@scta123 What Rapa dose have you been taking?
5-6mg weekly until September and since September I am taking daily 1mg for 3 weeks and I have one week off. Amount of rapamycin is same, just the schedule is different. I will have new tests at the end of February to see if new schedule observational benefits translate to biomarkers. (Last quick blood test was done in december)
I’m looking forward to hearing about your new and improved numbers!
It is helpful to have people trying different dosing schemes. Personally I would not want to try this sort of approach, but it helps to develop knowledge of what the impact might be. This is where multiple N=1 is a good way of dealing with things.
I had the same schedule for immunosuppression. It accumulated quickly (1 week was too short of a break for me) and gave me side effects (mouth sores, red spots on skin, dry patches on shoulders, elevated glucose and lipids). Had to reduce the dose.
I don’t have any side effects that I would notice. I just checked my lipids in December (I decided to test lipids every 3 months) and they were fine, other markers I will test in March (6 months into this regimen). I had some acne some two months into regimen for few weeks. But that resolved on it’s own. And it was just an odd pimple here and there. It felt like I am entering puberty. Otherwise my skin is much better, almost no signs of my seborrheic dermatitis and dyshidrosis completely gone. If markers will be worse than before I will probably just do 14 days 1mg and 14 days off. Or go back to 6mg weekly.
It could be that your reaction to that dose is better than mine because your body weight is bigger than mine. So per kg of body weight you take less Rapa. I’m only 49.8 kg.
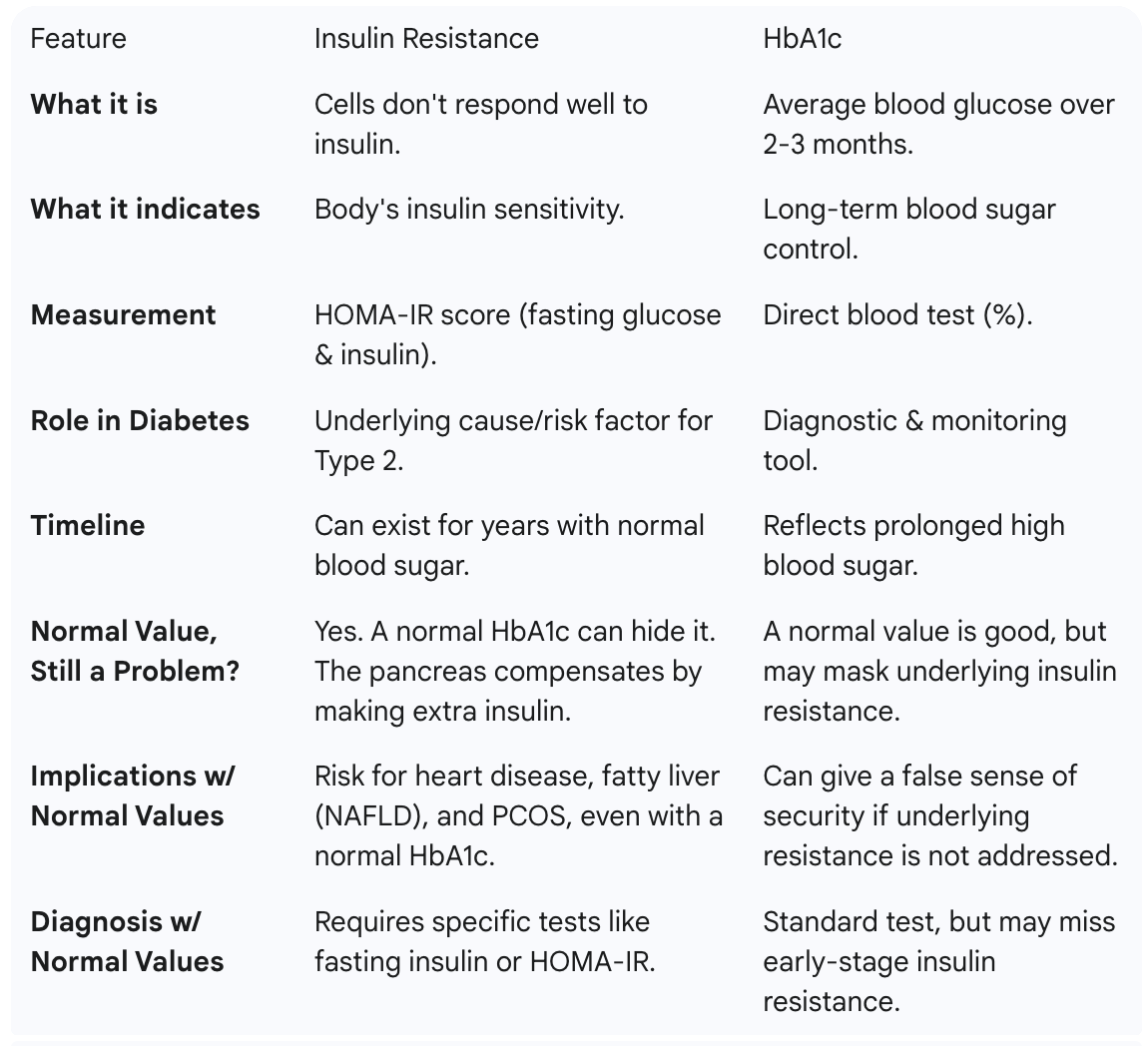
I retested after not taking rapamycin for 5 weeks. Hb A1C dropped back to 5.7 after rising to 6.0 on rapamycin. I believe the 5.7 level is a result of taking rosusvastatin 5 mg qd for 18 months. Insulin resistance lowered dramatically from 10.7 down to 6 off of the rapa. Prior to starting rapa, my insulin was 6.4. Glucose dropped to 88 from 93. This equates to a HOMA-IR score of 1.3, a dramatic decrease from 2.46 recorded after 3 months of rapamycin 6 mg po once weekly. Testosterone result was stable at 658 as was my lipid panel of LDL 64, Triglycerides 77 & HDL 45. Various other contributors to this site have commented on being “strong responders”. I interpret this to mean that a ‘normal’ dose of 6 mg of rapamycin led them into much more pronounced mTORC 2 inhibition with concomitant negative effects. I believe this to be my case ( I am a very healthy 86 kg, frequent exerciser). I have also read that apparently more people are deciding on an every other week dosing regimen to allow for complete washout. My plan is to restart the rapamycin at 4 mg every other week and then retest in 3 months to evaluate mTORC 2 inhibition with the goal to slowly increase the dosage back to 6 mg every other week. Would appreciate any comments/observations/opinions. Thxs. 03.03.24
What is the current consensus on rapamycin and insulin resistance? Has any of you followed your insulin levels with tests such as C-Peptide and Insulin Random, both of which can be elevated with normal HbA1c and normal glucose levels?
Here is the summary by Grok about the discussion above so far (not checked):
- Initial Report: A physician reported taking 12 mg of sirolimus every two weeks (0.2 mg/kg) for 9 months with no other lifestyle changes.
- Lab Results: HOMA-IR doubled from 0.9 to 1.9, and fasting insulin levels also doubled, indicating increased insulin resistance.
- Testosterone Drop: A decline in testosterone levels was reported, though specific pre/post values were not detailed.
- Insulin Resistance Mechanism: Rapamycin may cause insulin resistance by disrupting the mTORC2 pathway, which is separate from longevity benefits.
- Biphasic Effect: Rapamycin might initially improve insulin sensitivity but lead to resistance with chronic use.
- Testosterone Effects: Some evidence suggests rapamycin lowers testosterone, supported by anecdotal reports and social media discussions (e.g., Ben Bikman).
- Mixed Study Findings: Animal studies show rapamycin can elevate testosterone in PCOS models but may worsen reproductive issues and insulin resistance.
- Male Mice Studies: Chronic rapamycin use in male mice induces diabetes-like symptoms (glucose intolerance, insulin resistance), with less focus on testosterone.
- Consensus on Risks: Insulin resistance and testosterone changes are potential risks of higher-dose, long-term rapamycin use for longevity.
- Mitigation Strategies: Effects may be reversible, dose-dependent, or mitigated by cycling rapamycin, exercise, or metformin.
- Data Needs: More user data and studies are needed due to individual variability in side effects.
- Monitoring Tools: Users shared tools like HOMA-IR calculators for self-monitoring insulin resistance.
- Testosterone Replacement Concerns: Combining rapamycin with testosterone replacement may lead to interactions that reduce benefits.
From my N=1, my insulin sensitivity is exceptional after 2 years of weekly use of at least 10 mg equivalent (3 mg + GFJ + EVOO). (sometimes at very high doses - 21 mg equivalent 7 mg + GFJ + EVOO)
My fasting insulin:
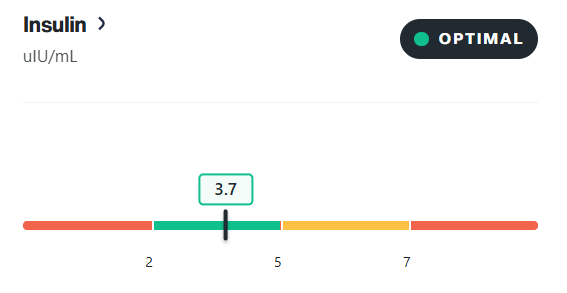
I had recent lab tests back and my A1C is down to 4.9 after it was 5.5 about 5 months ago. This is all while being on 5mg Rapamycin per week and lowering Rosuvastatin from 5mg to 2.5mg daily. 3mg Retatrutide, 10mg Empagliflozin, and 200mg Acarbose are the drugs I am taking to lower it.
So basically, my Rapamycin use is being offset as far as insulin resistance goes.
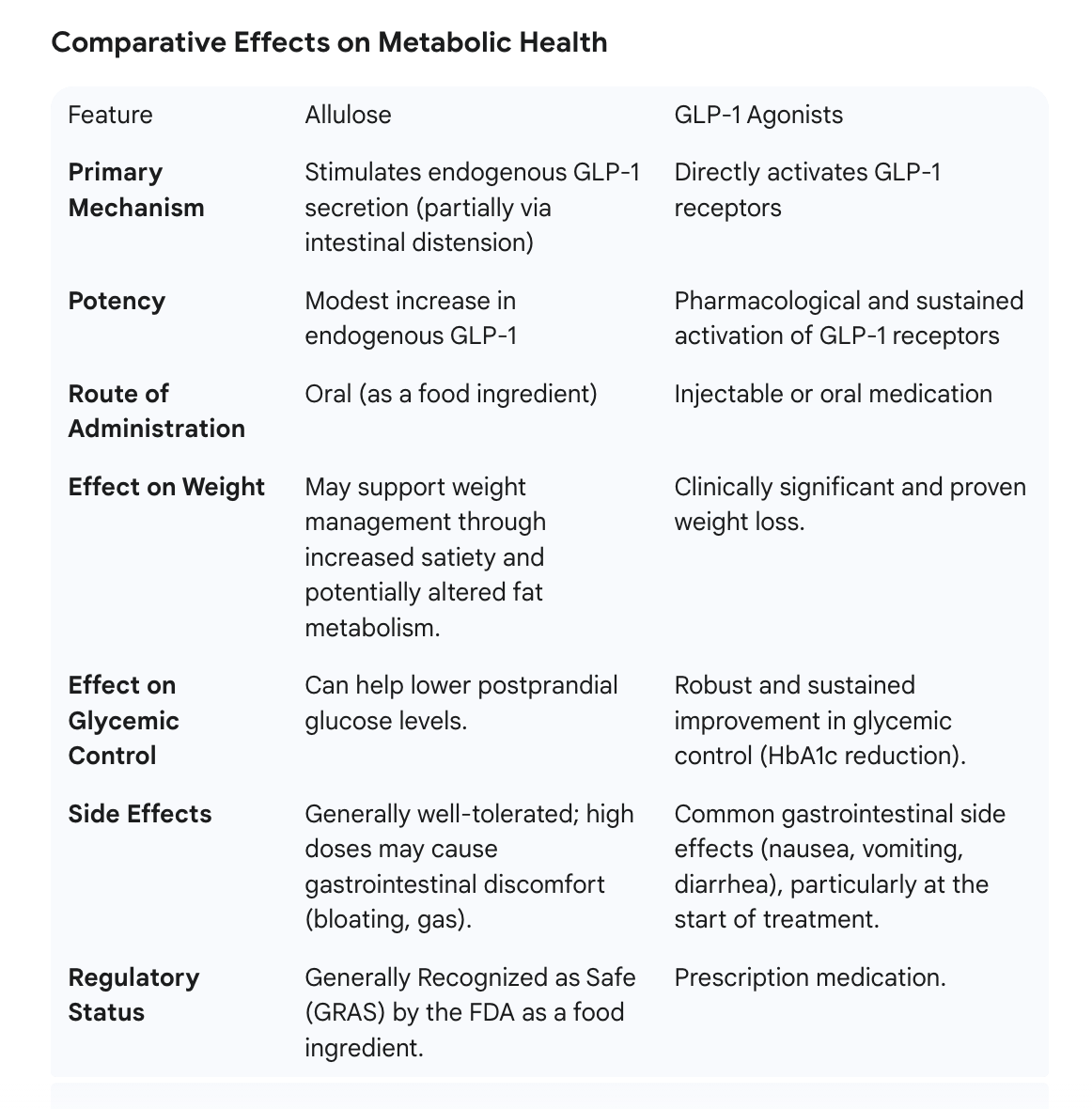
GLP1 agonists are very powerful insulin sensitizers so Reta alone could probably account for it.
Bingo. Since I was already on the other things before so all I did was cut rosuvastatin in half to 2.5mg and continue Reta (3mg per week divided MWF).
My A1C 5.5 bothers me, but iam resistant to take Reta. Iam very slim(BMI 20,6)…
I posted this elsewhere a while back but copying it here
I did a baseline IGF-1 prior to starting weekly Rapamycin. It was 74. After six months of weekly regimen, the IGF-1 went upto 115!
A1c(5.1), Lipids etc remain same. Omega index remains horribly low ( not that Rapa has anything to do with it; just my vegetarian diet). Can’t seem to figure out the IGF-1 trend though!
Yes, my testosterone levels did drop. Levels were drawn at the trough of Rapa. In other words immediately prior to weekly dosing.
Here is a link to the discussion of how IGF-1 and longevity have a U-curve association:
For people that use say daily sirolimus for organ transplant, Im guessing they need something strong like pioglitazone to control insulin resistance. For weekly dose it shouldnt affect much but if it does adding an extra day between dosing (once every 8 days instead of 7) might be all that is needed
My IGF-1 is high as well, although I never attributed it to Rapamycin. I would assume that Rapamycin would counter any negatives from high IGF-1 through MTOR1 inhibition.
Has anyone on CGM tried Allulose?
Metabolic Link Podcast – Allulose Episode (2024 Metabolic Health Summit Panel)
I. Show Introduction
-
Host: Dom D’Agostino, Ph.D.
-
Theme: Metabolism as the common thread in health & disease.
II. Episode Focus: Allulose
-
Rare release of full 2024 Summit panel discussion.
-
Goal: translate latest science → real-world metabolic-health tools.
III. Expert Panel
-
Richard Johnson, MD – Professor of Medicine, Univ. Colorado.
-
Jeff Volek, Ph.D., RD – Professor Human Sciences, Ohio State.
-
Ben Bikman, Ph.D. – Professor Cell Biology, BYU.
-
Andrew Koutnik, Ph.D. – Research Scientist, Samson Diabetes Research Institute.
-
Dominic D’Agostino, Ph.D. – Assoc. Prof. Pharmacology & Physiology, Univ. South Florida.
IV. Key Science Points Discussed
-
Glycemic impact: 0-5 g allulose blunts post-prandial glucose & insulin excursions.
-
Insulin sensitivity: acute & chronic improvements in clamp & CGM studies.
-
Weight management: ↓ energy intake via early satiety signals; animal data show ↓ fat mass.
-
GLP-1 pathway: dose-dependent secretion → delayed gastric emptying, enhanced insulin release.
-
Fructose comparison: minimal hepatic metabolism → low uric-acid & lipogenesis risk.
-
Safety profile: FDA GRAS; ≤ 0.66 g/kg/day GI tolerance in adults.
A normal HbA1c is a positive indicator, but it does not rule out the presence of insulin resistance.
Yes, and it doesn’t spike blood glucose. In my readings, it often decreased glucose levels. It’s my sugar additive of choice.