
I would disagree. Most of those chronic diseases are treatable and preventable with lifestyle changes. We as a society have just chosen to ignore diet and exercise.
Its education not research thats needed. Doctors can’t help much as they aren’t given time for education, patients have roadblocks to exercise and good diet.
Yes, true… certainly a large percentage:
A third approach is to estimate the percentage of disease that is potentially preventable by reducing multiple behavioral risk factors using prospective cohort studies. Among U.S. adults, more than 90 percent of type 2 diabetes, 80 percent of CAD, 70 percent of stroke, and 70 percent of colon cancer are potentially preventable by a combination of nonsmoking, avoidance of overweight, moderate physical activity, healthy diet, and moderate alcohol consumption (Willett 2002).
In my mountaineering days, we used to talk about not dying of stupidity. The unfortunate truth is most people die too young from some combination of stupidity, stubbornness, and bad luck.
Stolen from Twitter
“When you are dead, you don’t know you are dead. It’s pain only for others.
It’s the same thing when you are stupid.”
What point, that everyone doesn’t know, are you trying to make?
And education starts with children.
I have been exercising in an open air “fitness area” and sometimes some school children would come by with physical ed. teacher trying to get them to exercise.
I am always shocked how unfit they are and how many are overweight. I was checking statistics on overweight children and it is horrible. In some areas the number reaches 50-70%. And an overweight child has more chances to become an overweight metabolically unhealthy adult…
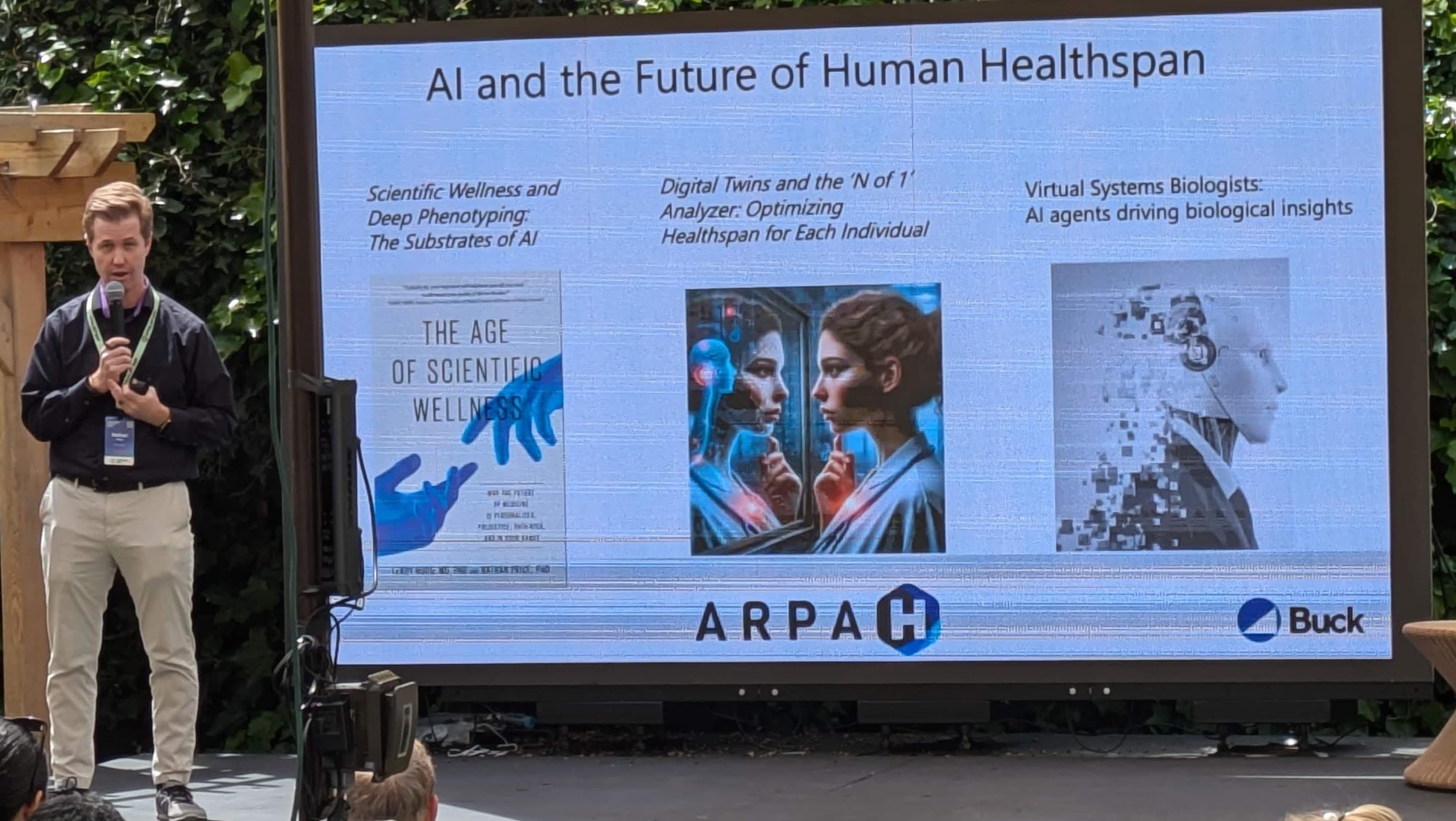
I finally got around to reading The Age of Scientific Wellness. It aligned perfectly with what I have been imagining as the ideal approach to healthcare based on endless consumption of The Drive and this website.
Does anybody know where this has gone? I see that Nathan Price is affiliated with Thorne and the Buck Institute. Has anybody on here interacted with these guys or kept track of what they’re up to these days?
I saw him at the Vitalist Bay conference in May in Berkeley. He’s still at the Buck. Working on the same stuff. I have the book but haven’t read it yet. Did you find there were any actionable insights from it?
No actionable insights from the book. This is what interests me most: You have the obvious advice to exercise more, get more sleep, eat well, have community, etc. If we had urban design and economy organized properly, this would be as passive as access to clean water. But in our country, at this time, we need to actively choose our priorities.
Your primary care doctor isn’t going to pay attention to anything until you have a complaint, and then it had better fit into a disease. According to the book, Nathan and Lee had success prospectively in disease avoidance interventions with some of their study participants (who had iron issues from hemochromatosis) and success retrospectively in identifying signs of disease long before the traditional system discovered it (where they found evidence (after the diagnosis) of cancer emerging in a blood sample taken two years prior to the diagnosis).
I am sympathetic to their view that we need massive machine learning so we have a digital twin to tell each of us what we individually should prioritize. The book was inspiring, and I think any benefit downstream of the book will be from practitioners inspired by it, not from specific insights anybody on this forum would pull from it.
Here is the WSJ article by Nathan Price and Lee Hood, covering their perspective:
The AI Will See You Now
As medical research produces ever more data on health and disease, doctors are turning to artificial intelligence to help them make the best decisions for patients.
By Lee Hood and Nathan Price, April 7, 2023 9:58 am ET
By virtue of their medical training, doctors have a wealth of knowledge, experience, wisdom and judgment. Yet even the greatest of human brains can’t remember or interpret a tiny fraction of the information now available on human health and disease. Just a few years ago, most medical decisions were based entirely on the knowledge in the head of the doctor at the time the decision was made. Today that is beginning to change, thanks to the rapid development of artificial intelligence.
The evolution that brought the world ChatGPT and similar large language models is making AI one of the most quickly adopted technologies in history, promising profound changes for the way we live and work. Some of the most important will take place in the field of healthcare. As the technology behind these systems progresses, AI will soon be as much a part of our healthcare experience as doctors, nurses, waiting rooms and pharmacies. In fact, it won’t be long before AI has mostly replaced or redefined all of these.
A host of AI “decision support systems” are already helping to give physicians access to a wealth of information at the point of care. These systems leverage what computers are naturally good at—storing, recalling and correlating vast amounts of information virtually instantaneously—and link it to the ability of a human expert to reason intuitively and think creatively.
When early so-called “expert systems” were first being developed in the 1980s and 1990s, they were met with hostility by many physicians who worried that computers would soon be in charge of medical decision-making, taking the “doctor’s touch” out of the equation and binding the hands of physicians whose opinions differed from the computer’s analysis. But that’s not what happened. Research has shown that these systems have gotten better and better at helping doctors spot potential outcomes that they might have missed, without taking the ultimate decision-making authority out of their hands.
We are fast approaching an age of ‘centaur doctors,’ combining the best parts of human intelligence and AI assistance.
Read the full story: The AI Will See You Now (WSJ)