Is the response to antihypertensive drugs heterogeneous? Rationale for personalized approach 2024
The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019, which estimated the proportion of mortality, years of life lost, and years of life lived with disability attributable to 87 behavioural, environmental, occupational, and metabolic risk factors, highlighted how the predominant share of deaths in the world is attributable to systolic BP values ≥ 110–115 mmHg with an estimate of 10.8 million avoidable deaths every year and 235 million years of life lost or lived with disability every year.
Furthermore, the combination of drugs that act on different mechanisms involved in the rise in BP values reduces the variability of the BP response to treatment and allows for a faster BP response to be obtained than that which can be obtained with increasing doses of a single drug and it is safe and well tolerated with a modest risk of hypotensive episodes, even when prescribed to patients with grade 1 hypertension.
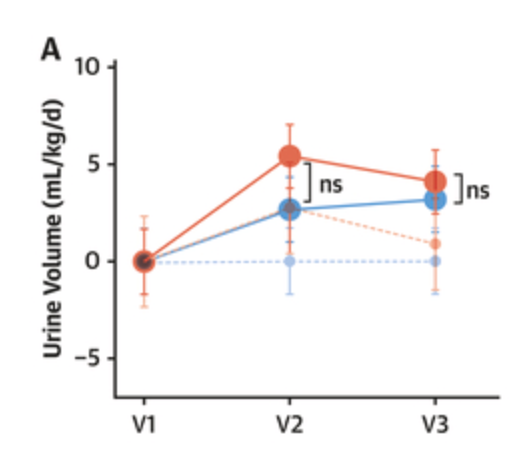
The finding of a substantial heterogeneity in the individual response to the different treatments used in the PHYSYC study suggests the possibility of obtaining additional advantages with a personalization of the treatment, but in the current state of knowledge, this eventuality still appears rather theoretical, especially due to the difficulties in making personalized choices. Following the approach used in the PHYSIC study, one could hypothesize testing the patient’s individual response to a series of short periods of treatment before defining long-term therapy with one or more drugs, but this approach appears quite laborious.
Theoretically, it would be simpler to identify phenotypic characteristics that can predict a satisfactory response to a drug or a combination of drugs. Indeed, beyond the long-known modest sensitivity of black hypertensive patients to treatment with ACE-I, the limited availability to date of phenotypic indicators of response to a drug makes this approach difficult to pursue.
The progressive digitalization of healthcare systems is making enormous quantities of data available for machine learning systems which will allow the derivation of management algorithms for truly personalized antihypertensive therapy in the near future.
In the meantime, I guess the best approach is trial and error and/or a low-dose combination of the best-in-class agents (so telmisartan, amlodipine, indapamide SR, and bisoprolol?).
Provisionally accepted paper, we don’t have the full text yet: Association between types of antihypertensive medication and the risk of atrial fibrillation: A nationwide population study 2024
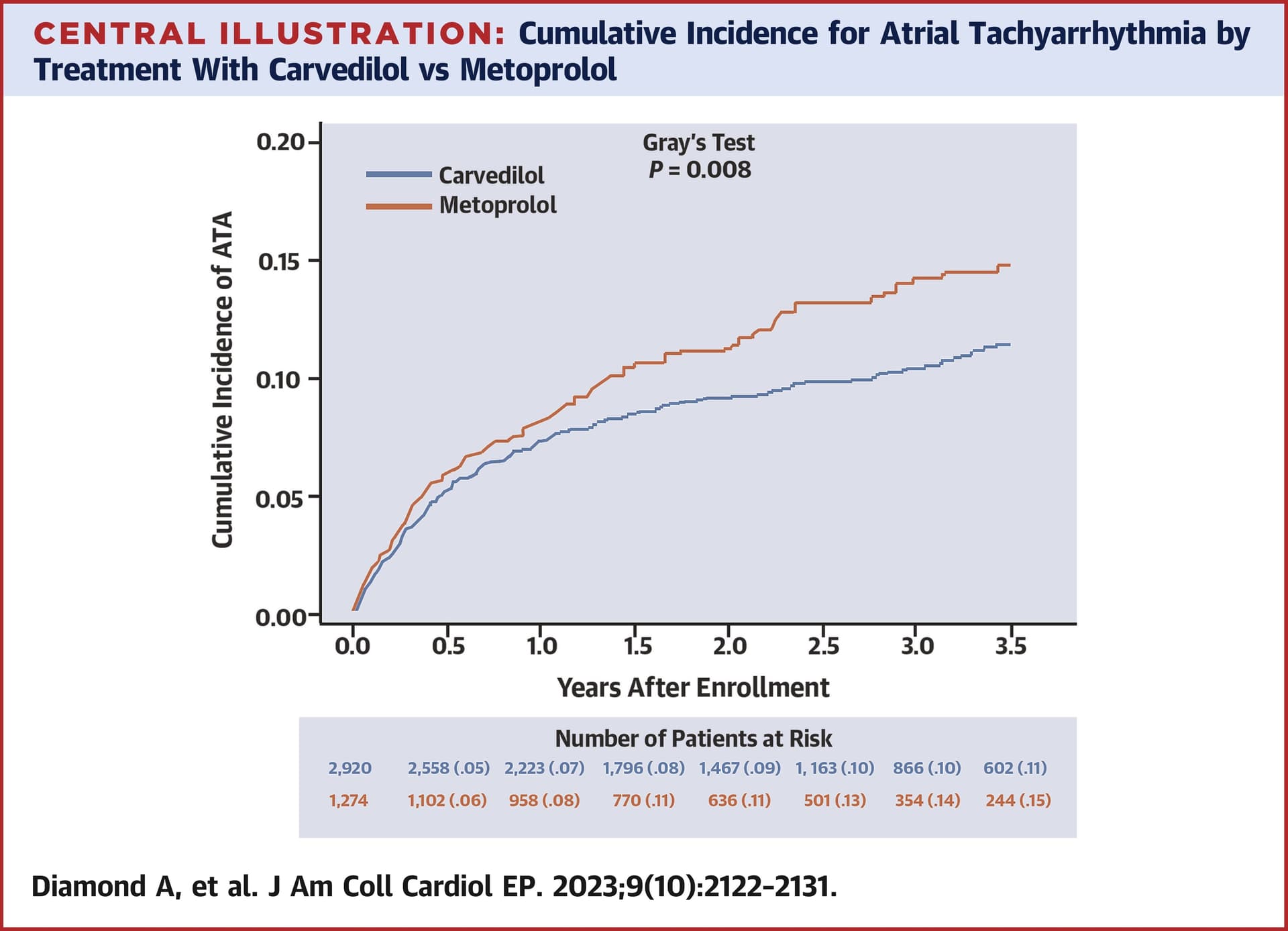
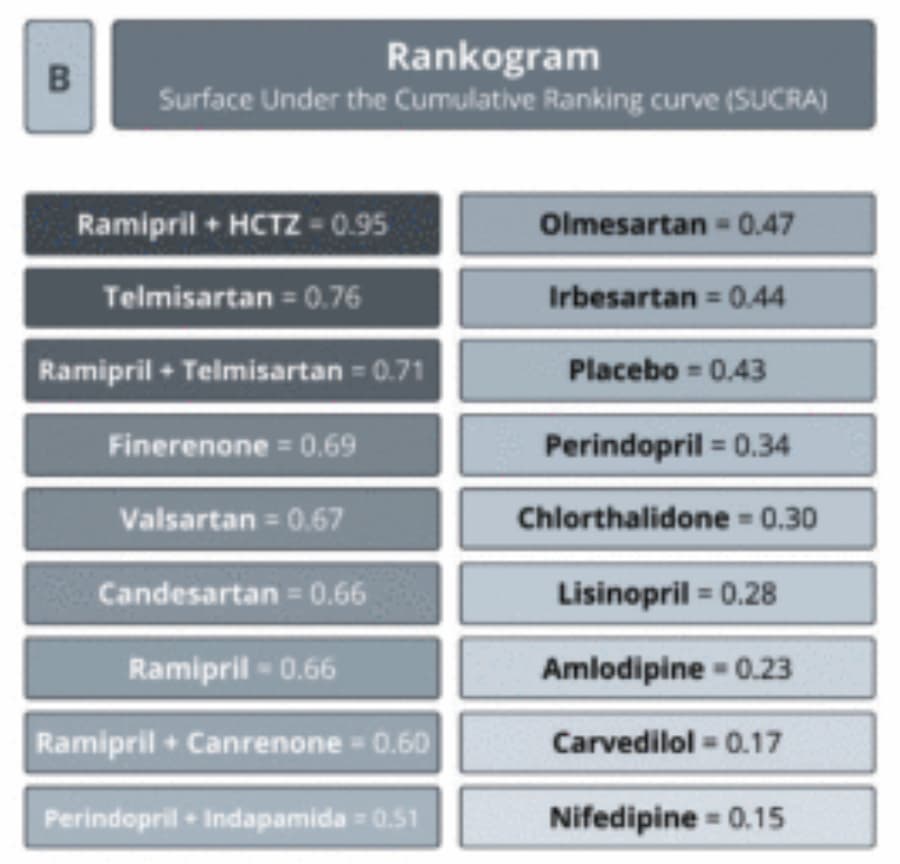
In monotherapy, ACEi and CCB had similar AF risks as ARB, while beta-blockers and diuretics showed higher AF risks than ARB. In combination therapy, ARBs/CCBs and ARBs/diuretics had the lowest AF risk, whereas ARBs/beta-blockers had the highest compared to ARB/CCB. Among the specific ARBs, the AF risk varied insignificantly, except for telmisartan and candesartan. In hypertensive patients receiving monotherapy, ACEi and CCB showed a similar AF risk as ARBs, while beta-blockers and diuretics were associated with a higher risk.Among those receiving combination therapy, ARBs/CCBs and ARBs/diuretics had the lowest AF risk, whereas ARBs/beta-blockers showed the highest risk. Various types of ARBs have different associations with AF risk.